Abstract
Purpose
Data on the benefit of stereotactic body radiation therapy (SBRT) in patients with breast cancer (BC) and bone metastases remain limited. The purpose of this study is to report our 10-year experience of bone SBRT, analyzing toxicity and prognostic factors for local control (LC); progression-free survival, and overall survival (OS).
Methods/patients
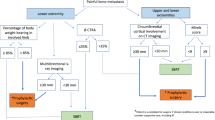
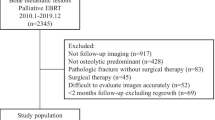
We analyzed all spine and non-spine bone SBRT performed in patients with BC during the 2012–2022 period at our institution. Treatments carried out with ablative intent in stereotactic conditions with dose/fraction ≥ 5 Gy in 5 or fewer sessions were considered. Demographic, treatment, and toxicity data were recorded according to CTCAEv4. Risk factors were assessed through univariate and multivariate analysis by Cox regression.
Results
60 bone SBRT treatments were performed during the study period. 75% were spine SBRT and 25% were non-spine SBRT (median BED4Gy was 80 Gy4). The median age was 52.5 years (34–79). The median tumor volume was 2.9 cm3 (0.5–39.4). The median follow-up was 32.4 months (1.2–101.7). 1 and 2 years LC were 92.9 and 86.6%, respectively. 1 and 2 years OS were 100 and 90.6%, respectively. Multivariate analysis (MVA) associated volume of the treated lesion ≥ 13 cm3 with worse LC (p = 0.046; HR 12.1, 95%CI = 1.1–140.3). In addition, deferring SBRT > 3 months after lesion diagnosis to prioritize systemic treatment showed a significant benefit, improving the 2 years LC up to 96.8% vs. 67.5% for SBRT performed before this period (p = 0.031; HR 0.1, 95%CI = 0.01–0.8). Hormonal receptors, the total number of metastases, and CA15-3 value were significantly associated with OS in MVA. During follow-up, three non-spine fractures (5%) were observed.
Conclusions
According to our data, bone SBRT is a safe and effective technique for BC. Upfront systemic treatment before SBRT offers a benefit in LC. Therefore, SBRT should be considered after prior systemic treatment in this population.


Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Data code
All data and materials as well as the software application or custom code support their published claims and comply with field standards.
References
Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M. Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2017;26(6):809–15.
Lüftner D, Lorusso V, Duran I, Hechmati G, Garzon-Rodriguez C, Ashcroft J, et al. Health resource utilization associated with skeletal-related events in patients with advanced breast cancer: results from a prospective, multinational observational study. Springerplus. 2014;3:328.
Gobbini E, Ezzalfani M, Dieras V, Bachelot T, Brain E, Debled M, et al. Time trends of overall survival among metastatic breast cancer patients in the real-life ESME cohort. Eur J Cancer. 2018;96:17–24.
Fietz T, Tesch H, Rauh J, Boller E, Kruggel L, Jänicke M, et al. Palliative systemic therapy and overall survival of 1,395 patients with advanced breast cancer—results from the prospective German TMK cohort study. Breast. 2017;34:122–30.
Strauss JB, Chmura SJ. Oligometastatic breast cancer. Semin Radiat Oncol. 2022;32(3):282–90.
Koleva-Kolarova RG, Oktora MP, Robijn AL, Greuter MJW, Reyners AKL, Buskens E, et al. Increased life expectancy as a result of non-hormonal targeted therapies for HER2 or hormone receptor positive metastatic breast cancer: a systematic review and meta-analysis. Cancer Treat Rev. 2017;55:16–25.
Viani GA, Gouveia AG, Louie AV, Korzeniowski M, Pavoni JF, Hamamura AC, et al. Stereotactic body radiotherapy to treat breast cancer oligometastases: a systematic review with meta-analysis. Radiother Oncol. 2021;164:245–50.
Pagani O, Senkus E, Wood W, Colleoni M, Cufer T, Kyriakides S, et al. International guidelines for management of metastatic breast cancer: can metastatic breast cancer be cured? J Natl Cancer Inst. 2010;102(7):456–63.
Harrow S, Palma DA, Olson R, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic radiation for the comprehensive treatment of oligometastases (SABR-COMET)—extended long-term outcomes. Int J Radiat Oncol Biol Phys. 2022;S0360–3016(22):00412–6.
Katipally RR, Pitroda SP, Juloori A, Chmura SJ, Weichselbaum RR. The oligometastatic spectrum in the era of improved detection and modern systemic therapy. Nat Rev Clin Oncol. 2022;19(9):1–15.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31(12):1623–49.
Wong AC, Watson SP, Pitroda SP, Son CH, Das LC, Stack ME, et al. Clinical and molecular markers of long-term survival after oligometastasis-directed stereotactic body radiotherapy (SBRT). Cancer. 2016;122(14):2242–50.
Pérez-Montero H, Godino O, Lozano A, Asiáin L, Martínez I, Sánchez JJ, et al. Long-term outcomes of spinal SBRT. Is it important to select the treatment time? Clin Transl Oncol. 2021. https://doi.org/10.1007/s12094-021-02684-9.
Milano MT, Katz AW, Zhang H, Huggins CF, Aujla KS, Okunieff P. Oligometastatic breast cancer treated with hypofractionated stereotactic radiotherapy: some patients survive longer than a decade. Radiother Oncol. 2019;131:45–51.
Stewart R, White M, Tan J, Siva S, Karroum L, David S. SABR in oligometastatic breast cancer: current status and future directions. Breast. 2021;60:223–9.
Weykamp F, König L, Seidensaal K, Forster T, Hoegen P, Akbaba S, et al. Extracranial stereotactic body radiotherapy in oligometastatic or oligoprogressive breast cancer. Front Oncol. 2020;10:987.
Bonet M, García V, Farré N, Algara M, Farrús B, Fernandez J, et al. Radiation therapy for bone-only metastases in breast cancer patients: a GOCO survey of current clinical practice. Rep Pract Oncol Radiother. 2020;25(1):113–6.
Yoo GS, Yu JI, Park W, Huh SJ, Choi DH. Prognostic factors in breast cancer with extracranial oligometastases and the appropriate role of radiation therapy. Radiat Oncol J. 2015;33(4):301–9.
Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–66.
Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European society for radiotherapy and oncology and European organisation for research and treatment of cancer consensus recommendation. Lancet Oncol. 2020;21(1):e18-28.
Krug D, Vonthein R, Illen A, Olbrich D, Barkhausen J, Richter J, et al. Metastases-directed radiotherapy in addition to standard systemic therapy in patients with oligometastatic breast cancer: study protocol for a randomized controlled multi-national and multi-center clinical trial (OLIGOMA). Clin Transl Radiat Oncol. 2021;28:90–6.
Lopez-Campos F, Cacicedo J, Couñago F, García R, Leaman-Alcibar O, Navarro-Martin A, et al. SEOR SBRT-SG stereotactic body radiation therapy consensus guidelines for non-spine bone metastasis. Clin Transl Oncol. 2022;24(2):215–26.
Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, et al. International spine radiosurgery consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2012;83(5):e597-605.
Dunne EM, Sahgal A, Lo SS, Bergman A, Kosztyla R, Dea N, et al. International consensus recommendations for target volume delineation specific to sacral metastases and spinal stereotactic body radiation therapy (SBRT). Radiother Oncol. 2020;145:21–9.
Nguyen T, Chin L, Sahgal A, Dagan R, Eppinga W, Guckenberger M, et al. International consensus contouring recommendations for stereotactic body radiotherapy of non-spine bone metastases. Int J Radiat Oncol Biol Phys. 2020;108(3):S90.
Soltys SG, Grimm J, Milano MT, Xue J, Sahgal A, Yorke E, et al. Stereotactic body radiation therapy for spinal metastases: tumor control probability analyses and recommended reporting standards. Int J Radiat Oncol Biol Phys. 2021;110(1):112–23.
Yamada Y, Katsoulakis E, Laufer I, Lovelock M, Barzilai O, McLaughlin LA, et al. The impact of histology and delivered dose on local control of spinal metastases treated with stereotactic radiosurgery. Neurosurg Focus. 2017;42(1):E6.
Alomran R, White M, Bruce M, Bressel M, Roache S, Karroum L, et al. Stereotactic radiotherapy for oligoprogressive ER-positive breast cancer (AVATAR). BMC Cancer. 2021;21(1):303.
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0 Published: May 28, 2009 (v4.03: June 14, 2010). U.S. Department of Health and Human Services. National Institutes of Health National Cancer Institute.
Kucharczyk MJ, Parpia S, Walker-Dilks C, Banfield L, Swaminath A. Ablative therapies in metastatic breast cancer: a systematic review. Breast Cancer Res Treat. 2017;164(1):13–25.
Milano MT, Zhang H, Metcalfe SK, Muhs AG, Okunieff P. Oligometastatic breast cancer treated with curative-intent stereotactic body radiation therapy. Breast Cancer Res Treat. 2009;115(3):601–8.
David S, Tan J, Savas P, Bressel M, Kelly D, Foroudi F, et al. Stereotactic ablative body radiotherapy (SABR) for bone only oligometastatic breast cancer: a prospective clinical trial. Breast. 2020;49:55–62.
Li MP, Kelly D, Tan J, Siva S, Kron T, David S. Single-fraction stereotactic ablative body radiotherapy for sternal metastases in oligometastatic breast cancer: technique and single institution experience. J Med Imaging Radiat Oncol. 2020;64(4):580–5.
Gomez DR, Tang C, Zhang J, Blumenschein GR, Hernandez M, Lee JJ, et al. Local consolidative therapy Vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II randomized study. J Clin Oncol. 2019;37(18):1558–65.
Iyengar P, Wardak Z, Gerber DE, Tumati V, Ahn C, Hughes RS, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2018;4(1):e173501.
Soran A, Ozmen V, Ozbas S, Karanlik H, Muslumanoglu M, Igci A, et al. Randomized trial comparing resection of primary tumor with no surgery in stage IV breast cancer at presentation: protocol MF07-01. Ann Surg Oncol. 2018;25(11):3141–9.
Khan SA, Zhao F, Goldstein LJ, Cella D, Basik M, Golshan M, et al. Early local therapy for the primary site in de novo stage IV breast cancer: results of a randomized clinical trial (E2108). JCO. 2022;40(9):978–87.
Chmura SJ, Winter KA, Woodward WA, Borges VF, Salama JK, Al-Hallaq HA, et al. NRG-BR002: a phase IIR/III trial of standard of care systemic therapy with or without stereotactic body radiotherapy (SBRT) and/or surgical resection (SR) for newly oligometastatic breast cancer (NCT02364557). JCO. 2022;40(16):1007–1007.
Nguyen AT, Shiao SL, McArthur HL. Advances in combining radiation and immunotherapy in breast cancer. Clin Breast Cancer. 2021;21(2):143–52.
Qu XM, Chen Y, Zaric GS, Senan S, Olson RA, Harrow S, et al. Is SABR cost-effective in oligometastatic cancer? an economic analysis of the SABR-COMET randomized trial. Int J Radiat Oncol Biol Phys. 2021;109(5):1176–84.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
HP-M, AL and AN-M: contributed to the study conception and design. Data collection, analysis, and interpretation were performed by HP-M and AN-M. HP-M, AN-M, AL, RB, JJS, ML, EM, MG-G, CF, AG-T, SP, OG and MJP: are physicians or medical physicists who contributed in the treatment and/or follow-up of the cases. The first draft of the manuscript was written by HP-M and AN-M. All authors revised critically and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Miguel Gil-Gil has received personal fees from Pfizer, Daiichi Sankyo, Novartis, Gilead, AstraZeneca, and Roche. These fees are not related to this study. The rest of the authors have no relevant financial or non-financial interests to disclose. The authors alone are responsible for the content and writing of the paper.
Ethics approval
All procedures were performed under the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval for this study was granted by the Ethics Committee of Hospital Universitari de Bellvitge (15.06.2021/PR224/21).
Consent to participate
For this type of study, formal consent is not required. The patients did not receive any specific informed consent as data were collected from a retrospective review of electronic medical records. The patients signed the informed consent for the usual procedure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pérez-Montero, H., Lozano, A., de Blas, R. et al. Ten-year experience of bone SBRT in breast cancer: analysis of predictive factors of effectiveness. Clin Transl Oncol 25, 1756–1766 (2023). https://doi.org/10.1007/s12094-023-03073-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03073-0