Abstract
Aims
Acute kidney injury (AKI) remains a frequent complication after cardiac interventions, such as left atrial appendage closure (LAAC), yet limited data are available on the incidence and clinical implication of AKI in this setting. We sought to assess incidence, predictors and relevance of AKI after LAAC.
Methods and results
We retrospectively analyzed 95 LAAC patients in three European centers. AKI was defined according to the Acute Kidney Injury Network (AKIN) classification. The incidence of AKI was 13.7% with mild AKI in 92.3% and AKI stage > II in 7.7%. Total contrast volume was not linked to the occurrence of AKI (AKI: 127 ± 83 vs. no AKI: 109 ± 92 ml, p = 0.41), however increasing contrast volume (CV) to glomerular filtration rate (GFR) ratio (CV/GFR ratio) was associated with an increased risk of AKI (OR, per unit increase: 1.24, 95% CI 0.97–1.58, p = 0.08). ROC-analysis revealed a moderate predictive value of CV/GFR ratio for the prediction of AKI (AUC: 0.67, 95% CI 0.50–0.84, p = 0.05). Furthermore, AKI was associated with significantly increased mortality 6 months and 1 year after LAAC. No significant difference in the incidence of AKI was observed between patients with mere fluoroscopic and additional echocardiographic guidance (16.3% vs. 11.5%, p = 0.56).
Conclusion
Whereas mild AKI is common in patients after LAAC, severe AKI is rare. AKI after LAAC is associated with poor baseline renal function, increased doses of contrast (CV/GFR ratio) and impaired outcome. Future studies will be needed to elaborate the benefit of reducing or avoiding contrast volume regarding this endpoint.
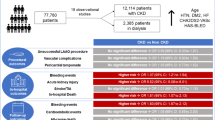
Graphic abstract




Similar content being viewed by others
Abbreviations
- ACP:
-
Amplatzer Cardiac Plug
- AF:
-
Atrial fibrillation
- AKI:
-
Acute kidney injury
- AKIN:
-
Acute Kidney Injury Network
- AUC:
-
Area under the curve
- CHA2DS2-VASC:
-
CHA2DS2-VASC-Score
- CI:
-
Confidence interval
- CV:
-
Contrast volume
- CV/GFR ratio:
-
Contrast volume to glomerular filtration rate ratio
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- HAS-BLED:
-
HAS-BLED-score
- KDIGO:
-
Kidney disease improving global outcomes
- LAAC:
-
Left atrial appendage closure
- LVEF:
-
Left ventricular ejection fraction
- OAC:
-
Oral anticoagulation
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- TAVR:
-
Transcatheter aortic valve replacement
- TEE:
-
Transesophageal echocardiography
References
Reddy VY, Holmes D, Doshi SK et al (2011) Safety of percutaneous left atrial appendage closure: results from the watchman left atrial appendage system for embolic protection in patients with AF (PROTECT AF) clinical trial and the continued access registry. Circulation 123:417–424. https://doi.org/10.1161/CIRCULATIONAHA.110.976449
Tzikas A, Shakir S, Gafoor S et al (2016) Left atrial appendage occlusion for stroke prevention in atrial fibrillation: multicentre experience with the AMPLATZER Cardiac Plug. EuroIntervention 11:1170–1179. https://doi.org/10.4244/EIJY15M01
Holmes DR, Kar S, Price MJ et al (2014) Prospective randomized evaluation of the watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol 64:1–12. https://doi.org/10.1016/j.jacc.2014.04.029
D’Ancona G, Safak E, Ince H (2019) Left atrial appendage occlusion in patients with atrial fibrillation and high risk of fall: a clinical dilemma or a budgetary issue? Clin Res Cardiol. https://doi.org/10.1007/s00392-019-01476-0
Seeger J, Bothner C, Dahme T et al (2016) Efficacy and safety of percutaneous left atrial appendage closure to prevent thromboembolic events in atrial fibrillation patients with high stroke and bleeding risk. Clin Res Cardiol 105:225–229. https://doi.org/10.1007/s00392-015-0910-8
Gupta RK, Bang TJ (2010) Prevention of contrast-induced nephropathy (CIN) in interventional radiology practice. Semin Intervent Radiol 27:348–359. https://doi.org/10.1055/s-0030-1267860
McCullough PA, Wolyn R, Rocher LL et al (1997) Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med 103:368–375. https://doi.org/10.1016/S0002-9343(97)00150-2
Hatakeyama Y, Horino T, Nagata K et al (2018) Transition from acute kidney injury to chronic kidney disease: a single-centre cohort study. Clin Exp Nephrol. https://doi.org/10.1007/s10157-018-1571-5
Kellum J, Lameire N, Aspelin P et al (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138. https://doi.org/10.1038/kisup.2012.7
Nombela-Franco L, Rodés-Cabau J, Cruz-Gonzalez I et al (2018) Incidence, predictors, and prognostic value of acute kidney injury among patients undergoing left atrial appendage closure. JACC Cardiovasc Interv 11:1074–1083. https://doi.org/10.1016/j.jcin.2018.03.022
Stähli BE, Gebhard C, Gick M et al (2018) Outcomes after percutaneous coronary intervention for chronic total occlusion according to baseline renal function. Clin Res Cardiol 107:259–267. https://doi.org/10.1007/s00392-017-1179-x
Kefer J, Tzikas A, Freixa X et al (2016) Impact of chronic kidney disease on left atrial appendage occlusion for stroke prevention in patients with atrial fibrillation. Int J Cardiol 207:335–340. https://doi.org/10.1016/j.ijcard.2016.01.003
Mehta RL, Kellum JA, Shah SV et al (2007) Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:1–8. https://doi.org/10.1186/cc5713
Levey AS, De Jong PE, Coresh J et al (2011) The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int 80:17–28. https://doi.org/10.1038/ki.2010.483
Gurm HS, Dixon SR, Smith DE et al (2011) Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol 58:907–914. https://doi.org/10.1016/j.jacc.2011.05.023
Koskinas KC, Shakir S, Fankhauser M et al (2016) Predictors of early (1-Week) outcomes following left atrial appendage closure With Amplatzer devices. JACC Cardiovasc Interv 9:1374–1383. https://doi.org/10.1016/j.jcin.2016.04.019
Tzikas A, Holmes DR, Gafoor S et al (2017) Percutaneous left atrial appendage occlusion: the Munich consensus document on definitions, endpoints, and data collection requirements for clinical studies. Europace 19:4–15. https://doi.org/10.1093/europace/euw141
Rihal CS, Textor SC, Grill DE et al (2002) Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation 105:2259–2264. https://doi.org/10.1161/01.CIR.0000016043.87291.33
Keaney JJ, Hannon CM, Murray PT (2013) Contrast-induced acute kidney injury: how much contrast is safe? Nephrol Dial Transplant 28:1376–1383. https://doi.org/10.1093/ndt/gfs602
Feldkamp T, Luedemann M, Spehlmann ME et al (2018) Radial access protects from contrast media induced nephropathy after cardiac catheterization procedures. Clin Res Cardiol 107:148–157. https://doi.org/10.1007/s00392-017-1166-2
Amin AP, Bach RG, Caruso ML et al (2017) Association of variation in contrast volume with acute kidney injury in patients undergoing percutaneous coronary intervention. JAMA Cardiol 2:1007–1012. https://doi.org/10.1001/jamacardio.2017.2156
Tsai TT, Patel UD, Chang TI et al (2014) Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR cath-PCI registry. JACC Cardiovasc Interv 7:1–9. https://doi.org/10.1016/j.jcin.2013.06.016
Celik O, Ozturk D, Akin F et al (2015) Association between contrast media volume-glomerular filtration rate ratio and contrast-induced acute kidney injury after primary percutaneous coronary intervention. Angiology 66:519–524. https://doi.org/10.1177/0003319714542277
Sinning JM, Ghanem A, Steinhuser H et al (2010) Renal function as predictor of mortality in patients after percutaneous transcatheter aortic valve implantation. JACC Cardiovasc Interv 3:1141–1149. https://doi.org/10.1016/j.jcin.2010.09.009
Spieker M, Hellhammer K, Katsianos S et al (2018) Effect of acute kidney injury after percutaneous mitral valve repair on outcome. Am J Cardiol 122:316–322. https://doi.org/10.1016/j.amjcard.2018.03.358
Rudnick MR, Goldfarb S, Wexler L et al (1995) Nephrotoxicity of ionic and nonionic contrast media in 1196 patients: a randomized trial. Kidney Int 47:254–261. https://doi.org/10.1038/ki.1995.32
Laskey WK, Jenkins C, Selzer F et al (2007) Volume-to-creatinine clearance ratio. A pharmacokinetically based risk factor for prediction of early creatinine increase after percutaneous coronary intervention. J Am Coll Cardiol 50:584–590. https://doi.org/10.1016/j.jacc.2007.03.058
Park HS, Kim CJ, Yi JE et al (2015) Contrast volume/raw eGFR ratio for predicting contrast-induced acute kidney injury in patients undergoing percutaneous coronary intervention for myocardial infarction. CardioRenal Med 5:61–68. https://doi.org/10.1159/000369940
Aminian A, Lempereur M, Ben Yedder M, Dubois P (2018) Real-time fusion of echocardiography and fluoroscopy allowing successful implantation of a WATCHMAN device without contrast injection. EuroIntervention 14:174–175. https://doi.org/10.4244/EIJ-D-17-00398
Sedaghat A, Al-Kassou B, Vij V et al (2019) Contrast-free, echocardiography-guided left atrial appendage occlusion (LAAo): a propensity-matched comparison with conventional LAAo using the AMPLATZER™ Amulet™ device. Clin Res Cardiol 108:333–340. https://doi.org/10.1007/s00392-018-1401-5
Acknowledgements
All co-authors contributed fully in terms of the design of the study, the evaluation of data, the actual manuscript preparation, and the revision and approval of the final submitted manuscript. As the corresponding author, Dr. Gloekler confirms that all authors have approved the final text.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexander Sedaghat has received travel grants from Abbott, Boston Scientific, Medtronic and Edwards Lifesciences. Baravan Al-Kassou has received travel grants from Abbott. Jan Wilko Schrickel has participated in clinical trials conducted by Abbott. Fabian Nietlispach is a consultant to Abbott, Edwards Lifesciences, and Medtronic. Marco Valgimigli reports research grants, advisory board and lectures fees from Abbott; Stephan Windecker received grants to the institution from Abbott, Biotronik, Boston Scientific, Medtronic and Edwards Lifesciences; Bernhard Meier received speaker and proctor fees from Abbott. Georg Nickenig has received speaker honoraria from Abbott. Steffen Gloekler received institutional grants from Abbott and a grant from the Swiss Heart Foundation. The other authors have no conflicts of interest.
Ethical approval
Declaration of Helsinki: The authors state that the study complies with the Declaration of Helsinki. The locally appointed ethics committee has approved the research protocol. Informed consent has been obtained from the subjects.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table
3 Clinical characteristics depending on periprocedural imaging modalities (DOCX 16 kb)
Supplemental Table
4 Multivariate analysis for independent predictive value for 1-year mortalities (DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Sedaghat, A., Vij, V., Streit, S.R. et al. Incidence, predictors, and relevance of acute kidney injury in patients undergoing left atrial appendage closure with Amplatzer occluders: a multicentre observational study. Clin Res Cardiol 109, 444–453 (2020). https://doi.org/10.1007/s00392-019-01524-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01524-9