Abstract
Aim
Osteoporotic thoracolumbar fractures are of increasing importance. To identify the optimal treatment strategy this multicentre prospective cohort study was performed.
Purpose
Patients suffering from osteoporotic thoracolumbar fractures were included. Excluded were tumour diseases, infections and limb fractures. Age, sex, trauma mechanism, OF classification, OF-score, treatment strategy, pain condition and mobilization were analysed.
Methods
A total of 518 patients’ aged 75 ± 10 (41–97) years were included in 17 centre. A total of 174 patients were treated conservatively, and 344 were treated surgically, of whom 310 (90%) received minimally invasive treatment. An increase in the OF classification was associated with an increase in both the likelihood of surgery and the surgical invasiveness.
Results
Five (3%) complications occurred during conservative treatment, and 46 (13%) occurred in the surgically treated patients. 4 surgical site infections and 2 mechanical failures requested revision surgery. At discharge pain improved significantly from a visual analogue scale score of 7.7 (surgical) and 6.0 (conservative) to a score of 4 in both groups (p < 0.001). Over the course of treatment, mobility improved significantly (p = 0.001), with a significantly stronger (p = 0.007) improvement in the surgically treated patients.
Conclusion
Fracture severity according to the OF classification is significantly correlated with higher surgery rates and higher invasiveness of surgery. The most commonly used surgical strategy was minimally invasive short-segmental hybrid stabilization followed by kyphoplasty/vertebroplasty. Despite the worse clinical conditions of the surgically treated patients both conservative and surgical treatment led to an improved pain situation and mobility during the inpatient stay to nearly the same level for both treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic vertebral body fractures of the thoracolumbar spine (OVCFs) are an increasingly frequent health care issue. In Germany, the incidence of OVCFs in the lumbar spine among people over 70 years of age increased by 21%, reaching 254/100,000, and the incidence in the thoracic spine increased by 32%, reaching 137/10,000 [1].
The optimal treatment strategy for OVCFs has yet to be identified. A large number of studies have evaluated conservative treatment as well as operative treatment using cement augmentation for these fractures [2,3,4]. Two level I studies found contradictory results [5, 6]. However, the number of studies examining posterior fixation of OVCFs is limited. In summary, the literature does not provide a clear recommendation for treatment. One of the reasons for this lack of a clear recommendation may be the insufficient classification of OVCFs. Several studies examining the treatment of OVF used the Genant classification [4,5,6]. Therefore, the stability of the fracture was not sufficiently considered. In particular, both the involvement of the posterior ligament complex and the posterior cortex are not components of the Genant classification.
To solve this problem, in 2018, the Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopedics and Trauma (AG-OF) published a classification system for osteoporotic thoracolumbar fractures, i.e. the OF classification [7], which is presented in Fig. 1.
Five types of classification: a and b OF1 No deformation (vertebral body oedema in MRI-STIR), c and d OF 2 Deformation of one endplate, e and f OF3 Deformation of one endplate with distinct involvement of the posterior wall, g and h OF 4 Deformation of both endplates with/without posterior wall involvement, i OF5 Injuries with tension band failure
Additionally, treatment recommendations for each fracture type and the OF score (Table 1) were developed [8]. Posterior stabilization was recommended in unstable fractures, such as OF type 3–5 fractures, depending on the clinical course. To date, several studies have evaluated the treatment of OVCFs using the OF score [2, 9,10,11,12], including the treatment of short- and long-segmental posterior stabilizations. Recently, OF classifications have gained an increased level of acceptance [13,14,15].
With the aim of evaluating the OF-score, the AG-OF designed the “Clinical evaluation of the OF-score for therapy planning and treatment recommendations for osteoporotic fractures of the thoracolumbar spine” study (EOFTT).
The current investigation focused on inpatient treatment and clinical results up to discharge and evaluated treatment modalities with regard to the OF classification and OF-score.
Materials and methods
This study was approved by the research ethics committee of the Medical Association of Saxony Anhalt Germany (14. June 2017, file number 31/17) and was performed in accordance with the Declaration of Helsinki. Additionally, each participating centre had an approval of their regional ethic committee. The patients were informed about the study and included in the study only after signing their consent. Data were collected prospectively and across multiple centres. The inclusion criterion was hospital admission caused by acute osteoporotic thoracolumbar fractures. Acute fractures were defined as a fracture that occurred no more than 3 months ago or a fracture with oedema on MRI. Furthermore, patients had to be diagnosed with osteoporosis according to WHO criteria, be at least 18 years old. The exclusion criteria were tumor diseases, infections (e.g. spondylodiscitis), and limb injuries affecting mobilization or other outcome parameters.
Data collection was carried out by the participating centre using a case report form (CRF). The completed CRF was returned to the central study centre where data processing was performed. Each participating centre was coded as a two-digit numeric ID, and each patient was anonymized by using a two- or three-digit numerical ID (e.g. 01–123).
Diagnosis
The fractures were detected using at least one of the following modalities: X-ray, CT scan and MRI. Epidemiological data, such as duration of hospital stay, age, sex, cause of OVCF (traumatic or spontaneous) fracture, morphology (OF classification), and fracture level, were recorded.
Osteoporosis was diagnosed following the DVO [16] and WHO [17] recommendations. For patients older than 75 years of age, no specific diagnosis was necessary. In younger patients (≤ 75 years), bone quality was evaluated by either DEXA, q-CT or Hounsfield unit (HU) measurement in the technique described by Schreiber et al. [18]. Exclusively, patients with osteoporotic bone quality were included.
For the description of the patients’ ASA classification, anticoagulation therapy, spinal neurological status (normal, radiculopathy, paraparesis, cauda equina syndrome) and dementia were recorded.
The OF-score was assessed at admission, the day of treatment decision (dtd) and discharge.
In cases treated with conservative therapy, the use of orthoses, physiotherapy and analgesic drugs (WHO scheme) were recorded.
Surgical therapy was subdivided into four main categories:
-
1.
standalone vertebroplasty/kyphoplasty,
-
2.
short-segmental-posterior fixation (2-segments),
-
3.
long-segmental (> 2 segments) posterior fixation, and
-
4.
combined anterior–posterior approach (long and short segmental posterior fixation).
Short-segmental posterior fixation was subdivided into four categories depending on the augmentation state:
-
1.
augmentation of pedicle screws and fractured vertebral body (hybrid stabilization),
-
2.
augmentation of pedicle screws without augmentation of the fractured vertebral body,
-
3.
augmentation of the fractured vertebral body without screw augmentation, and
-
4.
without any PMMA augmentation.
Additionally, the surgical procedure was subdivided into two groups based on invasiveness: open surgery (OS) and minimally invasive surgery (MIS).
Outcomes
The length of hospital stay was recorded in days. Pain was characterized using the visual analogue scale (0–10). Mobility was assessed using an ordinal 5-point Likert scale that was scored as follows: 1—fully mobile without an assistive device, 2—wheeled walker or forearm crutches, 3—mobile with a high walker, 4—bed edge and stand, 5—bedridden at three time points, i.e. before fracture, admission and discharge.
Complications were recorded as common complications (urinary tract infection, thrombosis, embolism, delirium, pneumonia), surgery-associated complications (mechanical implant failure, surgical site infection, superficial wound healing disorder, revision surgery necessary) and neurological complications (radiculopathy, paraplegia or conus-medullaris syndrome).
Statistical methods
Differences in gender and the occurrence of trauma in OF classification were assessed with Chi2 tests or Fisher’s exact text, as appropriate. The correlation between age and fracture location with fracture morphology was analysed with Spearman’s correlation analysis.
The correlation of the severity of fracture morphology (OF classification) with the scope/severity of treatment was calculated using Cramer’s V, where values 0.1 indicate small effects, values of 0.3 indicate medium effects and values greater 0.5 indicate large effects [19].
Binary logistic regression analyses were performed to investigate the relation between complications and OF classification and invasiveness of therapy. The quality of the model was assessed using Nagelkerke’s pseudo-R2.
The effect of the OF classification on the applied therapy (surgical or conservative) was assessed using the Chi2 test and contingence coefficient.
Differences in the hospital stay were analysed using the Mann‒Whitney U test. The change in pain and mobility during the hospital stay and differences depending on the performed therapy were analysed using a repeated-measures general linear model. The dependent variables (pain and mobility) were used as within-subjects factors, and the selected therapy was used as a between-subjects factor. The correlation between intervention severity/invasiveness was assessed with Spearman’s correlation analysis. Differences in the use of analgesic drugs between therapy types were assessed using the Chi2 test.
Differences in the frequency of complications between surgically and conservatively treated patients were assessed using the Chi2 test or Fisher’s exact test.
The prediction of surgical complications by OF classification and the invasiveness of the surgical intervention was assessed by binomial logistic regression. Both variables were considered ordinal variables. The reference for the odds of developing complications was OF1 and vertebroplasty/kyphoplasty, which were defined as the lowest grade of fracture severity and surgical invasiveness, respectively. The odds for general complications were also examined using binomial logistic regression. OF1 was used as the reference for the odds for OF classification, and conservative treatment was used as the reference for the selected therapy; both variables were defined as the mildest level of fracture severity and treatment invasiveness.
For statistical analyses, SPSS Version 27.0 (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp) was used with an alpha of 0.05.
Results
Seventeen participating centres (16 German, 1 Swiss) collected data from patients with OVCF. 689 patients were eligible for the study during the inclusion period. 518 patients (128 men, 390 women, 75 ± 10 years, range 41–97) could be included in the study.
The diagnosis of fracture was radiologically clarified with only one imaging modality in 7% of the patients (X-ray: 5%, MRI: 0.4%, CT: 1.6%). A total of 32% of patients were diagnosed using at least two, and 61% of patients were diagnosed using three imaging modalities.
Sixty-five percent of the patients (n = 338) reported a trauma, while 33% (n = 168) reported no trauma. In 2% of patients (n = 12), it was unclear whether trauma had occurred.
The OVCFs were located between Th2 and L5. The majority (70%) of the fractures were located at the thoracolumbar junction (Th11: 6%, Th12: 22%, L1: 30%, L2: 12%). The remaining OVCFs were localized at the mid thoracic spine (14%) and the lower lumbar spine (16%).
In 53% (N = 276) of the patients DEXA score (− 3.21 ± 1.15) was obtained. QCT was performed in 28% (N = 147) of all patients (qCT 62 ± 24 mgHA/cm3). The frequently determination of bone quality was performed using Hounsfield Units in 81% (N = 419) of all patients. A combination of two or three methods was performed in 54% (N = 279).
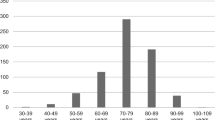
The OF classification ranged from 1 to 5. OF3 was the most frequent type (42%); OF2 and OF4 fractures were present in 26% and 27% of patients, respectively; and OF1 and OF5 fractures were present in 1% and 4% of patients, respectively. Further information about the distribution of the OF classification subgroups and the distribution of fracture levels are shown in Table 2 and Fig. 2.
The severity of fracture increased with age (r = 0.104, p = 0.018) and more cranial (thoracic) fracture localization (r = 0.106, p = 0.016). Sex (p = 0.970) and memorable trauma (p = 0.678) were shown to have no effect on the severity of fracture morphology.
Fracture–related neurological deficits were found in 12 patients (3%), while eleven patients showed neurological radicular symptoms and one showed transversal symptoms.
The surgically treated patients had a slightly higher ASA status than the conservatively treated patients (p = 0.028, r = 0.095). Anticoagulation therapy was provided to 163 (31%) patients at admission, with no differences between surgically (33%) and conservatively (29%) treated patients (p = 0.368). Dementia was diagnosed in a total of 30 patients, with no significant differences between the treatment groups (p = 0.695). Dependency on nursing was observed in 59 (11%) patients, with no significant differences between the groups (p = 0.770).
Initially, a reduction in OF-score values from admission to the day of treatment decision (dtd) was observed (admission: 6.51 ± 2.48, dtd: 6.38 ± 2.55, p = 0.004). The OF-score for treatment recommendation at dtd ranged from 0 to 13 points. In 49% of patients (n = 251), surgical treatment was recommended, and in 37% of patients (n = 190), conservative treatment was recommended. In 14% of patients (n = 74), the OF-score was six, leading to indifferent therapeutic recommendations. At discharge, the mean OF-score was 4.8 ± 2.4 (admission: p < 0.001, dtd: p < 0.001). The change in OF-score during the inpatient stay is shown in Fig. 3 for the surgical and conservative treatment groups.
Fisher’s exact test showed that OF classification was a significant predictor of therapy choice (p < 0.001). The higher the OF classification, the more likely surgery was be performed (contingence coefficient = 0.264). Ultimately, 66% of patients received surgical treatment. Table 3 presents an overview of the relation between OF classification and therapy choice.
The most common surgical intervention (46%, n = 159) was two-level posterior fixation. Stand-alone kyphoplasty or vertebroplasty was used in 39% (n = 134) of cases. Table 4 provides detailed information about surgical treatment based on the OF classification. Figure 4 shows an example for each surgical category.
a and b OF2, fracture with slight deformation without or little posterior wall involvement, kyphoplasty was performed because of drug resistant pain; c and d OF3, fracture with deformation and posterior wall involvement, short segmental posterior fixation with augmentation of screws and fractured vertebra (hybrid stabilization) was performed; e and f OF5, fracture with tension band injury due to fall from bed, multimorbid 87-year-old female, posterior long segmental fixation with screw augmentation was performed; g and h OF 3 fracture due to fall from standing position, 60-year-old surgical stuff nurse with qCT proven osteoporosis 67 mg Ca hydroxylapatit/cm3, one stage anterior posterior reduction and fixation was performed
Detailed information about the variation of short segmental posterior fixation and its combination with or without screw or index-vertebra augmentations is shown in Table 5.
A total of 310 (90,1%) of 344 surgical procedures were performed with minimal invasiveness. The invasiveness of treatment was moderately correlated with the severity of fracture morphology (p < 0.001, r = 0.385).
Conservative treatment was performed in 34% (n = 174) of patients, 94% (n = 157) of whom received physiotherapy and 22% (n = 37) of whom received orthotic treatment. In 18% of all conservatively treated patients, a combination of orthosis and physiotherapy was used.
The conservatively treated patients received lower amounts of pain medication on the day of the treatment decision than the surgically treated patients (p < 0.001). At the time of discharge, conservatively treated patients received 44% (n = 75) level I pain medication, 33% (n = 56) received level II pain medication, and 23% (n = 39) received level III pain medication according to the WHO ladder. In contrast, among surgically treated patients, 24% (n = 80) received level I pain medication, 40% (n = 136) received level II pain medication, and 36% (n = 123) received level III pain medication.
The mean hospital stay was 10 ± 7 d and differed significantly between treatment groups (p < 0.001). The mean hospital stay among surgically treated patients (12 ± 7 d) was 5 days longer than that of conservatively treated patients (7 ± 5 d).
During the hospital stay, both treatment groups showed significant improvement in pain (p < 0.001); patients in the surgical treatment group experienced better pain reduction (p < 0.001) in comparison with higher initial values (p < 0.001). At hospital discharge, no significant differences in pain were observed between conservative and surgically treated patients (p = 0.577).
The mobility of patients was significantly better before fracture emergence than at admission. Mobility was significantly worse before intervention in surgically treated patients than in conservatively treated patients (admission: p < 0.001). The improvement in mobility was significantly stronger for surgically treated patients than for conservatively treated patients (p = 0.007). In both groups, significant improvement in mobility was achieved (p < 0.001). Despite these findings, the conservatively treated patients showed significantly (p < 0.001) better mobility than the surgically treated patients at discharge (Fig. 5).
Level of mobility using an ordinal 5-point Likert scale (level 1: fully mobile without assistive device, 2-wheeled walker or forearm crutches, 3–mobile with high walker, 4-bed edge and stand, 5–bedridden) of patients with osteoporotic fractures before the fracture occurred, at admission and at discharge. Data are presented as the means and 95% confidence intervals (CI) in grey for conservatively treated patients and in black for surgically treated patients
A total of 5 (3%) complications occurred in the conservatively treated group, while 46 (13%) occurred in the surgically treated group (p = 0.001). Revision surgery was necessary in 6 cases (2%); two cases were due to mechanical implant failure, and four cases were due to a surgical site infection. Details about surgery-associated and general complications among surgically and conservatively treated patients are shown in Table 6. In two patients, neurological deterioration occurred with mild radiculopathy after surgery. In both cases, no revision was performed due to the mild degree and spontaneous remission.
Details about common complications are shown in Table 7. It should be noted that some patients reported more than one complication.
Linear regression analysis revealed that OF classification was not a significant predictor of surgical complications (p > 0.973) or the invasiveness of surgical treatment (p > 0.469). The model quality was poor (Nagelkerke’s R2 = 0.064).
Regarding general complications, surgical invasiveness showed no significant difference compared to conservative treatment (p > 0.113). With poor model quality (Nagelkerke’s R2 = 0.130), the OF classification showed a significant impact on general complications for OF3 (p = 0.032), OF4 (p = 0.007) and OF5 (p = 0.006) compared to OF1.
Discussion
The treatment of OVCFs remains controversial since very few recommendations exist [3, 8, 13]. The recently developed OF-score aims to facilitate the decision of whether to operate in OVCFs by incorporating radiological and clinical aspects [8]. The presented results of the study “Clinical Evaluation of the OF-score for Therapy-Planning and Treatment-Recommendations for Osteoporotic Fractures of the thoracolumbar spine” provide further knowledge regarding the inpatient course.
The most important findings of this study are the distribution of the fracture morphologies at the thoracolumbar spine with predominant OF2-4 fractures and only minor numbers of OF1 and OF5 fractures. OF4 fractures were relatively common at the mid-thoracic spine and at Th12 and L1. The therapy strategy was dependent on fracture type. Mainly conservative treatment and stand-alone cement augmentation were performed in OF2 fractures. Conservative treatment, standalone cement augmentation and short segmental stabilization were predominantly performed in OF3 fractures, with a similar distribution between the treatment strategies. Mainly, short-segmental stabilization was performed in OF4 fractures with an increasing rate of long-segmental stabilizations, which is equally common to conservative treatment.
To the authors’ best knowledge, this study is one of the largest prospective studies of OVCFs in the literature. The large number of prospectively included patients is comparable to the study published by Reinhold et al. [20]. However, only a minority of patients in their study suffered from OVCFs. Similarly, the fracture distribution showed a bimodal distribution, mainly affecting the thoracolumbar junction. This is consistent with previous findings on OVCFs [21]. Schnake et al. [23] included a similar patient cohort but did not evaluate clinical outcomes.
The OF-score is a dynamic score that is based on pain situation, grade of mobility and fracture morphology. Thus, conservative therapy was mainly performed in patients with stable fractures OF1 and OF2 or in those with higher fracture severity but rather low pain levels and sufficient mobility. Thus, patients who were treated conservatively had either low pain levels at admission or improved after receiving sufficient pain medication over the first 3 to 5 days. This can be interpreted, that the OF-score indicates changes in the clinical course and leads to a separation of the cohort into two groups. The group with a reduction in OF score under initial conservative therapy will continue to be treated conservatively. The group with no reduction in OF score will receive surgical therapy.
Interestingly, at discharge, there was a persistent and significant reduction in the OF-score in both groups associated with lower pain levels and superior mobility in comparison to admission status. Thus, the surgically treated patients had a significantly stronger improvement at discharge than the conservatively treated patients. Generally, the OF-score seems to be a useful tool for decision-making leading to an improvement in the patient condition at discharge for both conservative and operative treatment.
The treatment strategies performed were in accordance with the recommendations of Blattert et al. [8]. Patients suffering from stable OF2 fractures received either conservative treatment or standalone cement augmentation. Herein, cement augmentation was recommended in patients with persistent pain and reduced mobility despite sufficient analgesics in accordance with the OF-score [8]. Posterior stabilization is the most commonly used technique in patients suffering from fractures with a higher degree of instability, such as type OF3-5 fractures. The equal distribution of conservative treatment, standalone cement augmentation, and posterior short-segmental stabilization in patients with OF3 fractures can be explained by the diversity of these fractures being comparable to the heterogeneous therapy strategies in patients with traumatic incomplete burst fractures type AO Spine A3 [22]. The real fracture instability is dependent on the degree of posterior wall involvement. In contrast, posterior stabilization is the dominant therapy strategy in patients with type OF4 and 5 fractures. Both conservative and surgical treatment led to a significant reduction in pain and improved mobility during the in-hospital stay. Therefore, both the pain situation and the level of mobility on admission were worse in the surgically treated patients. This is not a surprising finding considering the higher level of instability seen in those patients.
In comparison to the data presented by Schnake et al. [23], who prospectively included 707 patients in 2012, treatment strategies have changed over the years. In comparison, a higher rate of patients (82%) were treated surgically. Therefore, the rate of standalone augmentation was far higher (66%) than that in our patients (25%). This could be explained by the fact that the surgical strategies focus on short segmental posterior fixation for fractures of OF3–OF5 and more conservative treatment in OF1–OF2 fractures. Similarly, Bigdon et al. reported a tendency towards fewer standalone augmentation procedures over the ten years. However, this is still an ongoing debate [5, 6].
Considering the 157 patients treated with short-segmental posterior stabilization, the majority of surgeries were performed via MIS. This is in accordance with the recommendations published in the literature based on the lower morbidity and lower blood loss associated with MIS [24,25,26]. The dominant treatment strategy in the included patients was hybrid stabilization, including posterior short-segmental stabilization and cement augmentation of the fractured vertebral body. Some authors even report a lower rate of subsequent fractures with this surgical technique compared to kyphoplasty standalone, especially for OF2 and OF3 fractures in the thoracolumbar region [27]. Traumatic vertebral disc lesions can be neglected in patients suffering from OVCFs. The intervertebral discs are commonly sclerotic, and the dominant trauma mechanisms are low-energy accidents [28]. Thus, hybrid stabilization in MIS represents a minimally invasive 360° stabilization performed via an isolated posterior approach. Interestingly, approximately one-third of all included patients suffered from atraumatic OVCFs. Therefore, the relative rate of atraumatic fractures was highest at the mid-thoracic spine. Similarly, it has been shown that higher rates of midthoracic fractures are related to frailty [29].
Generally, the presented therapy strategy is more aggressive than the strategies published in the literature, with a predominance of conservative treatment or stand-alone augmentation strategies in OVCFs. Reasons could be the high demand of the patients and the unrestricted availability of minimally invasive surgical techniques. Additionally, only acute fractures in an inpatient setting were included.
Although the overall number of complications was high, only 2% of surgically treated patients had to undergo revision surgery. The majority of complications were nonsurgical and not life threatening and could thus be treated conservatively. Overall, the number of complications was comparable to or even lower than that reported in the literature [30, 31].
Limitations
The study has several limitations. Due to the study design no actual control cohort exists. This limits the assessability of the therapy decision based on the therapy success. Based on the results of this study, detailed questions regarding therapy should be investigated in future prospective randomized trials.
Only data from the inpatient stay were evaluated. Based on the multicentric approach of the study, the indication of surgery may differ between the involved centres. Thus, the individual benefits of each treatment strategy were not investigated. Additionally, the treatment strategy used might have been influenced by the patient’s wishes rather than the recommendation of the surgeons. Detailed data on comorbidities were not collected, therefore interactions between them and complication rates remain unclear. The prospective, multicentre nature of this study and the sample size of more than 500 patients are strengths of this study. This study provided a comprehensive overview of the demographic situation in the German speaking countries with regard to the fracture location, fracture severity, and initial treatment.
Conclusion
The OF classification is suitable to indicate the fracture severity, and it is significantly and positively correlated with surgical invasiveness. The most commonly used posterior stabilization strategy was minimally invasive short-segmental hybrid stabilization. Both conservative and surgical treatment strategies lead to improvements in pain, mobility and the OF-score during the inpatient stay.
Abbreviations
- OVCF:
-
Osteoporotic vertebral compression fracture of the thoracolumbar spine
- EOFTT:
-
Clinical evaluation of the OF-score for therapy planning and treatment recommendations for osteoporotic fractures of the thoracolumbar spine
- HU:
-
Hounsfield unit
- dtd:
-
Day of treatment decision
- AG-OF:
-
Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopedics and Trauma
References
Rupp M, Walter N, Pfeifer C, Lang S, Kerschbaum M, Krutsch W, Baumann F, Alt V (2021) The incidence of fractures among the adult population of Germany-an analysis from 2009 through 2019. Dtsch Arztebl Int 118(40):665–669
Zhai G, Li A, Liu B, Lv D, Zhang J, Sheng W, Yang G, Gao Y (2021) A meta-analysis of the secondary fractures for osteoporotic vertebral compression fractures after percutaneous vertebroplasty. Medicine 100(16):e25396
Spiegl U, Bork H, Grüninger S, Maus U, Osterhoff G, Pieroh P, Schnoor J, Heyde C, Schnake K (2021) Osteoporotic fractures of the thoracic and lumbar vertebra: diagnosis and conservative treatment-a systematic review. Dtsch Arztebl Int 118(40):670–677
Wu Y, Wang F, Zhou J-Q, Liu C-Y, Wu R-X (2014) Analysis of clinical effects of percutaneous vertebroplasty and percutaneous kyphoplasty in treating osteoporotic vertebral compression fracture. Zhongguo Gu Shang = China J Orthop Traumatol 27(5):385–389
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361(6):557–568
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361(6):569–579
Schnake KJ, Blattert TR, Hahn P, Franck A, Hartmann F, Ullrich B, Verheyden A, Mörk S, Zimmermann V, Gonschorek O (2018) Classification of osteoporotic thoracolumbar spine fractures: recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Glob Spine J 8(2_suppl):46S-49S. https://doi.org/10.1177/2192568217717972
Blattert TR, Schnake KJ, Gonschorek O, Gercek E, Hartmann F, Katscher S, Mörk S, Morrison R, Müller M, Partenheimer A (2018) Nonsurgical and surgical management of osteoporotic vertebral body fractures: recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Glob Spine J 8(2_suppl):50S-55S
Palmowski Y, Balmer S, Hu Z, Winkler T, Schnake KJ, Kandziora F, Pumberger M (2020) Relationship between the OF classification and radiological outcome of osteoporotic vertebral fractures after kyphoplasty. Glob Spine J. https://doi.org/10.1177/2192568220964051
Palmowski Y, Balmer S, Bürger J, Schömig F, Hu Z, Pumberger M (2020) Influence of operative timing on the early post-operative radiological and clinical outcome after kyphoplasty. Eur Spine J 29(10):2560–2567
Spiegl UJ, Hölbing P-L, Jarvers J-S, vd Höh N, Pieroh P, Osterhoff G, Heyde C-E (2021) Midterm outcome after posterior stabilization of unstable Midthoracic spine fractures in the elderly. BMC Musculoskelet Disord 22(1):1–10
Spiegl UJ, Anemüller C, Jarvers J-S, von der Höh N, Josten C, Heyde C-E (2019) Hybrid stabilization of unstable osteoporotic thoracolumbar vertebral body fractures: clinical and radiological outcome after a mean of 4 years. Eur Spine J 28(5):1130–1137
Rajasekaran S, Kanna RM, Schnake KJ, Vaccaro AR, Schroeder GD, Sadiqi S, Oner C (2017) Osteoporotic thoracolumbar fractures—how are they different?—classification and treatment algorithm. J Orthop Trauma 31:S49–S56
Schönrogge M, Lahodski V, Otto R, Adolf D, Damm R, Sitte-Zöllner A, Piatek S (2022) Inter- and intraobserver reliabilities and critical analysis of the osteoporotic fracture classification of osteoporotic vertebral body fractures. Eur Spine J. https://doi.org/10.1007/s00586-022-07201-2
Quinteros G, Cabrera JP, Urrutia J, Carazzo CA, Guiroy A, Marre B, Joaquim A, Yurac R (2022) Reliability evaluation of the new AO spine-DGOU classification for osteoporotic thoracolumbar fractures. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.02.029
Thomasius F, Baum E, Bernecker P, Böcker W, Brabant T, Clarenz P, Demary W, Dimai H, Engelbrecht M, Engelke K (2018) DVO Guideline 2017 on prophylaxis, diagnosis and therapy of osteoporosis in postmenopausal women and men. Osteologie 27(03):154–160
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. Osteoporos Int 4(6):368–381
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Jt Surg Am 93(11):1057–1063. https://doi.org/10.2106/JBJS.J.00160
Ellis PD (2010) The essential guide to effect sizes: statistical power, meta-analysis, and the interpretation of research results. Cambridge University Press
Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M (2010) Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, internet-based multicenter study of the spine study group of the German association of trauma surgery. Eur Spine J 19(10):1657–1676. https://doi.org/10.1007/s00586-010-1451-5
Nevitt M, Ross P, Palermo L, Musliner T, Genant H, Thompson D, Group FITR (1999) Association of prevalent vertebral fractures, bone density, and alendronate treatment with incident vertebral fractures: effect of number and spinal location of fractures. Bone 25(5):613–619
Spiegl U, Jarvers J-S, Heyde C-E, Josten C (2017) Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360°-stabilization. Eur J Trauma Emerg Surg 43(1):27–33
Schnake KJ, Bouzakri N, Hahn P, Franck A, Blattert TR, Zimmermann V, Gonschorek O, Ullrich B, Kandziora F, Müller M (2021) Multicenter evaluation of therapeutic strategies of inpatients with osteoporotic vertebral fractures in Germany. Eur J Trauma Emerg Surg 48(2):1401–1408
Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V (2014) Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 20(2):150–156
Wang B, Fan Y, Dong J, Wang H, Wang F, Liu Z, Liu H, Feng Y, Chen F, Huang Z (2017) A retrospective study comparing percutaneous and open pedicle screw fixation for thoracolumbar fractures with spinal injuries. Medicine 96(38):e8104
Kohler FC, Schenk P, Bechstedt-Schimske M, Ullrich B, Klauke F, Hofmann G, Mendel T (2021) Open versus minimally invasive fixation of thoracic and lumbar spine fractures in patients with ankylosing spinal diseases. Eur J Trauma Emerg Surg 48(3):2297–2307
Aboud N, Eckardt N, Kamp MA, Senft C, Schwarz F (2022) Occurrence of adjacent segment fractures after surgical treatment of an osteoporotic vertebral fracture: a retrospective comparison between two different treatment methods. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04434-0
Adams MA, Dolan P (2011) Biomechanics of vertebral compression fractures and clinical application. Arch Orthop Trauma Surg 131(12):1703–1710
Spiegl UJ, Scheyerer MJ, Osterhoff G, Grüninger S, Schnake KJ (2021) Osteoporotic mid-thoracic vertebral body fractures: what are the differences compared to fractures of the lumbar spine?—a systematic review. Eur J Trauma Emerg Surg 48(3):1639–1647
Rometsch E, Spruit M, Zigler JE, Menon VK, Ouellet JA, Mazel C, Härtl R, Espinoza K, Kandziora F (2020) Screw-related complications after instrumentation of the osteoporotic spine: a systematic literature review with meta-analysis. Glob Spine J 10(1):69–88
Bigdon SF, Saldarriaga Y, Oswald KA, Müller M, Deml MC, Benneker LM, Ecker MT, Albers CE (2022) Epidemiologic analysis of 8000 acute vertebral fractures: evolution of treatment and complications at 10-year follow-up. J Orthop Surg Res 17(1):1–12
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ullrich, B.W., Schenk, P., Scheyerer, M.J. et al. Georg Schmorl prize of the German spine society (DWG) 2022: current treatment for inpatients with osteoporotic thoracolumbar fractures—results of the EOFTT study. Eur Spine J 32, 1525–1535 (2023). https://doi.org/10.1007/s00586-022-07519-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07519-x