Abstract
Background
This is the first report from a multicenter prospective cohort study of colorectal neuroendocrine tumor (NET), the C-NET STUDY, conducted to assess the long-term outcomes of the enrolled patients. This report aimed to elucidate the clinicopathological features of the enrolled patients and lesions.
Methods
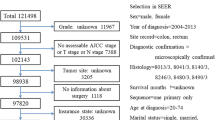
Colorectal NET patients aged 20–74 years were consecutively enrolled and followed up at 50 institutions. The baseline characteristics and clinicopathological findings at enrollment and treatment were assessed.
Results
A total of 495 patients with 500 colorectal NETs were included. The median patient age was 54 years, and 85.3% were asymptomatic. The most frequent lesion location was the lower rectum (88.0%); 99.4% of the lesions were clinically diagnosed to be devoid of metastatic findings, and 95.4% were treated with endoscopic resection. Lesions < 10 mm comprised 87.0% of the total, 96.6% had not invaded the muscularis propria, and 92.6% were classified as WHO NET grade 1. Positive lymphovascular involvement was found in 29.2% of the lesions. Its prevalence was high even in small NETs with immunohistochemical/special staining for pathological assessment (26.4% and 40.9% in lesions sized < 5 mm and 5–9 mm, respectively). Among 70 patients who underwent radical surgery primarily or secondarily, 18 showed positive lymph node metastasis.
Conclusions
The characteristics of real-world colorectal NET patients and lesions are elucidated. The high positivity of lymphovascular involvement in small NETs highlights the necessity of assessing the clinical significance of positive lymphovascular involvement based on long-term outcomes, which will be examined in later stages of the C-NET STUDY.
Trial registration number
UMIN000025215.
Similar content being viewed by others
References
Who Classification of Tumours Editorial Board (eds). WHO classification of tumours of the digestive system, 5th edn. 2019; Lyon: IARC Press.
Ahmed M. Gastrointestinal neuroendocrine tumors in 2020. World J Gastrointest Oncol. 2020;12:791–807.
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–42.
Ito T, Igarashi H, Nakamura K, et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: a nationwide survey analysis. J Gastroenterol. 2015;50:58–64.
Masui T, Ito T, Komoto I, Uemoto S, JNETS Project Study Group. Recent epidemiology of patients with gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NEN) in Japan: a population-based study. BMC Cancer. 2020;20:1104.
Basuroy R, Haji A, Ramage JK, et al. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016;44:332–45.
Ramage JK, Valle JW, Nieveen van Dijkum EJM, the ENETS 2016 Munich Advisory Board Participants; ENETS 2016 Munich Advisory Board Participants. Colorectal neuroendocrine neoplasms: areas of unmet need. Neuroendocrinology. 2019;108:45–53.
Ramage JK, De Herder WW, Delle Fave G, et al. ENETS consensus guidelines update for colorectal neuroendocrine neoplasms. Neuroendocrinology. 2016;103:139–43.
Kunz PL, Reidy-Lagunes D, Anthony LB, et al. North American Neuroendocrine Tumor Society. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42:557–77.
Ito T, Masui T, Komoto I, et al. JNETS clinical practice guidelines for gastroenteropancreatic neuroendocrine neoplasms: diagnosis, treatment, and follow-up: a synopsis. J Gastroenterol. 2021;56:1033–44.
de Mestier L, Brixi H, Gincul R, et al. Updating the management of patients with rectal neuroendocrine tumors. Endoscopy. 2013;45:1039–46.
Sekiguchi M, Sekine S, Sakamoto T, et al. Excellent prognosis following endoscopic resection of patients with rectal neuroendocrine tumors despite the frequent presence of lymphovascular invasion. J Gastroenterol. 2015;50:1184–9.
Kitagawa Y, Ikebe D, Hara T, et al. Enhanced detection of lymphovascular invasion in small rectal neuroendocrine tumors using D2–40 and Elastica van Gieson immunohistochemical analysis. Cancer Med. 2016;5:3121–7.
Nakamura K, Osada M, Goto A, et al. Short- and long-term outcomes of endoscopic resection of rectal neuroendocrine tumours: analyses according to the WHO 2010 classification. Scand J Gastroenterol. 2016;51:448–55.
Kang HS, Kwon MJ, Kim TH, et al. Lymphovascular invasion as a prognostic value in small rectal neuroendocrine tumor treated by local excision: a systematic review and meta-analysis. Pathol Res Pract. 2019;215: 152642.
Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma: the 3d English Edition [Secondary Publication]. J Anus Rectum Colon. 2019; 3: 175–95.
Soga J. Early-stage carcinoids of the gastrointestinal tract: an analysis of 1914 reported cases. Cancer. 2005;103:1587–95.
Hotta K, Shimoda T, Nakanishi Y, et al. Usefulness of Ki-67 for predicting the metastatic potential of rectal carcinoids. Pathol Int. 2006;56:591–6.
Konishi T, Watanabe T, Kishimoto J, et al. Prognosis and risk factors of metastasis in colorectal carcinoids: results of a nationwide registry over 15 years. Gut. 2007;56:863–8.
Fahy BN, Tang LH, Klimstra D, et al. Carcinoid of the rectum risk stratification (CaRRs): a strategy for preoperative outcome assessment. Ann Surg Oncol. 2007;14:1735–43.
Shields CJ, Tiret E, Winter DC. Carcinoid tumors of the rectum: a multi-institutional international collaboration. Ann Surg. 2010;252:750–5.
Fujimoto Y, Oya M, Kuroyanagi H, et al. Lymph-node metastases in rectal carcinoids. Langenbecks Arch Surg. 2010;395:139–42.
Yoon SN, Yu CS, Shin US, et al. Clinicopathological characteristics of rectal carcinoids. Int J Colorectal Dis. 2010;25:1087–92.
Park CH, Cheon JH, Kim JO, et al. Criteria for decision making after endoscopic resection of well-differentiated rectal carcinoids with regard to potential lymphatic spread. Endoscopy. 2011;43:790–5.
Kasuga A, Chino A, Uragami N, et al. Treatment strategy for rectal carcinoids: a clinicopathological analysis of 229 cases at a single cancer institution. J Gastroenterol Hepatol. 2012;27:1801–7.
Sugimoto S, Hotta K, Shimoda T, et al. The Ki-67 labeling index and lymphatic/venous permeation predict the metastatic potential of rectal neuroendocrine tumors. Surg Endosc. 2016;30:4239–48.
Ngamruengphong S, Kamal A, Akshintala V, et al. Prevalence of metastasis and survival of 788 patients with T1 rectal carcinoid tumors. Gastrointest Endosc. 2019;89:602–6.
Yamaguchi T, Takahashi K, Yamada K, et al. A nationwide, multi-institutional collaborative retrospective study of colorectal neuroendocrine tumors in Japan. Ann Gastroenterol Surg. 2020;5:215–20.
Acknowledgements
We would like to thank all investigators and physicians who participated in this study at the 50 participating institutions. We are also grateful to Ms. Natsuko Nishida and Ms. Naoko Sawada for their contribution to the study management. We also thank Editage (www.editage.com) for editing the draft of the manuscript.
Funding
This study was supported by the Japan Agency for Medical Research and Development (AMED; JP16ck0106102, JP19ck0106276).
Author information
Authors and Affiliations
Consortia
Contributions
All authors were involved in the design of the study and the data collection. MS, TM, and HI analyzed the data. MS drafted the article. All authors contributed to the critical revision of the article for important intellectual content and approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The following author disclosed financial relationships: Y. Takeuchi received speaker’s honoraria from Olympus. All other authors disclosed no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sekiguchi, M., Hotta, K., Takeuchi, Y. et al. Characteristics of colorectal neuroendocrine tumors in patients prospectively enrolled in a Japanese multicenter study: a first report from the C-NET STUDY. J Gastroenterol 57, 547–558 (2022). https://doi.org/10.1007/s00535-022-01877-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-022-01877-5