Abstract
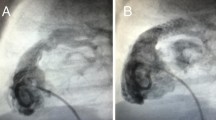
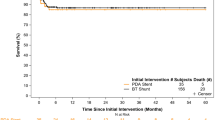
Neonates with symptomatic tetralogy of Fallot (sTOF) may undergo palliations with varying physiology, namely systemic to pulmonary artery connections (SPC) or right ventricular outflow tract interventions (RVOTI). A comparison of palliative strategies based on the physiology created is lacking. Consecutive sTOF neonates undergoing SPC or RVOTI from 2005–2017 were reviewed from the Congenital Cardiac Research Collaborative. The primary outcome was survival with successful complete repair (CR) by 18 months. A variety of secondary outcomes were assessed including overall survival, hospitalization-related comorbidities, and interstage reinterventions. Propensity score adjustment was utilized to compare treatment strategies. The cohort included 252 SPC (surgical shunt = 226, ductus arteriosus stent = 26) and 68 RVOTI (balloon pulmonary valvuloplasty = 48, RVOT stent = 11, RVOT patch = 9) patients. Genetic syndrome (29 [42.6%] v 75 [29.8%], p = 0.04), weight < 2.5 kg (28 [41.2%] v 68 [27.0%], p = 0.023), bilateral pulmonary artery Z-score < − 2 (19 [28.0%] v 36 [14.3%], p = 0.008), and pre-intervention antegrade flow (48 [70.6%] v 104 [41.3%], p < 0.001) were more common in RVOTI. Significant center differences were noted (p < 0.001). Adjusted survival to CR by 18 months (HR = 0.87, 95% CI = 0.63–1.21, p = 0.41) and overall survival (HR = 2.08, 95% CI = 0.93–4.65, p = 0.074) were similar. RVOTI had increased interstage reintervention (HR = 2.15, 95% CI = 1.36–3.99, p = 0.001). Total anesthesia (243 [213, 277] v 328 [308, 351] minutes, p < 0.001) and cardiopulmonary bypass times (117 [103, 132] v 151 [143, 160] minutes, p < 0.001) favored RVOTI. In this multicenter comparison of physiologic palliation strategies for sTOF, survival to successful CR and overall survival were similar; however, reintervention burden was significantly higher in RVOTI.




Similar content being viewed by others
References
Blalock A, Taussig HB (1945) The surgical treatment of malformations of the heart: in which there is pulmonary stenosis or pulmonary atresia. JAMA 128:189–202. https://doi.org/10.1001/jama.251.16.2123
Slusmans T, Neven B, Rubay J, Lintermans J, Ovaert C, Mucumbitsi J, Shango P, Stijns M, Wliers A (1995) Early balloon dilatation of the pulmonary valve in infants with tetralogy of Fallot Risks and benefits. Circulation 91:1506–1511. https://doi.org/10.1161/01.cir.91.5.1506
Muneuchi J, Watanabe M, Sugitani Y, Kawaguchi N, Matsuoka R, Ando Y, Ochiai Y (2020) Early palliative balloon pulmonary valvuloplasty in neonates and young infants with tetralogy of Fallot. Heart Vessels 35:252–258. https://doi.org/10.1007/s00380-019-01468-0
Sreeram N, Saleem M, Jackson M, Peart I, McKay R, Arnold R, Walsh K (1991) Results of balloon pulmonary valvuloplasty as a palliative procedure in tetralogy of Fallot. J Am Coll Cardiol 18:159–165. https://doi.org/10.1016/s0735-1097(10)80235-9
Lizano santamaria RW, Gillespie MJ, Dori Y, Rome JJ, Glatz AC (2015) Palliative balloon pulmonary valvuloplasty for infants with unrestrictive ventricular septal defect or single ventricle associated with severe pulmonary stenosis. Catheter Cardiovasc Interv 86:829–833. https://doi.org/10.1002/ccd.26083
Sandoval JP, Chaturvedi RR, Benson L, Morgan G, Van Arsdell G, Honjo O, Caldarone C, Lee KJ (2016) Right ventricular outflow tract stenting in tetralogy of Fallot Infants with risk factors for early primary repair. Circ Cardiovasc Interv 9:e003979. https://doi.org/10.1161/CIRCINTERVENTIONS.116.003979
Quandt D, Ramchandani B, Penford G, Stickley J, Bhole V, Mehta C, Jones T, Barron DJ, Stumper O (2017) Right ventricular outflow tract stent versus BT shunt palliation in tetralogy of Fallot. Heart 103:1985–1991. https://doi.org/10.1136/heartjnl-2016-310620
Quandt D, Ramchandani B, Stickley J, Mehta C, Bhole V, Barron DJ, Stumper O (2017) Stenting of the right ventricular outflow tract promotes better pulmonary arterial growth compared with modified blalock-taussig shunt palliation in tetralogy of Fallot-type lesions. JACC Cardiovasc Interv 10:1774–1784. https://doi.org/10.1016/j.jcin.2017.06.023
Zhang H, Fan X, Su J, Liu Y, Zhao L, Li G (2019) The efficiency of systemic-to-pulmonary shunts in older children with hypoplastic pulmonary arteries. J Card Surg 34:463–467. https://doi.org/10.1111/jocs.14063
Bradley SM, Erdem CC, Hsia TY, Atz AM, Bandisode V, Ringewald JM (2008) Right ventricle-to-pulmonary artery shunt: alternative palliation in infants with inadequate pulmonary blood flow prior to two-ventricle repair. Ann Thorac Surg 86:183–188
Korbmacher B, Heusch A, Sunderdiek U, Gams E, Rammos S, Langenbach MR, Schipke JD (2005) Evidence for palliative enlargement of the right ventricular outflow tract in severe tetralogy of Fallot. Eur J Cardiothorac Surg 27:945–948. https://doi.org/10.1016/j.ejcts.2005.02.010
Selmonosky CA, Farhangian D, Folger GM, Ellison RG (1972) Palliative shunting operations in tetralogy of Fallot. Effects upon the results of total correction. Ann Thorac Surg 14:16–23. https://doi.org/10.1016/s0003-4975(10)65192-2
Glatz AC, Petit CJ, Goldstein BH, Kelleman MS, McCracken CE, McDonnell A, Buckey T, Mascio CE, Shashidharan S, Ligon RA, Ao J, Whiteside W, Wallen WJ, Metcalf CM, Aggarwal V, Agrawal H, Qureshi AM (2018) Comparison between patent ductus arteriosus stent and modified blalock-taussig shunt as palliation for infants with ductal-dependent pulmonary blood flow: insights from the congenital catheterization research collaborative. Circulation 137:589–601. https://doi.org/10.1161/CIRCULATIONAHA.117.029987
Ratnayaka K, Nageotte SJ, Moore JW, Guyon PW, Bhandari K, Weber RL, Lee JW, You H, Griffin DA, Rao RP, Nigro JJ, El-Said HG (2021) Patent ductus arteriosus stenting for all ductal-dependent cyanotic infants: waning use of blalock-taussig shunts. Circ Cardiovasc Interv 14:e009520. https://doi.org/10.1161/CIRCINTERVENTIONS.120.009520
Bentham JR, Kava NK, Harrison WJ, Shauq A, Kalantre A, Derrick G, Chen RH, Dhillon R, Taliotis D, Kang SL, Crossland D, Adesokan A, Hermuzi A, Kudumula V, Yong S, Noonan P, Hayes N, Stumper O, Thomason JDR (2018) Stenting versus modified Blalock-Taussig shunt in neonates with duct dependent pulmonary blood flow: associations with clinical outcomes in a multicenter national study. Circulation 137:581–588. https://doi.org/10.1161/CIRCULATIONAHA.117.028972
Ohye RG, Ludomirsky A, Devaney EJ, Bove EL (2004) Comparison of right ventricle to pulmonary artery conduit and modified Blalock-Taussig shunt hemodynamics after the Norwood operation. Ann Thorac Surg 78:1090–1093. https://doi.org/10.1016/S0003-4975(03)01386-9
Petrucci O, O’Brien SM, Jacobs ML, Jacobs JP, Manning PB, Eghtesady P (2011) Risk factors for mortality and morbidity after the neonatal Blalock-Taussig shunt procedure. Ann Thorac Surg 92:642–651 (discussion 51–2)
Godart F, Qureshi SA, Simha A, Deverall PB, Anderson DR, Baker EJ, Tynan M (1998) Effects of modified and classic Blalock-Taussig shunts on the pulmonary arterial tree. Ann Thorac Surg 66:512–7 (discussion 8)
Goldstein BH, Petit CJ, Qureshi AM, McCracken CE, Kelleman MS, Nicholson GT, Law MA, Meadows JJ, Zampi JD, Shabanavaz S, Mascio CE, Chai PJ, Romano JC, Batlivala SP, Maskatia SA, Asztalos IB, Kamsheh AM, Healan SJ, Smith JD, Ligon RA, Pettus JA, Juma S, Raulston JEB, Hock KM, Pajk AL, Eilers LF, Khan HQ, Merritt TC, Canter M, Jerugensen S, Rinderknecht FA, Bauser-Heaton H, Glatz AC (2021) Comparison of management strategies for neonates with symptomatic tetralogy of Fallot. J Am Coll Cardiol 77:1093–1106. https://doi.org/10.1016/j.jacc.2020.12.048
Petit CJ, Qureshi AM, Glatz AC, McCracken CE, Kelleman M, Nicholson GT, Meadows JJ, Shahanavaz S, Zampi JD, Law MA, Pettus JA, Goldstein BH (2019) Comprehensive comparative outcomes in children with congenital heart disease: the rationale for the congenital catheterization research collaborative. Congenit Heart Dis 14:341–349. https://doi.org/10.1111/chd.12737
Pettus JA, Pajk AL, Glatz AC, Petit CJ, Goldstein BH, Qureshi AM, Nicholson GT, Meadows JJ, Zampi JD, Law MA, Shahanavaz S, Kelleman MS, McCracken CM, Congenital Cardiac Research Collaborative (2021) Data quality methods through remote source data verification auditing: results from the Congenital Cardiac Research Collaborative. Cardiol Young 31:1829–1834. https://doi.org/10.1017/S1047951121000974
Nakata S, Imai Y, Takanashi Y, Kurosawa H, Tezuka K, Nakazawa M, Ando M, Takao A (1984) A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg 88:610–619
Meadows JJ, Qureshi AM, Goldstein BH, Petit CJ, McCracken CE, Kelleman MS, Aggarwal V, bauser-Heaton H, Combs CS, Gartenberg AJ, Ligon RA, Nicholson GT, Galtz AC (2019) Comparison of Outcomes at Time of Superior Cavopulmonary Connection Between Single Ventricle Patients With Ductal-Dependent Pulmonary Blood Flow Initially Palliated With Either Blalock-Taussig Shunt or Ductus Arteriosus Stent: Results From the Congenital Catheterization Research Collaborative. Circ Cardiovasc Interv 12:e008110. https://doi.org/10.1161/CIRCINTERVENTIONS.119.008110
Mair R, Tulzer G, Sames E, Gitter R, Lechner E, Steiner J, Hofer A, Geiselseder G, Gross C (2003) Right ventricular to pulmonary artery conduit instead of modified Blalock-Taussig shunt improves postoperative hemodynamics in newborns after the Norwood operation. J Thorac Cardiovasc Surg 126:1378–1384. https://doi.org/10.1016/s0022-5223(03)00389-1
Rhodes J, O’Brien S, Patel H, Cao QL, Banerjee A, Hijazi ZM (2000) Palliative balloon pulmonary valvuloplasty in tetralogy of fallot: echocardiographic predictors of successful outcome. J Invasive Cardiol 12:448–451
Quandt D, Penford G, Ramchandani B, Bhole V, Mehta C, Stumper O (2017) Stenting of the right ventricular outflow tract as primary palliation for Fallot-type lesions. J Congenit Cardiol 1:3
Savla JJ, Faerber JA, Huang YV, Zaoutis T, Goldmuntz E, Kawut SM, Mercer-Rosa L (2019) 2-Year outcomes after complete or staged procedure for tetralogy of Fallot in neonates. J Am Coll Cardiol 74:1570–1579. https://doi.org/10.1016/j.jacc.2019.05.057
Qureshi AM, Caldarone CA, Romano JC, Chai PJ, Mascio CE, Glatz AC, Petit CJ, McCracken CE, Kelleman MS, Nicholson GT, Meadows JJ, Zampi JD, Shabanavaz S, Law MA, Batlivala SP, Goldstein BH (2021) Comparison of management strategies for neonates with symptomatic tetralogy of Fallot and weight<2.5 kg. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2021.01.100
Daliento L, Mapelli D, Russo G, Scarso P, Limongi F, Iannizzi P, Melendugno A, Mazzotti E, Volpe B (2005) Health related quality of life in adults with repaired tetralogy of Fallot: psychosocial and cognitive outcomes. Heart 91:213–218. https://doi.org/10.1136/hrt.2003.029280
Acknowledgements
We thank Joelle Pettus for her tireless efforts in the management of the Congenital Cardiac Research Collaborative. The collaborative acknowledges and would like to thank the Children’s Healthcare of Atlanta and Emory University Pediatrics Biostatics Collaboration Core for their continued expertise and support. The Congenital Cardiac Research Collaborative Investigators Collaborators include Lindsay F. Eilers, MD, and Hala Q. Khan, BSc (The Lillie Frank Abercrombie Section of Cardiology, Texas Children’s Hospital and Department of Pediatrics, Baylor College of Medicine, Houston, TX); Justin D. Smith (C.S. Mott Children’s Hospital, Ann Arbor, MI); Ivor B. Asztalos, MD, MSCE, and Alicia M. Kamsheh, MD (Children’s Hospital of Philadelphia, Philadelphia, PA); R. Allen Ligon, MD, and Sarina Juma, MPH, (Children’s Healthcare of Atlanta, Department of Pediatrics, Emory University School of Medicine, Atlanta, GA); Stephan Juergensen, MD, and Fatuma Ayann Rinderknecht, BA, (University of California, San Francisco, San Francisco, CA); Taylor C Merritt RN BSN, and Matthew Candor MET (St Louis Children’s Hospital, St. Louis, MO); Amy L Pajk, MBA, CCRP (Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH); Steven J. Healan, MD, MSCI, (Division of Cardiology, Department of Pediatrics, Vanderbilt University School of Medicine, Nashville TN).
Funding
Funding for this project was provided by the author’s respective institutions and in part by the generous support from the member institutions of the collaborative as well as the Kennedy Hammill Pediatric Cardiac Research Fund, The Liam Sexton Foundation, and A Heart Like Ava. Dr. Goldstein receives consulting fees from Medtronic, W.L. Gore & Associates, Mezzion Pharma and PECA labs.
Author information
Authors and Affiliations
Consortia
Contributions
All authors listed on this paper contributed significantly to the planning, conduct, and reporting of the work described in this article. Drs Law and Qureshi are responsible for the overall content and are the guarantors for this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or non-financial interests to declare.
Informed Consent
Cincinnati Children’s Hospital Institutional Review Board (single-institutional review board of record for each of the participating centers) approved the study and informed consent was waived.
Disclosure
Dr Glatz has served as a consultant for Ampio Pharmaceuticals. Dr Goldstein has served as a consultant for Medtronic, W.L. Gore & Associates, and Mezzion PharmaMedtronic, and has served as a consultant and on the advisory board for PECA Labs. Dr Qureshi has served as a consultant for Medtronic, W.L. Gore & Associates, Edwards Lifesciences, and Abiomed. Dr Shahanavaz has served as a consultant for Medtronic, Edwards Lifesciences, W.L Gore & Associates, and Abbott Inc. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Congenital Cardiac Research Collaborative (CCRC) Investigators are listed in the acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Law, M.A., Glatz, A.C., Romano, J.C. et al. Palliation Strategy to Achieve Complete Repair in Symptomatic Neonates with Tetralogy of Fallot. Pediatr Cardiol 43, 1587–1598 (2022). https://doi.org/10.1007/s00246-022-02886-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02886-0