Burden of tuberculosis and its association with socio-economic development status in 204 countries and territories, 1990–2019
- 1Department of Burns and Plastic and Wound Repair Surgery, Xiang'an Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
- 2School of Medicine, Xiamen University, Xiamen, China
- 3Department of Clinical Laboratory, Shanghai Ninth people's Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
- 4Division of Plastic Surgery, The First Affiliated Hospital of Xiamen University, Xiamen, China
- 5Department of Plastic Surgery, Zhongshan Hospital, Fudan University, Shanghai, China
- 6Department of Otolaryngology, Eye Ear Nose and Throat Hospital, Fudan University, Shanghai, China
Background: Tuberculosis (TB) always runs in the forefront of the global burden when it comes to infectious diseases. Tuberculosis, which can lead to impairment of quality of life, financial hardship, discrimination, marginalization, and social barriers, is a major public health problem. The assessment of TB burden and trend can provide crucial information for policy decision and planning, and help countries in the world to achieve the goal of sustainable development of ending the epidemic of TB in 2030.
Methods: All data are from the Global Burden of Disease 2019 (GBD 2019) database, which analyzed the burden trend of age-standardized incidence, DALYs, and deaths rate in TB and HIV/AIDS-infected TB over the past 30 years. Also, GBD 2019 not only analyzed the burden distribution of TB in 204 countries and main regions of the world but also analyzed the relationship between the burden of global TB and the socio–demographic Index (SDI).
Results: The age-standardized incidence, age-standardized disability-adjusted life years (DALYs), and age-standardized deaths rate for HIV-negative TB were 10,671.45 (9,395.60–12,194.10), 59,042.45 (53,684.78–64,641.53), and 1,463.62 (1,339.24–1,602.71) (95% CI, per 100,000 person-years) in 2019, respectively. Age-standardized incidence, age-standardized DALYs, and age-standardized deaths rate of HIV/AIDS-XDR-TB (95% CI, per 1,000 person-years) were 2.10 (1.51–2.90), 64.23 (28.64–117.74), and 1.01 (0.42–1.86), respectively. We found that TB is inversely proportional to SDI, the age-standardized incidence, DALYs, and deaths rate low burden countries were in high SDI areas, while high burden countries were in low SDI areas. The global TB showed a slow decline trend, but the age-standardized incidence of HIV-positive TB was increasing, and mainly distributed in sub-Saharan Africa.
Conclusion: Age-standardized incidence, age-standardized DALYs, and age-standardized deaths rate of TB is related to SDI, and the burden of low SDI countries is lighter than that of high SDI countries. Without effective measures, it will be difficult for countries around the world to achieve the goal of ending the TB epidemic by 2030. Effective control of the spread of TB requires concerted efforts from all countries in the world, especially in the countries with low SDI, which need to improve the diagnosis and preventive measures of TB and improve the control of HIV/AIDS-TB.
Introduction
Tuberculosis is an ancient disease. In 1882, Robert Koch announced the discovery of the main bacterium of TB and named it Mycobacterium TB (1). Tuberculosis is caused by the Bacillus Mycobacterium TB, which is mainly transmitted through air. About one-fourth of the world's population is infected with Mycobacterium TB (2). Over the past 25 years, TB has been the leading cause of global adult infectious diseases and has been regarded as a worldwide public health emergency (3). Tuberculosis is the leading cause of death (single infectious source disease), ranking higher than HIV/AIDS, and is one of the 10 leading causes of death worldwide (2). Tuberculosis is a disease of poverty. People affected by TB often face financial difficulties, marginalization, and discrimination (2). According to WHO estimates, in 2019, there were 10.0 million (8.9–11.0) TB cases in the world, about 8.2% of them were HIV infected patients, about 1.2 million (1.1–1.3) of HIV-negative TB patients died, and 208,000 (177,000–242,000) HIV-positive TB patients died (2).
Although TB has dropped from No. 7 position in 1990 (all ages) [3.1 (2.8–3.4), percentage of DALYs] to the No. 20 position in 2019 [1.9(1.7–2.0), percentage of DALYs] (4). However, it is estimated that the global incidence of TB is slowly decreasing at a rate of 1.6% per year, which is far from reaching the WHO target of 4–5% (5). If the current trend continues, it will be difficult to achieve the 2030 agenda of Sustainable Development Goals (SDGs). Including the goal of ending the TB epidemic, and reducing the number of TB deaths by 90% by 2030, and reducing the incidence of TB by 80% compared with 2015 (including new and relapse cases per 100,000 per year) (2). Evaluating the progress of this goal can provide intuitive and important information for future policy formulation. Many low- and middle-income countries lack high-quality data and high-quality health testing systems. Accurately assessing the burden of TB poses certain challenges (6). The drug-resistant TB not only poses a huge challenge to global TB prevention and control but also is one of the important burdens of TB (7). Individuals who have received the previous treatment are still at high risk of recurrent TB. Follow-up after the treatment and secondary preventive treatment can accelerate the decline in the incidence of TB, and follow-up after the treatment is also very important (8). In addition, innovations in patient-centered strategies and advances in testing and treatment are also critical to ending the TB epidemic (9, 10). Therefore, the prevention and control of TB require joint efforts of prevention, diagnosis, treatment, and follow-up after treatment.
This study can provide the latest data on the age-standardized incidence, DALYs, and mortality of global TB through GBD 2019 data, which is of great significance for the prevention and control of tuberculosis. Combined with age-standardized incidence rates of TB, the association of DALYs and deaths rate analyses with SDI was more reflective of the impact of TB on socioeconomic status. Moreover, the GBD 2019 database can analyze the changes of TB in 204 countries and regions in the past 30 years (1990–2019). The burden of TB is related to many factors, such as gender, location, AIDS, and drug resistance. Analyzing the correlation between TB and these factors through the GBD 2019 database system and updating relevant information in a timely manner will help control the burden of TB and epidemiological trends.
Methods
Overview and data sources
The GBD database is a systematic and scientific work aimed at quantifying the comparative magnitude of health losses caused by diseases, injuries, and risk factors by age, gender, and geographical location. The latest data for estimating age-standardized incidence rate, DALYs rate, and deaths rate of TB were extracted from GBD 2019 (http://ghdx.healthdata.org/gbd-2019). The GBD 2019 includes 369 diseases and injuries in 204 countries or regions around the world as well as more than 80 behavioral, environmental, and other risk factors, whose estimation of attributable burden followed the general framework established for the comparative risk assessment (CRA) (11, 12) used in GBD since 2002. According to the GBD world population, an age-standardized ratio analysis per 100,000 person-years was recorded.
Disability-adjusted life years
The disability-adjusted life years (DALYs) was proposed by Global Burden of Disease to measure the disease burden, whose calculation takes into account the sum of years of life lost (YLL) and years of disability (YLD) for each reason, age, location, duration, gender, and year (11, 13). There has been a detailed description elsewhere for the GBD method used to estimate mortality and DALYs (14, 15).
Socio-demographic index
The SDI (http://ghdx.healthdata.org/gbd-2019) is a comprehensive indicator that reflects the social conditions and population, including per capita income, average years of education, and total fertility rate. The SDI score ranges from 0 to 1, which means that the correspondence relationship from the lowest income, the lowest average years of education, and the highest fertility rate to the highest income, the highest average years of education, and the lowest fertility rate, and each location is assigned an SDI score every year. The SDI was developed for GBD 2015 (16) and updated for GBD 2016 (14, 17). As for GBD 2017, due to the U-shaped pattern of age-specific fertility, the age of total fertility was changed to below 25 years. Similar to GBD 2017, GBD 2019 divides countries and regions into five levels according to SDI: High SDI (>0.81), high-middle SDI (0.70–0.81), middle SDI (0.61–0.69), low-middle SDI (0.46–0.60), and Low SDI (<0.46) (18).
Uncertainty analysis
We adopted the same techniques used elsewhere in the GBD study design to propagate uncertainty (19–21). For all steps, we calculated uncertainty for estimation of incidence, DALYs, and deaths systematically by generating 1,000 draws. The uncertainty was determined from the sampling error and the uncertainty of the model coefficients. We used Software Prism 8.0.1 and Adobe Photoshop 20.0.0 for drawing related graphics. The p < 0.05 (two tailed) was statistically significant. When reporting uncertainty intervals, the 95% UIs were calculated using the 2.5th and 97.5th percentiles of the draw-level values.
Results
Burden of major types of TB
From 1990 to 2019, according to the GBD 2019 age-standardized incidence, DALYs, and deaths rate estimates, all HIV-negative TB including the drug-susceptible tuberculosis (DS-TB), multidrug-resistant tuberculosis without extensive drug resistance (MDR-TB without XDR), and extensively drug-resistant tuberculosis (XDR-TB) were analyzed. The results of age-standardized incidence, DALYs, and deaths rate all show that DS-TB ranks first among the three types of HIV-negative TB, followed by MDR-TB without XDR and XDR-TB (Figures 1A–C; Supplementary Table S1). For HIV/AIDS-positive TB, HIV/AIDS-drug-susceptible tuberculosis (HIV/AIDS-DS-TB) ranks first, followed by MDR-TB without XDR and XDR-TB (Supplementary Figures S1A–C; Supplementary Table S2). In 2019, age-standardized incidence, DALYs, and deaths rate, all HIV-negative TB (95% CI, Supplementary Tables S1–S3) are 10.67 million (9.40–12.19), 59.04 million (53.68–64.64), 1.46 million (1.34–1.60). Regardless of age-standardized incidence and DALYs or age-standardized deaths rate of all HIV-negative TB, men are always higher than women (Figures 1D–F; Supplementary Table S3), and men's age-standardized incidence, DALYs, and deaths rate (95% CI) were 11.96 million (10.52–13.64), 75.05 million (67.57–82.50), 1.97 million (1.79–2.16), respectively; female age-standardized incidence, DALYs, and deaths rates (95% CI) are as follows: 9.49 million (8.30–10.91), 43.70 million (38.59–50.70), 1.01 million (0.88–1.21).
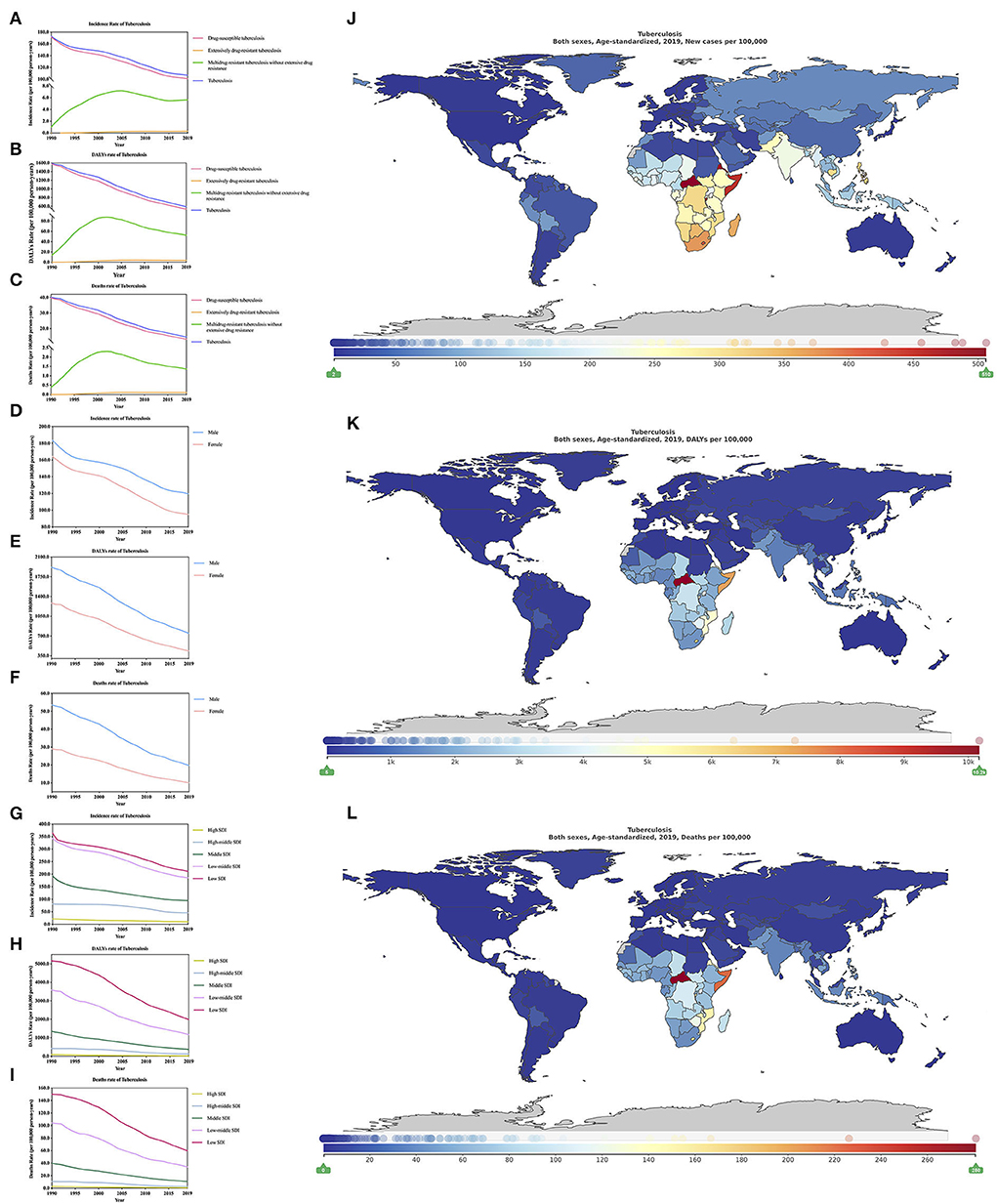
Figure 1. Burden of all HIV-negative tuberculosis for 204 countries and territories. Age-standardized incidence, DALYs, and deaths rate per 100,000 population of tuberculosis stratified by type (A–C), sex (D–F), and SDI (G–I) in global (1990–2019) and the distribution of tuberculosis globally in 2019 (J–L) were generated by GDB 2019.
From 1990–2019, the change of age-standardized incidence, DALYs, and deaths rate of all-HIV negative TB (Supplementary Table S3) have all decreased, respectively, by 38.16% (from −40.73 to −35.26), 62.75% (from −66.61 to −57.98) and 63.49% (−67.62 to −57.85). In addition, the decline of men is lower than that of women (Supplementary Table S3). From 1990 to 2019, we found that regardless of age-standardized incidence, DALYs or deaths rate, the regions with the highest burden of all HIV TB were in low SDI regions, followed by low-middle SDI, middle SDI, high-middle SDI, and high SDI regions (Figures 1G–I; Tables 1–3). In the low SDI regions, age-standardized incidence, DALYs, and deaths rates are 21.15 million (18.74–24.09), 198.31 million (175.76–227.72), 5.99 million (5.33–6.85), respectively; in high SDI regions, age-standardized incidence, DALYs, and deaths rates are 1.01 million (0.87–1.16), 1.97 million (1.77–2.21), 0.07 million (0.06–0.08), respectively. In the low SDI area, the mortality rate accounts for 28.32% of the morbidity, while in the high SDI area, the mortality rate accounts for 6.9% of the morbidity. The mortality/morbidity rate in the low SDI area is more than four times that of the high SDI area. The SDI areas are more likely to die from TB than high SDI areas. In addition, the age-standardized incidence of TB shows that low SDI areas are more than 20 times higher than high SDI areas, age-standardized DALYs, and low SDI areas are more than 100 times higher than high SDI areas. In terms of age-standardized deaths rate, low SDI area is about 85 times that of the high SDI area. Unfortunately, the GBD 2019 data lacks an overall estimate of HIV/AIDS-related TB. Nevertheless, we will discuss in detail the different drug resistance types of HIV/AIDS-related TB. In addition, our age-standardized incidence rates for DS-TB and HIV/AIDS-DS-TB, MDR-TB without XDR and HIV/AIDS-multidrug-resistant tuberculosis without extensive drug resistance (HIV/AIDS-MDR-TB without XDR), XDR-TB and HIV/AIDS-extensively drug-resistant tuberculosis (HIV/AIDS-XDR-TB), respectively, DALYs rate and deaths rate, compared from 1990–2019 change trends, the results show that the HIV-negative group is always higher than the latter (Figures 2A–I, Supplementary Tables S1, S2).
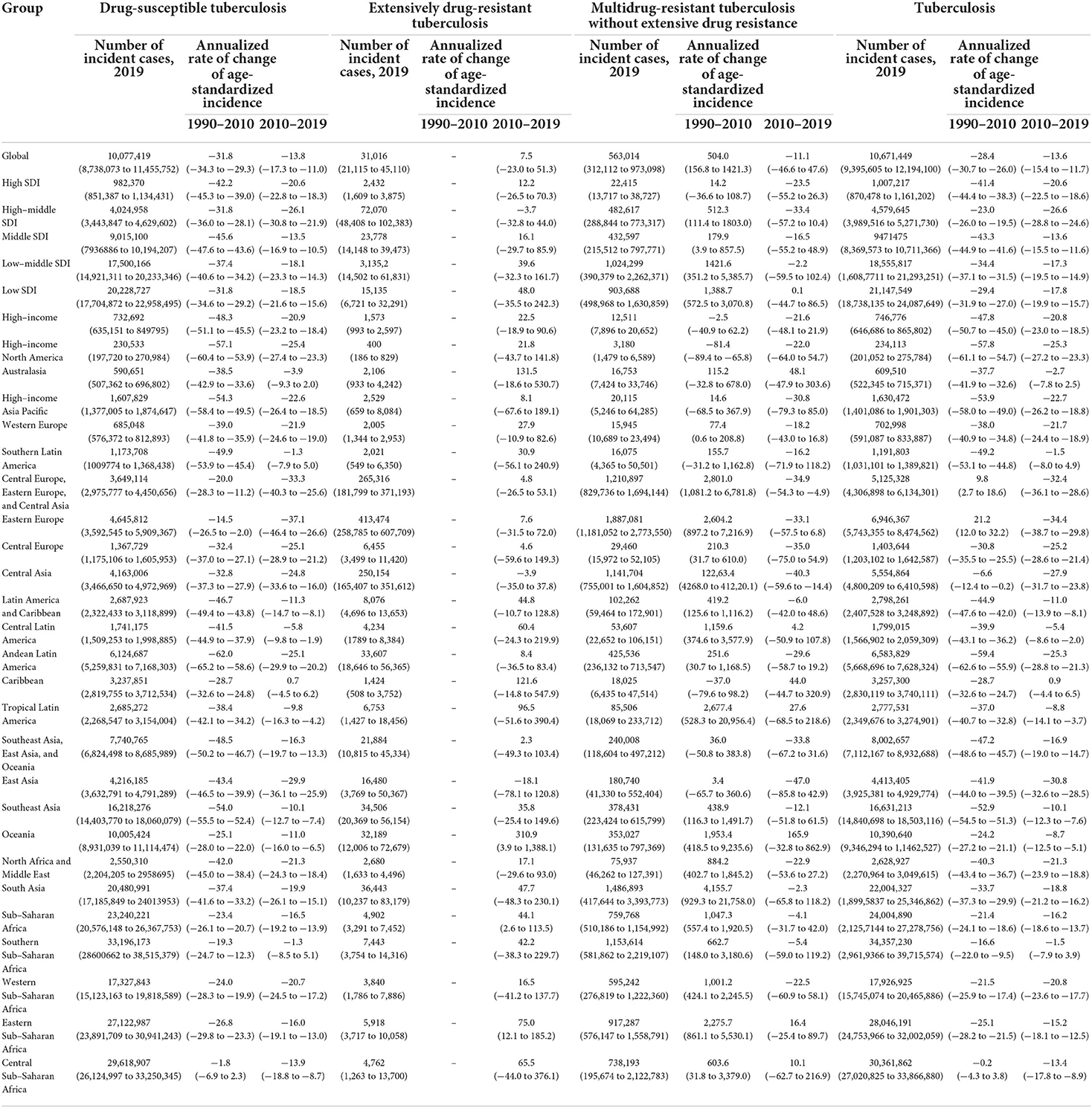
Table 1. Incidence of major HIV-negative individuals in 2019, and change of age-standardized incidence during the periods 1990–2010 and 2010–2019 for both sexes.
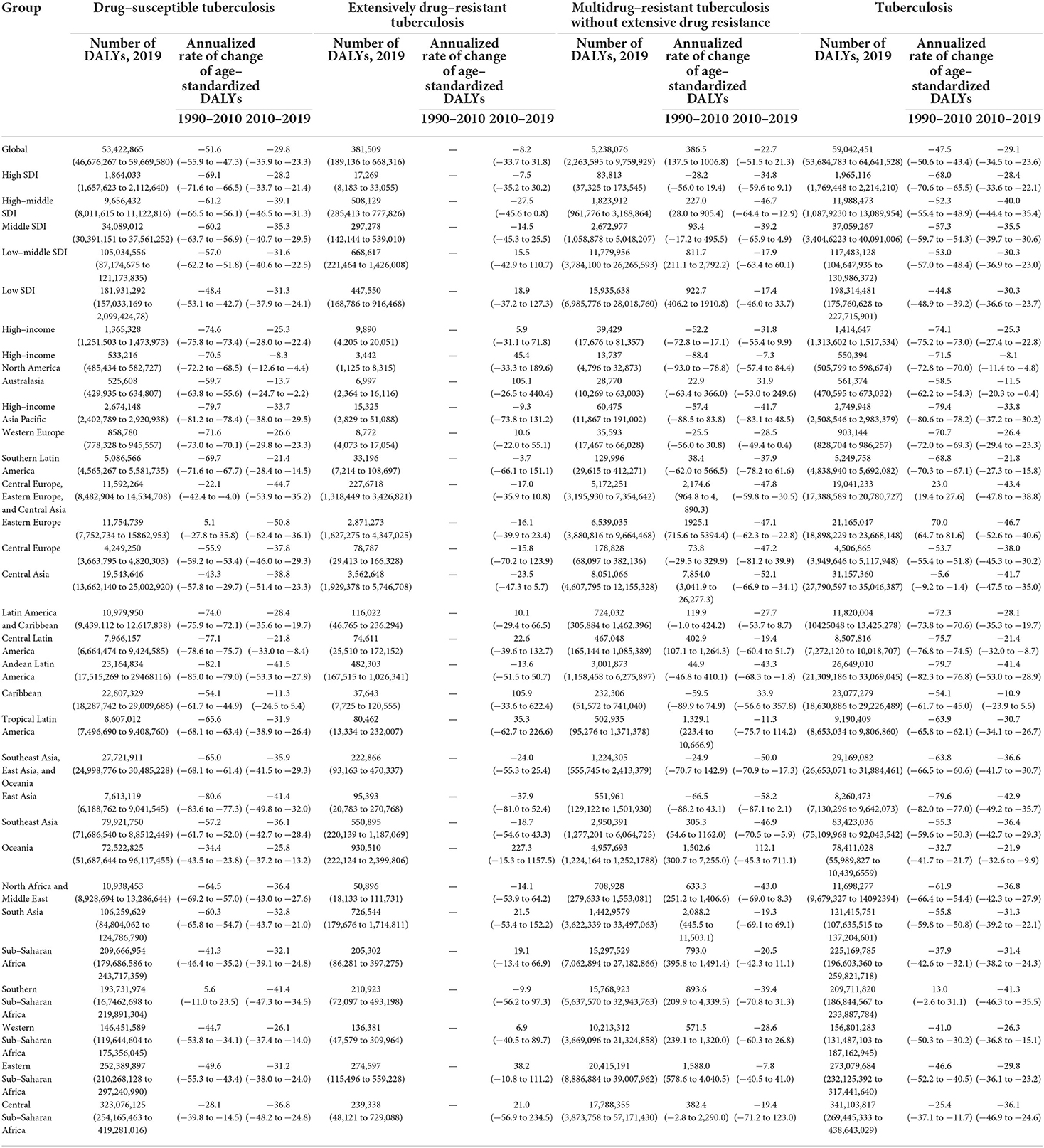
Table 2. The DALYs of major HIV–negative individuals in 2019, and change of age–standardized DALYs during the periods 1990–2010 and 2010–2019 for both sexes.
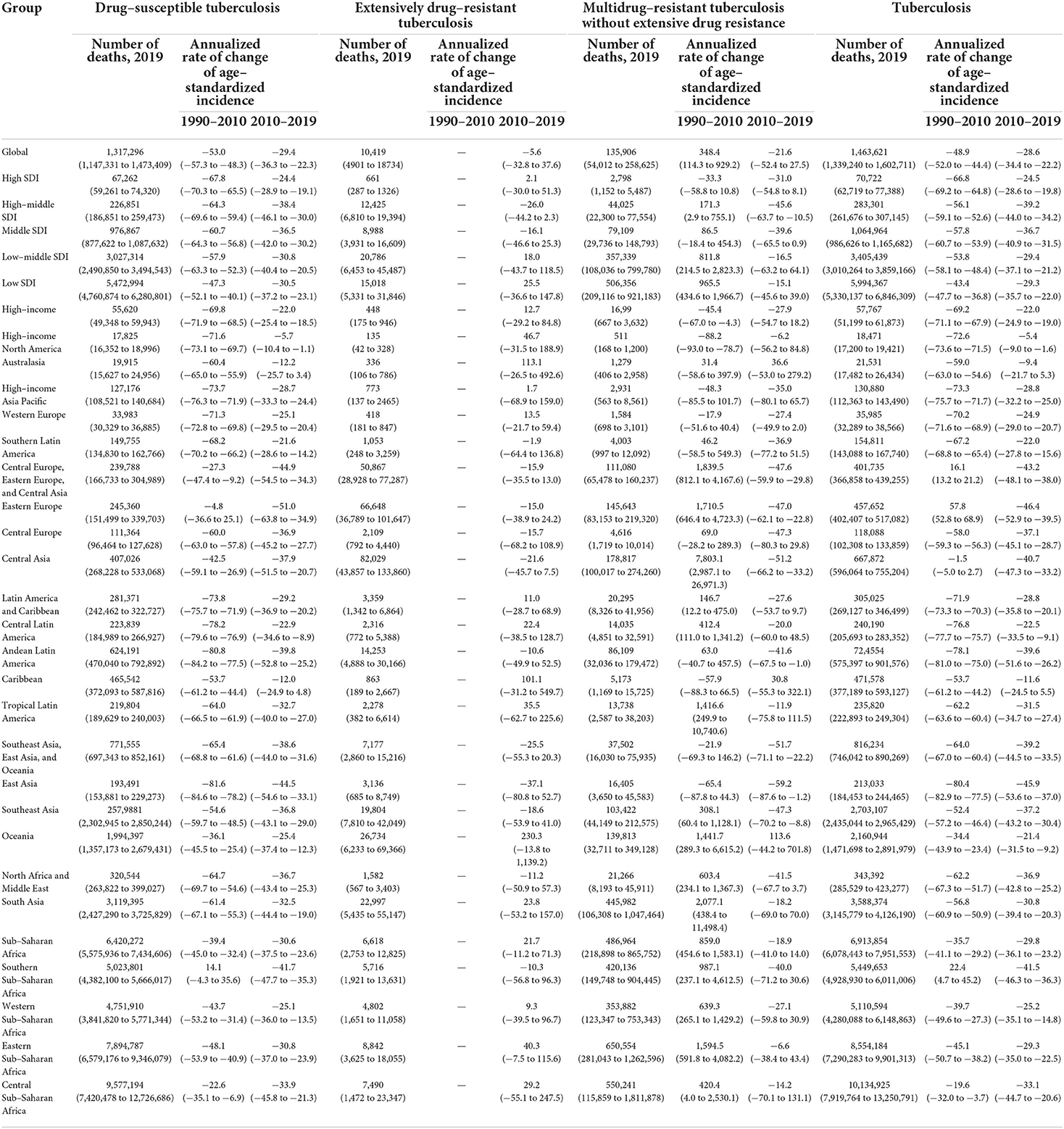
Table 3. Deaths of major HIV–negative individuals in 2019, and change of age–standardized deaths during the periods 1990–2010 and 2010–2019 for both sexes.
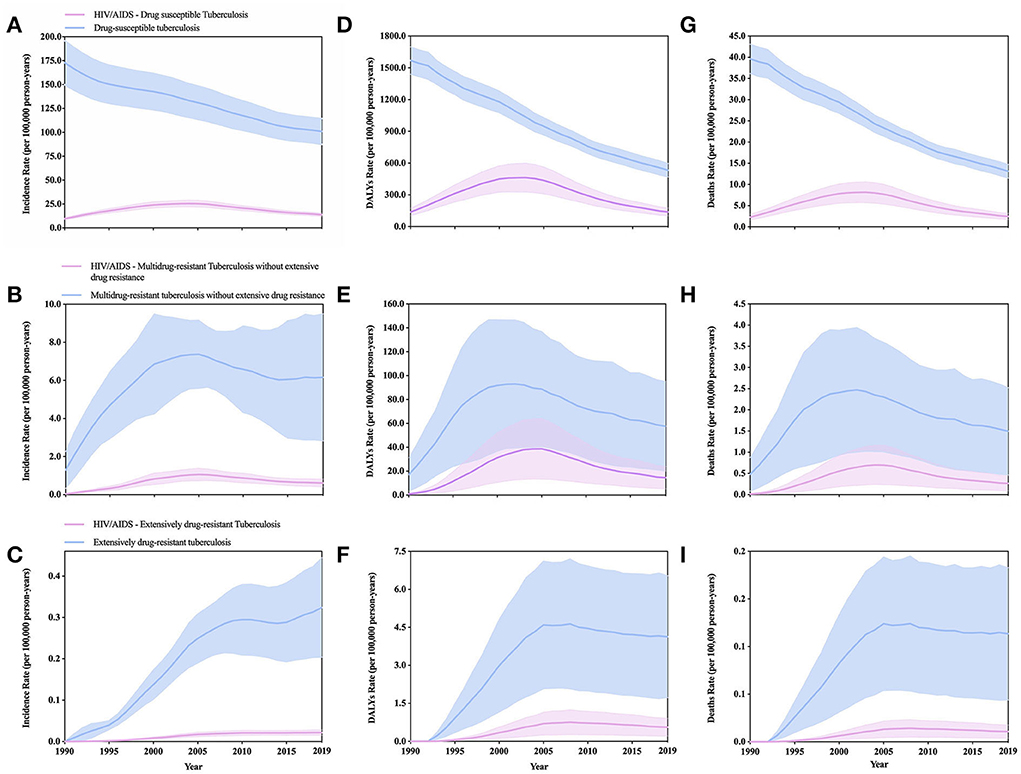
Figure 2. Comparison of major HIV/AIDS-negative and positive tuberculosis burdens estimates (solid lines) and 95% uncertainty intervals (shaded areas) for the age-standardized incidence (A–C), DALYs (D–F), and deaths (G–I) rate per 100,000 population of tuberculosis stratified by HIV/AIDS status in global (1990–2019).
According to GBD 2019, we analyzed the age-standardized incidence of all HIV negative TB in region-specific and country-specific in 2019 (Table 1). Among more than 21 regions in the world, Southern Sub-Saharan Africa has the highest incidence [34.36 million (29.62–39.72)], followed by Sub-Saharan Africa, Central Sub-Saharan Africa, and Eastern Sub-Saharan Africa. In 2019, the regions with the highest age-standardized DALYs and deaths rates are Central Sub-Saharan Africa (341.10 million (269.44–438.64)] (Table 2) and 10.13 million (7.92–13.25)] (Table 3). In short, in 2019, the regions with the highest age-standardized incidence, DALYs, and deaths rates are all in Africa, and the regions with the lowest burden are high-income North America (Tables 1–3), of which the regions with the highest age-standardized deaths rates It is more than 506 times that of low income areas. In 2019, the age-standardized incidence rate, DALYs rate, and deaths rate of all HIV negative TB (Figures 1J–L; Supplementary Tables S4–S6) are the countries with the heaviest burden in the Central African Republic, and their values are 50.62 million (45.98–55.57), 1,017.09 million (742.75–1,344.40), and 28.08 million (20.71–36.56), respectively. The countries with the least burden are the USA, Andorra, and Bermuda.
From 1990 to 2019, the change of age-standardized incidence rate of all HIV-negative TB (Supplementary Table S7) in 204 countries worldwide decreased in almost all countries except Ukraine, which increased by 10.76% (from −0.12 to 24.57). The country with the largest rate of decline is the USA [−72.08% (from −73.90 to −70.28)], and the country with the smallest decline rate is Sweden [−0.22% (from −9.40 to 9.31)]. For the change of age-standardized DALYs rate of all HIV negative TB (Supplementary Table S7), in addition to Lesotho, Zimbabwe, and Ukraine; these three countries showed an upward trend, and the rest of the countries showed a declined trend. The country with the largest decline is Maldives [−92.20% (from −94.06 to 89.14)]. For the change of age-standardized deaths rate of all HIV negative TB (Supplementary Table S7), among which Ukraine, Tajikistan, Lesotho, and Zimbabwe showed an upward trend, and the rest of the countries showed a declined trend. The country with the largest increase was Ukraine [53.26% (22.00–94.57)], and the country with the fastest decline in deaths is Hungary [−92.50% (from −93.91 to −90.77)]. The change of age-standardized deaths rate of all HIV negative TB, almost all countries have decreased, except for Ukraine, which has increased by 10.76% (from −0.12 to 24.57), and the country with the largest decline is the USA [72.08% (from −73.90 to −70.28)]. We analyzed the changes in 204 countries from 1990 to 2010 and from 2010 to 2019 (Tables 1–3). In addition, due to the lack of total HIV-positive TB data in GBD 2019, we are temporarily unable to analyze the global total HIV-positive TB data from the change of age-standardized incidence, DALYs, and deaths rate from 1990 to 2019.
Burden of DS-TB and HIV/AIDS-DS-TB
In 2017, the incidence (in thousands) and prevalence (in thousands) of DS-TB were 8,508.6 (7,808.6–9,371.0) and 9,828.6 (8,860.7–10,773.9), respectively (19). In 2015, there were 1.14 million new cases of HIV-1 and TB co-infection, and nearly 400,000 cases died from co-infection (22). In 2017, the number of HIV/AIDS and drug-susceptible TB co-infection cases reached 132 million (19). The median per capita cost of treating drug-sensitive TB in 2019 was US$860.4. According to the WHO report, the disposable US$6.5 billion in 2020, of which the cost for the diagnosis and treatment of drug-susceptible TB is as high as US$4.2 billion (2).
In 2019, age-standardized incidence, DALYs, and deaths rate of DS-TB (95% CI, Supplementary Table S1) are 10.08 million (8.74–11.46), 53.42 million (46.68–59.67), and 1.32 million (1.15–1.47), respectively. In 2019, age-standardized incidence, DALYs, and deaths rate of HIV/AIDS-DS-TB (95% CI, Supplementary Tables S4–S6) are 1.37 million (1.20–1.56), 13.70 million (10.07–17.57), and 0.24 million (0.17–0.32), respectively. From 1990–2019, age-standardized incidence rate, DALYs rate, and deaths rate of DS-TB, males are higher than females (Figures 3A–C; Supplementary Table S8), for HIV/AIDS-DS-TB, the proportion of females is higher than males (Supplementary Figures S1D–F; Supplementary Table S9). In 2019, the increase in the burden of DS-TB is in the opposite order of the increase in SDI. Low SDI locations record the highest age-standardized incidence, DALYs, and deaths rates of DS-TB. However, in high SDI areas, there are lowest rates (Figures 3D–F; Supplementary Table S10). The increase in the burden of HIV/AIDS-DS-TB has similar results with the trend of SDI and DS-TB (Supplementary Figures S1G–I; Supplementary Table S11).
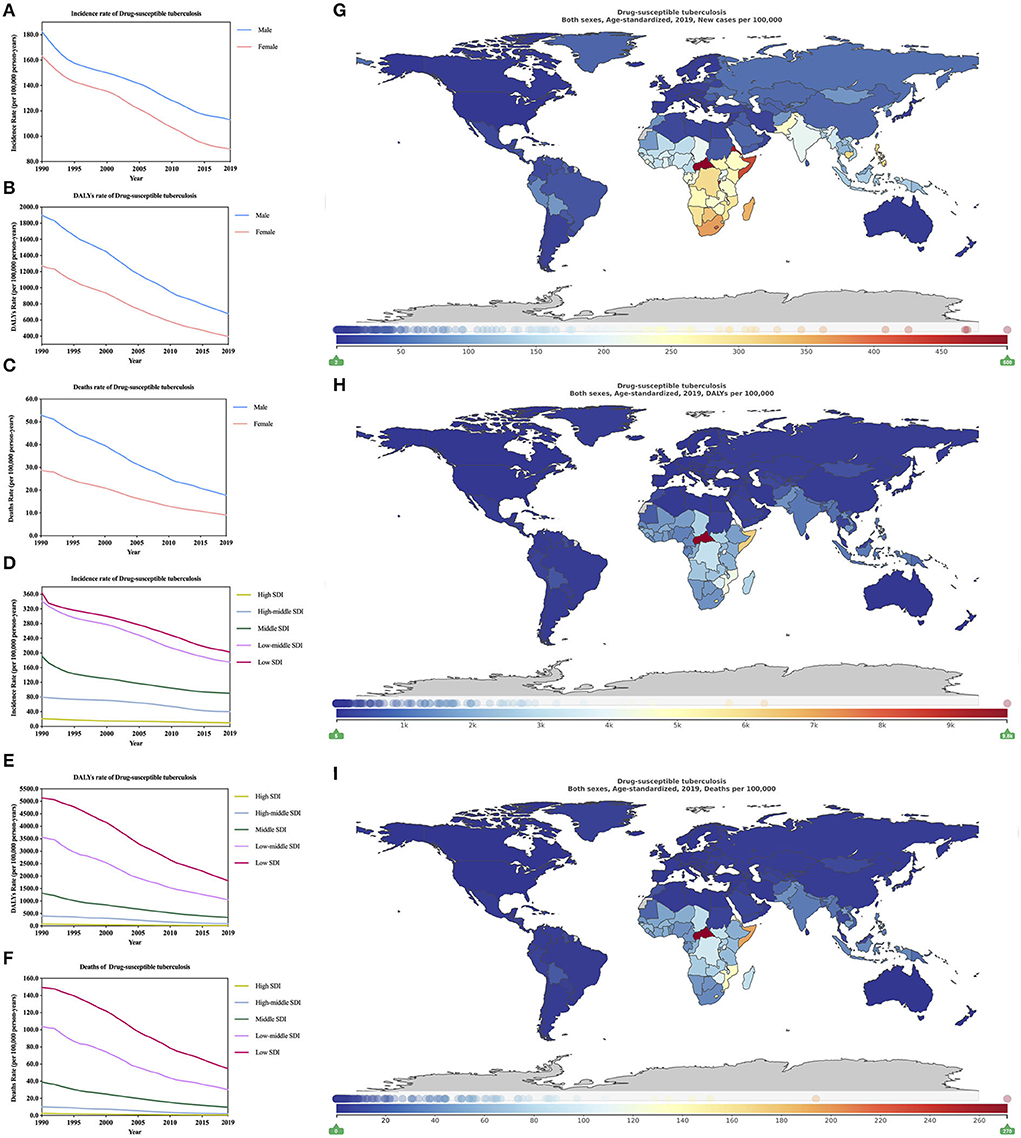
Figure 3. Burden of drug-susceptible tuberculosis for 204 countries and territories. Age-standardized incidence, DALYs, and deaths rate per 100,000 population of drug-susceptible tuberculosis stratified by sex (A–C) and SDI (D–F) in global (1990–2019) and the distribution of drug-susceptible tuberculosis globally in 2019 (G–I) were generated by GDB 2019.
In 2019, in high SDI and low SDI regions, the age-standardized incidence rate of DS-TB (Supplementary Table S10; 1,000 per year) is 982.37 (851.39–1,134.43) and 20,228.73 (17,704.87–22,958.49), respectively, and the low SDI region is high, which is more than 20 times the SDI area. The age-standardized DALYs rate of DS-TB (Supplementary Table S10; 1,000 per year) are 1,864.03 (1,657.62–2,112.64) and 18,193.29 (157,033.17–209,942.48), respectively. The low SDI area is 97 times that of the high SDI area. The age-standardized deaths rate of DS-TB (Supplementary Table S10; 1,000 per year) is 67.26 (59.26–74.32) and 5,472.99 (4,760.87–6,280.80), respectively. The low SDI area is 81 times that of the high SDI area. In 2019, the age-standardized incidence rate of HIV/AIDS-DS-TB (Supplementary Table S11; 1,000 per year) areas with high SDI and low SDI are 30.72 (26.67–35.58) and 3,476.76 (3,037.45–3,977.41), respectively. For age-standardized DALYs rate of HIV/AIDS-DS-TB (Supplementary Table S11; 1,000 per year) are 242.14 (164.86–348.22) and 45,495.49 (34,473.84–56,412.04), respectively. For age-standardized deaths rate of HIV/AIDS-DS-TB (Supplementary Table S11; 1,000 per year) are 5.07 (3.31–7.43) and 891.66 (658.69–1,106.21) respectively. In short, for HIV/AIDS-DS-TB, age-standardized incidence DALYs, and deaths rates in low SDI areas are higher than those in high SDI areas (both are >100 times).
In 2019, among the 21 regions of the world, the highest age-standardized incidence DS-TB of (Table 1) is Southern Sub-Saharan Africa [33.20 million (28.60–38.52)], followed by Central Sub-Saharan Africa and Eastern Sub-Saharan Africa (all >27 million), the region with the lowest burden is high-income North America [0.23 million (0.20–0.27)], the region with the highest burden is more than 142 times that of the lowest region. For age-standardized HIV/AIDS-DS-TB, the region with the highest burden is also Southern Sub-Saharan Africa [39.36 million (30.34–39.36)] (Supplementary Table S12), and the region with the lowest burden is Australasia [140.03 (120.54–164.06), 1,000 per year].
In 2019, for age-standardized DALYs of DS-TB, the region with the highest burden is Central Sub-Saharan Africa [323.07 million (254.17–419.28)], followed by Sub-Saharan Africa and Eastern Sub-Saharan Africa (both are >200 million) (Table 2). For age-standardized DALYs of HIV/AIDS-DS-TB, the region with the highest burden is Southern Sub-Saharan Africa [347.79 million (246.03–460.74)] (Supplementary Table S13). In addition, the area with the lowest burden for age-standardized DALYs of DS-TB and HIV/AIDS-DS-TB is Australasia. In 2019, the region with the highest burden for age-standardized deaths of DS-TB is still Central Sub-Saharan Africa [9.58 million (7.42–12.73)] (Table 3), followed by Eastern Sub-Saharan Africa and Sub-Saharan Africa, the region with the lowest burden is high-income North America. For age-standardized deaths of HIV/AIDS-DS-TB, the highest and lowest burden areas are Southern Sub-Saharan Africa [7.02 million (4.79–9.50)] and Australasia (Supplementary Table S14).
In 2019, the age-standardized incidence rate of DS-TB is different in different countries and regions (Figure 3G; Supplementary Table S4; 1,000 per year). The country with the heaviest burden is the Central African Republic 49,883.99 (45,088.71–54,815.06), followed by Eritrea, Burundi, and the country with the lightest burden is the United States of America [208.72 (177.91–245.42)], and the areas with the heaviest burden are 238 times as many as the areas with light burdens. For age-standardized DALYs (Figure 3H; Supplementary Table S5; 1,000 per year) and deaths rate DS-TB (Figure 3I; Supplementary Table S6; 1,000 per year), the countries with the heaviest burden are the Central African Republic, which are 983,328.10 (717,134.30–1,314,526.54) and 27,131.18 (19,686.98–35,825.78), respectively, the countries with the least burden are Malta [478.23 (382.87–598.79)] and Bermuda [6.38 (5.14–7.98)]. The countries with the highest and lowest age-standardized DALYs burden are 2,056 times the difference. The difference between the countries with the highest and lowest age-standardized deaths burden is 4,283 times. For the age-standardized incidence rate of HIV/AIDS-DS-TB (Supplementary Table S15; 1,000 per year) global distribution is analyzed. The country with the heaviest burden is Lesotho [77,828.41 (65,784.42–91,494.82)], and the country with the lightest burden is Iraq [0.70 (0.59–0.82)]. The age-standardized incidence and deaths rate DS-TB (Supplementary Tables S16, S17; 1,000 per year) also show that the country with the heaviest burden is Lesotho, which is 1,112,636.76 (872,521.60–1,403,125.61)] and 23,229.32 (18,518.84–28,711.45), respectively, the country with the least burden is Iraq, which is 5.44 (3.38–8.61) and 0.08 (0.05–0.14), respectively.
From 1990 to 2019, the change of age-standardized incidence of DS-TB (Supplementary Table S18) has dropped by 41.2% (from −44.4 to −38.3) globally, and all countries have fallen, of which Belarus has the largest decline [73.9% (from −80.7 to −66.9)], Sweden has the smallest decrease [3.1% (from −12.9 to 6.6)]. The change of age-standardized incidence of HIV/AIDS-DS-TB (Supplementary Table S19) is on the rise globally [44.5% (36.2–53.2)], and the existing data shows that 80 countries are on the rise, Mongolia has the largest increase (approximately 56 times). For change of age-standardized DALYs rate of DS-TB (Supplementary Table S18), it shows a downward trend in the world [66.00 (from −70.52 to −61.29]. Except for Lesotho and Zimbabwe, which showed an increasing trend, all other countries showed a downward trend. The largest amplitude is Guatemala [90.0 (from −94.2 to −90.0)]. For change of age-standardized DALYs rate of HIV/AIDS-DS-TB (Supplementary Table S19), the country with the largest increase is Papua New Guinea, which is as high as 105.8 times (95% CI, 35.5–369.3), and the country with the largest decrease is Hungary [95.2% (from −96.0 to −94.4)]. For change of age-standardized deaths rate of DS-TB (Supplementary Table S18) decreased by [41.2% (from −44.4 to −38.3)] globally, except for Lesotho and Zimbabwe, which showed an increasing trend. The rest countries are showing a downward trend, with the largest decline being Hungary [92.7% (from −94.3 to −91.0)]. For change of age-standardized deaths rate of HIV/AIDS-DS-TB (Supplementary Table S19), the country with the largest increase is Papua New Guinea, which is as high as 167.6 times (95% CI, 46.8–4,767.8), and the country with the largest decrease is Hungary [95.5% (from −96.3 to −94.6)]. In addition, more detailed information can be learned through the changes in the 204 countries from 1990 to 2010 and from 2010 to 2019 (Supplementary Tables S4–S6, S15–S17).
Burden of MDR-TB without XDR and HIV/AIDS-MDR-TB without XDR
Globally, 4.6% of TB patients have MDR-TB, but in some regions, such as Kazakhstan, Kyrgyzstan, Moldova, and Ukraine, this proportion exceeds 25% (23). Of the estimated total in 2020, US$8.3 billion (64%) is for diagnosis and treatment of drug-susceptible TB, US$4.3 billion is for diagnosis and treatment of MDR-TB (2). In 2019, age-standardized incidence, DALYs, and deaths rate of MDR-TB without XDR (95% CI, Supplementary Table S1) are 0.56 million (0.31–0.97), 5.24 million (2.64–9.76) and 0.14 million (0.05–0.26). In 2019 age-standardized incidence, DALYs, and deaths rate of HIV/AIDS-MDR-TB without XDR (95% CI, Supplementary Table S3) are 0.06 million (0.04–0.08), 1.34 million (0.58–2.46), and 0.02 million (0.01–0.05), respectively. We found that about one-third of people with HIV-infected MDR-TB without XDR died, which indicates that HIV infection is associated with increased mortality during multi-drug resistance (24).
From 1990 to 2019, the age-standardized incidence rate, DALYs rate, and deaths rate of MDR-TB without XDR between different genders all show that male MDR-TB without XDR is always higher than female (Figures 4A–C, Supplementary Table S20). For age-standardized incidence rate, DALYs rate, and deaths rate of HIV/AIDS-MDR-TB without XDR, women's MDR-TB without XDR is generally higher than men's, which is contrary to the results of MDR-TB without XDR (Supplementary Figures S2A–C; Supplementary Table S21). In 2019, the age-standardized incidence rate of MDR-TB without XDR (Supplementary Table S22; Figure 4D; 1,000 per year) is the low-middle SDI region [1024.30 (390.38–2262.37)], and the least burden is High SDI areas [22.41 (13.72–22.41)], and the incidence of low-middle SDI areas is 45 times that of high SDI areas. For the age-standardized DALYs rate of MDR-TB without XDR (Supplementary Table S22; Figure 4E), the heaviest burden is the low SDI area [15,935.64 (6,985.78–28,018.76)], and the lightest burden is the high SDI area [83.81 (37.32–173.54)], the incidence in low SDI areas is 190 times that of high SDI areas. For the age-standardized deaths rate of MDR-TB without XDR (Supplementary Table S22; Figure 4F), the lowest burden is in low SDI regions [506.36 (209.12–921.18)], and the least burden is in high SDI regions [2.80 (1.15) – 5.49)]. In 2019, the difference from MDR-TB without XDR is the age-standardized incidence rate of HIV/AIDS-MDR-TB without XDR (Supplementary Table S23; Supplementary Figure S2D). The region with the heaviest burden is low SDI [148.38 (92.05–230.78)], and the areas with the least burden are high SDI areas [0.86 (0.56–1.27)]. In addition, the age-standardized incidence rate of MDR-TB without XDR is 6.9 times that of MDR-TB without XDR. Similar to the age-standardized incidence rate of HIV/AIDS-MDR-TB without XDR, age-standardized DALYs and deaths rate of MDR-TB without XDR (Supplementary Table S23; Supplementary Figures S2E,F), the areas with the heaviest burden are low SDI regions are 4,499.35 (1,771.05–8,649.15) and 89.20 (34.64–173.04), respectively; the least burdened regions are high SDI regions, which are 13.29 (5.54–27.29) and 0.28 (0.11–0.57), respectively.
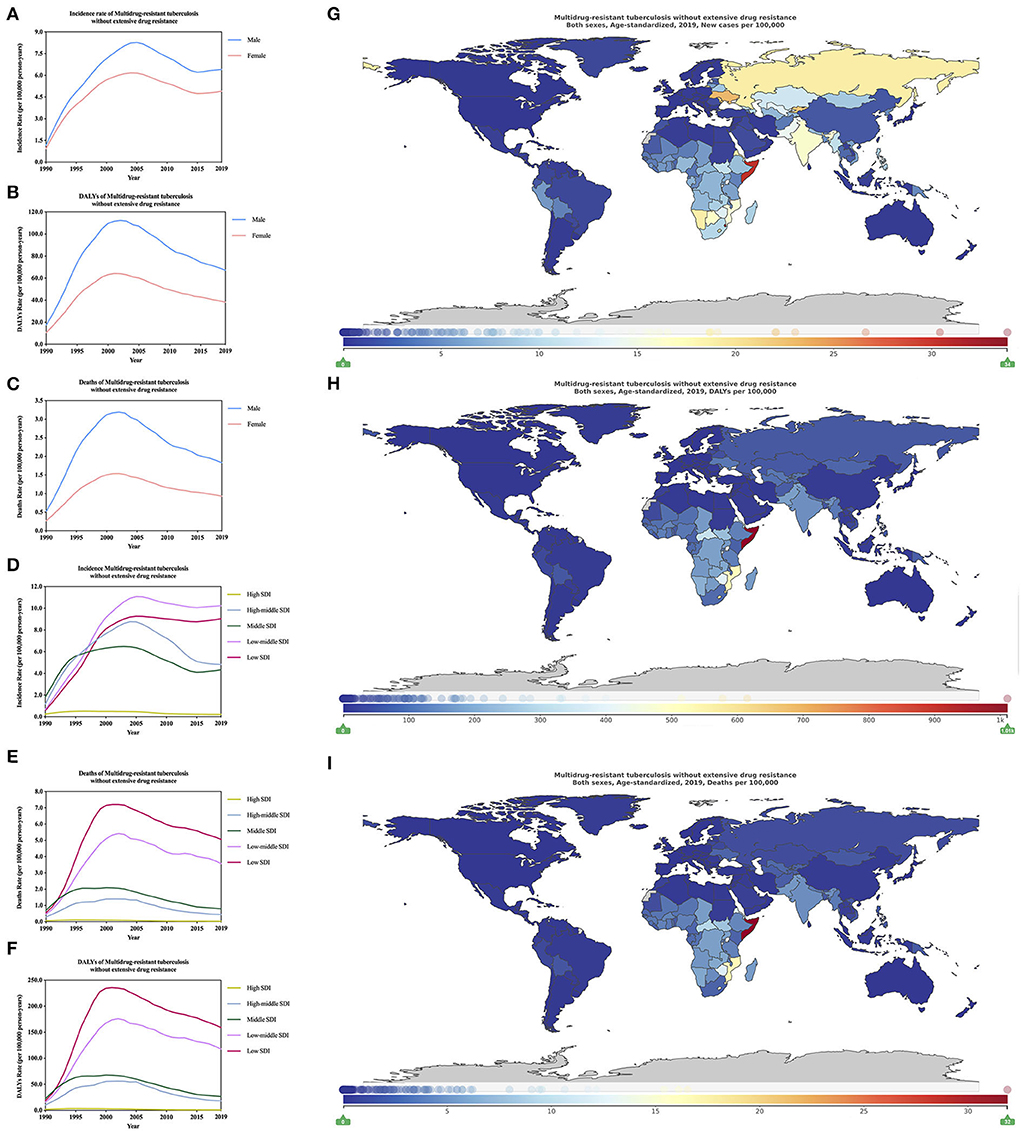
Figure 4. Burden of multidrug-resistant tuberculosis without extensive drug resistance for 204 countries and territories. Age-standardized incidence, DALYs, and deaths rate per 100,000 population of multidrug-resistant tuberculosis without extensive drug resistance stratified by sex (A–C) and SDI (D–F) in global (1990–2019) and the distribution of multidrug-resistant tuberculosis without extensive drug resistance globally in 2019 (G–I) were generated by GDB 2019.
In 2019, the regions with the highest burden of age-standardized incidence rate, DALYs rate, and deaths rate of MDR-TB without XDR are Eastern Europe [1.89 million (1.18–2.78)] (Table 1), Eastern Europe Sub-Saharan Africa [20.42 million (8.87–39.00)] (Supplementary Table S2) and Eastern Sub-Saharan Africa [0.65 million (0.28–1.26)] (Supplementary Table S3), the areas with the lowest burden are high-income North America in 21 regions of the world. For age-standardized incidence rate, DALYs rate, and deaths rate of HIV/AIDS-MDR-TB without XDR, the regions with the highest burden are Southern Sub-Saharan Africa [1.42 million (0.73–2.67)] (Supplementary Table S12), [31.95 million (11.58–65.82)] (Supplementary Table S13), and [0.66 million (0.23–1.38) (Supplementary Table S14), respectively. It is worth mentioning that among the 21 regions in the world, the age-standardized deaths rate of HIV/AIDS-MDR-TB is higher than that of MDR-TB without XDR, and the age-standardized incidence rate of HIV/AIDS-MDR-TB is the lowest. The region is also high-income North America. The regions with the lowest burden of age-standardized DALYs rate and deaths rate are in Australasia.
In 2019, the age-standardized incidence rate of MDR-TB without XDR (Supplementary Table S24; Figure 4G; 1,000 per year) is different in 204 countries. The country with the heaviest burden is Eswatini in Africa [3 386.25 (813.60–8,316.47)], the country with the lightest burden is Slovenia [0.49 (0.07–1.79)], and the highest region is 6,910 times that of the lowest region. The country with the highest burden of age-standardized DALYs and deaths rates of MDR-TB without XDR is Somalia and the values are [101,091.76 (23,053.54–277,892.34)] (Supplementary Table S24; Figure 4H) and [3,189.81 (711.50–8,858.71)] (Supplementary Table S24; Figure 4I), respectively. The least burdened country is Slovenia. For the age-standardized incidence rate of HIV/AIDS-MDR-TB without XDR (Supplementary Table S25; Supplementary Figure S2G), the country with the heaviest burden is Eswatini in southern Africa [7,000.85 (1,657.59–17,734.44)] The country with the lightest burden is Slovenia [0.01 (0.00–0.02)]. For age-standardized DALYs (Supplementary Table S25; Supplementary Figure S2H) and deaths rate of HIV/AIDS-MDR-TB without XDR (Supplementary Table S25, Supplementary Figure S2I) both show that the country with the heaviest burden is Eswatini, respectively, 167,061.73 (38,554.53–362,196.88) and 3,503.48 (792.18–7,698.64); the country with the least burden is Slovenia. HIV/AIDS-MDR-TB without XDR and MDR-TB without XDR have a heavy burden in Africa, and Africa should be a key area for global TB prevention and treatment.
From 1990 to 2019, the change of age-standardized incidence of MDR-TB without XDR (Supplementary Table S26) showed an upward trend in the world, rising by 4.37 times (1.03–14.11), and Slovenia had the largest decline [91.55% (from −99.08 to −18.55)], Kyrgyzstan increased [278.08 times (49.95–3,288.03)]. The change of age-standardized DALYs rate (Supplementary Table S26) of MDR-TB without XDR is on the rise globally [2.76 times (0.59 to 8.61)], and the largest increase is Tajikistan [135.31 times (28.89–1,517.36)] Slovenia [97.02% (from −71.48 to −99.68)] has the most significant decline. The MDR-TB without XDR change of age-standardized deaths rate (Supplementary Table S26) was 2.51 times (0.46–8.00), the largest increase was Tajikistan [162.74 times (35.39 to 1,783.52)], and the decrease was 96.87% (from −99.67 to −70.04). For change of age-standardized incidence of HIV/AIDS-MDR-TB (Supplementary Table S27), it is on the rise globally [15.75 times (8.60–27.41)], and the country with the largest increase is Mongolia (4,399.00 times). For change of age-standardized DALYs rate of HIV/AIDS-MDR-TB (Supplementary Table S27) is on the rise globally [17.36 times (9.10–30.48)], the countries with the largest increase are Djibouti and Papua New Guinea (both are greater than 10,000 times). The HIV/AIDS-MDR-TB change of age-standardized deaths rate (Supplementary Table S27) is on the rise globally, increasing by 18.15 times (9.62–32.15). The countries with the largest increase are Djibouti and Papua New Guinea (both are >14,000 times). Supplementary Tables S4–S6, S15–S17 show in detail the changes in the two phases of 1990–2010 and 2010–2019.
Burden of XDR-TB and HIV/AIDS-XDR-TB
It is noted that XDR-TB, like MDR-TB, remains a major challenge faced by clinicians and staff in global TB prevention and treatment (25). In 2019, age-standardized incidence, DALYs, and deaths rate of XDR-TB (95% CI, Supplementary Table S1; per 1,000 person-years) are 31.01 (21.15–45.11), 38.15 (18.91–66.83), and 10.42 (4.90–18.73), respectively. In 2019, age-standardized incidence, DALYs, and deaths rate of HIV/AIDS-XDR-TB (95% CI, per 1,000 person-years; Supplementary Table S3) are 2.10 [1.51–2.90], 64.23 (28.64–117.74), and 1.01 (0.42–1.86), respectively.
In 1990–2019, age-standardized incidence rate, DALYs rate, and deaths rate of XDR-TB all showed that male XDR-TB is always higher than female (Figures 5A–C; Supplementary Table S28). In 2019, age-standardized incidence rate, DALYs rate, and deaths rate of XDR-TB show (Supplementary Table S28, per 1000 person-years), males are 39.10 (26.83–56.47), 520.45 (261.99–902.84), and 14.73 (7.06–26.12), respectively; females are 23.18 (15.65–34.32), 247.24 (114.94–455.83), and 6.46 (2.86–12.30), respectively. For age-standardized incidence rate, DALYs rate, and deaths rate of HIV/AIDS-MDR-TB without XDR also shows that men are higher than women (Supplementary Figures S3A–C; Supplementary Table S29; per 1,000 person-years). Males are 2.56 (1.81–3.57), 60.95 (26.89–111.33), and 1.19 (0.51–2.19), respectively; females are 1.65 (1.21–2.24), 43.00 (18.76–78.31), and 0.80 (0.35–1.49), respectively. In 2019, the age-standardized incidence rate of XDR-TB (Figure 5D; Supplementary Table S30; per 1,000 person-years) is the area with the heaviest burden in high-middle SDI [72.07 (48.40–102.38)], and the area with the lowest burden, it is the high SDI area [2.43 (1.61–3.87)]. Moreover, the incidence rate in high-middle SDI areas is more than 29 times that of high SDI areas. For age-standardized DALYs rate of XDR-TB (Figure 5E; Supplementary Table S30; per 1,000 person-years), the heaviest burden is the low-middle SDI area [668.62 (221.46–1,426.01)], the least burden is high SDI area [17.27 (8.18–33.060)]. For age-standardized deaths rate of XDR-TB (Figure 5F; Supplementary Table S30; per 1,000 person-years), the area with the heaviest burden is low-middle SDI [20.19 (6.45–45.49)], and the area with the lightest burden is high SDI area [0.66 (0.29–1.33)]. The area with the heaviest burden of mortality is 30 times as much as the area with the least burden, which is consistent with the incidence rate results. In 2019, the age-standardized incidence rate of HIV/AIDS-XDR-TB (Supplementary Figure S3D; Supplementary Table S31; per 1,000 person-years), the highest burden is high-middle SDI area [5.34 (3.41–7.77)], the least burden is high SDI area [0.10 (0.07–0.15)], the heaviest burden is 53 times that of the least burdened area. For age-standardized DALYs rate of HIV/AIDS-XDR-TB (Supplementary Table S3E; Supplementary Figure S31; per 1,000 person-years). The highest burden is in the high-middle SDI area [85.31 (40.72–146.91)], and the lightest burden is also in the high SDI area [3.35 (1.36–6.87)]. For age-standardized deaths rate of HIV/AIDS-XDR-TB (Supplementary Figure S3F; Supplementary Table S31; per 1,000 person-years), the heaviest burden is the high-middle SDI area [1.63 (0.75–2.83)], the least burden is high SDI area [0.07 (0.03–0.15)] In contrast, low SDI regions are not the most affordable regions. This trend is different from DS-TB and MDR-TB without XDR.
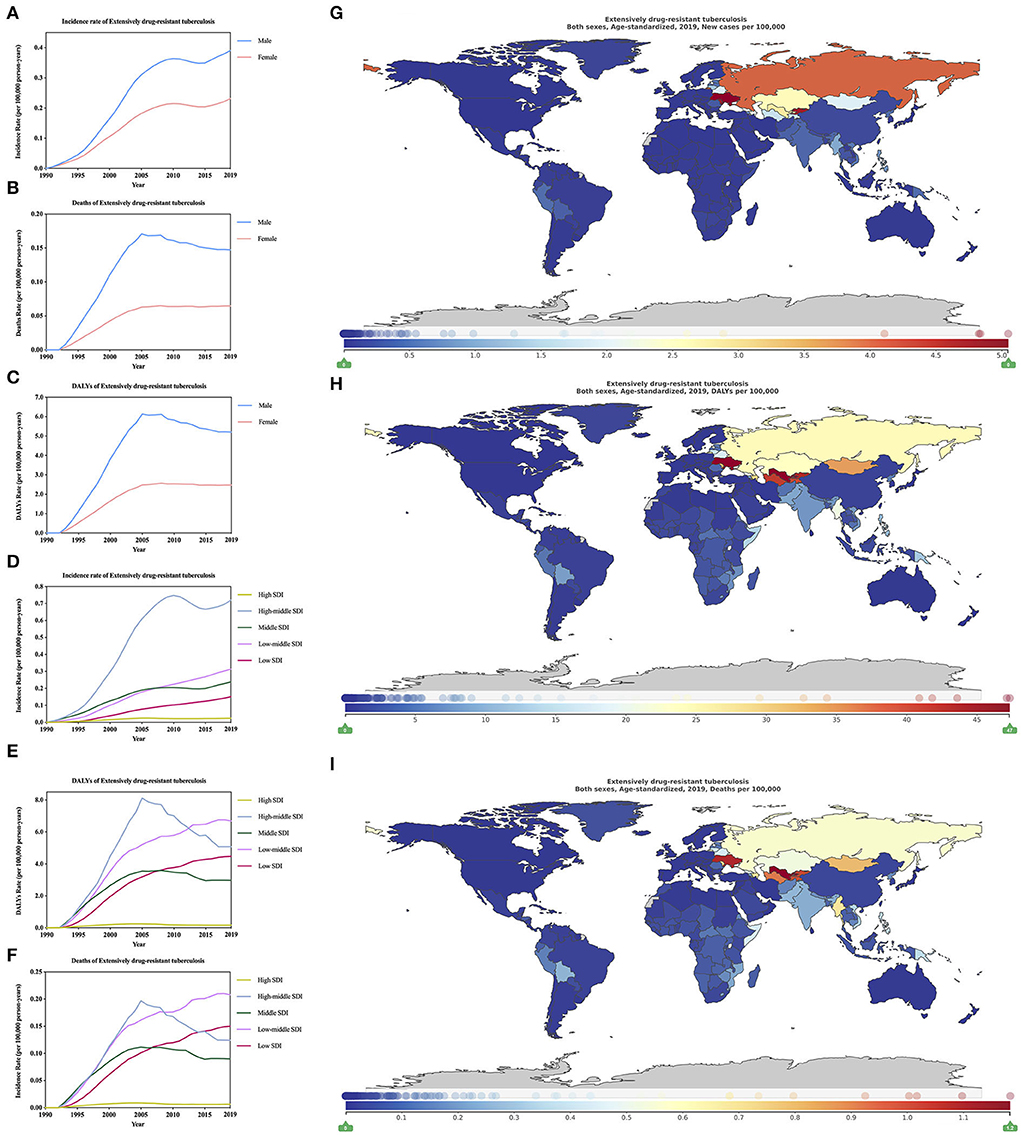
Figure 5. Burden of extensively drug-resistant tuberculosis for 204 countries and territories. Age-standardized incidence, DALYs, and deaths rate per 100,000 population of extensively drug-resistant tuberculosis stratified by sex (A–C) and SDI (D–F) in global (1990–2019) and the distribution of extensively drug-resistant tuberculosis globally in 2019 (G–I) were generated by GDB 2019.
In 2019, among 21 regions in the world (Table 1), the age-standardized incidence of XDR-TB, the highest region is Eastern Europe [0.41 million (0.26–0.61)], For age-standardized incidence of HIV/AIDS-XDR-TB, the highest region is also Southern Sub-Saharan Africa [34.62 million (30.34–39.36)] (Supplementary Table S12). For age-standardized DALYs of XDR-TB, the region with the highest burden is Central Asia [3.56 million (1.93–5.75)], followed by Central Sub-Saharan Africa (Table 2). For age-standardized DALYs of HIV/AIDS-XDR-TB, the region with the highest burden is Southern Sub-Saharan Africa [347.79 million (246.03–460.74)] (Supplementary Table S13). The region with the highest burden for age-standardized deaths of XDR-TB is still Central Asia [0.08 million (0.04–0.13)], followed by Eastern Europe (Table 3). For age-standardized deaths of HIV/AIDS-MDR-TB, the region with the highest burden is Eastern Europe [9.63 (95% CI, 4.46–16.79)] per 1,000 person-years, (Supplementary Table S14). For age-standardized incidence, DALYs, and deaths rate of XDR-TB, the region with the lowest burden is high-income North America, and for age-standardized incidence DALYs, and deaths rate of HIV/AIDS-MDR-TB, the region with the lowest burden is Australasia.
In 2019, the age-standardized incidence rate of XDR-TB (Figure 5G; Supplementary Table S4; per 1,000 person-years) is the country with the heaviest burden in Europe [504.89 (269.41–792.53)], and the country with the least burden is Slovenia [0.11 (0.02–0.39)]. For age-standardized DALYs rate of XDR-TB (Figure 5H; Supplementary Table S5), the country with the heaviest burden is Uzbekistan [4,733.82 (1,820.45–8,760.31)], followed by Ukraine, Kyrgyzstan, Turkmenistan, and the least burden country is Andorra [0.53 (0.05–2.37)]. For age-standardized deaths rate of XDR-TB (Figure 5I; Supplementary Table S6), the country with the heaviest burden is Uzbekistan [118.30 (44.54–220.48)], and the country with the lightest burden is Bermuda. In 2019, age-standardized incidence rate of HIV/AIDS-XDR-TB (Supplementary Figure S3G; Supplementary Table S15), the country with the heaviest burden is Ukraine [58.21 (30.04–93.29)], the country with the lightest burden is Iraq. For age-standardized DALYs, and deaths rate of HIV/AIDS-XDR-TB, the countries with the heaviest burden are Eswatini, 2,261.59 (455.28–5,543.59) (Supplementary Figure S3H; Supplementary Table S16) and 47.94 (9.64–114.62) (Supplementary Figure S3I; Supplementary Table S17), the countries with the least burden are Qatar. In short, unlike XDR-TB, countries with a heavier burden of age-standardized incidence, DALYs, and deaths rate of HIV/AIDS-XDR-TB are basically in Africa.
The GBD 2019 lacks relevant data on 1990–2019 change of age-standardized incidence, DALYs, and deaths rate of XDR-TB and HIV/AIDS-XDR-TB, but we have analyzed the relevant changes from 2010–2019. From 2010 to 2019, the change of age-standardized incidence of XDR-TB (Supplementary Table S4) is on the rise globally [7.51% (from −23.02 to 51.28)], of which Papua New Guinea has increased by 3.07 times (from −1.17 to 14.66) For change of age-standardized DALYs rate of XDR-TB (Supplementary Table S5), there is a downward trend in the world [−8.21% (from −33.68 to 31.82)], with the largest decline in Iceland [79.81% (from −96.02 to −31.56). For change of age-standardized deaths rate of XDR-TB (Supplementary Table S6) globally decreased by 5.62% (from −32.75 to 37.62), the largest decrease was Iceland [−80.57% (from −96.19 to −34.25)]. From 2010–2019, for change of age-standardized incidence of HIV/AIDS-XDR-TB (Supplementary Table S15), there is an upward trend in the world [3.36% (from −23.04 to 38.91)], the largest increase in Comoros [3.24 times [−0.12 to 18.99)]. For change of age-standardized DALYs of HIV/AIDS-XDR-TB (Supplementary Table S16) showed a global downward trend [−21.18% (from −36.02 to −0.97)], the largest decline The country is Iceland [−87.42% (from −97.57 to −59.17)]. For HIV/AIDS-XDR-TB change of age-standardized deaths rate (Supplementary Table S17), the global trend is declining [−19.05% (−34.50 to 1.55)], the country with the largest decline was also Iceland [80.36% (−96.22 to −36.28)].
Discussion
This study evaluated the level and trend of the burden of TB classified by drug resistance type and HIV status in 204 countries and regions in the past 30 years, focusing on the relationship between different types of TB and socioeconomic status (SDI). From 1990 to 2019, the global HIV-negative TB showed a downward trend. The age-standardized incidence rate dropped by 38.15%, the age-standardized DALYs dropped by 62.75%, and the age-standardized deaths rate dropped by 63.49%. However, the age-standardized incidence of HIV-positive TB is increasing, and it is more significant in sub-Saharan Africa. In addition, the age-standardized incidence, DALYs and deaths rates of TB vary greatly from country to country.
The HIV-related TB and drug-resistant TB have become the main burden of drug-resistant TB worldwide. We found that HIV-negative TB is inversely proportional to SDI. Countries with a low burden of age-standardized incidence, DALYs, and deaths rate are in high SDI regions, and countries with high burdens are in low SDI regions. HIV-positive TB (except HIV/AIDS-XDR-TB), age-standardized incidence, DALYs, and deaths rate of HIV/AIDS-DS-TB and HIV/AIDS-MDR-TB countries with the highest burden are in high SDI areas, the burden of the lowest countries are in low SDI regions. The age-standardized incidence of HIV-negative TB in men is higher than that in women. For HIV-positive TB, in addition to HIV/AIDS-XDR-TB, the other two types of HIV-positive TB both show that women are higher than men. Although GBD2017 reported that the global age-standardized incidence rate of HIV-positive TB women is lower than that of men (26), the age-standardized incidence rate of HIV/AIDS-DS-TB and HIV/AIDS-MDR-TB in women is higher than that in men. This may be because women are more susceptible to TB after being infected with HIV than men.
In the past 30 years, the deaths rate of TB has been decreasing year by year, and the prevention and control of TB have achieved remarkable results (25). However, the age-standardized mortality rate in many countries has fallen much faster than the age-standardized morbidity rate. Both AIDS and TB can easily lead to poverty and death, and there is a strong interaction between the two. The incidence of HIV-positive TB is increasing, which reflects that the current prevention and control of HIV-positive TB is facing quite severe challenges, especially in Africa, which is facing the burden of dual infections of AIDS and TB. The previous studies have also concluded that Africa has the highest HIV prevalence rate, and that a large proportion of TB is related to HIV, and the deaths rate of TB among people living with HIV is very high (27). All in all, in terms of TB prevention and control, the African region is currently the focus of global attention (6). While preventing TB, it is necessary to prevent the spread of HIV in a timely manner. Both can be truly controlled under good control.
Although the deaths rate of TB has declined, according to GBD 2019, it is estimated that there will still be about 1.46 million deaths among HIV-negative TB patients worldwide, and about 0.27 million deaths among HIV-positive TB patients in 2019. In HIV-negative and HIV-positive TB, the estimate of GBD 2019 is higher than the estimate of HIV-negative (1.2 million) and HIV-positive TB [208,000] in the WHO2020 report (2). This may be due to the GBD 2019 method of calculating the burden of TB. Unlike the method of the World Health Organization, the estimated value may be different in some regions, so there may be some differences in the global mortality rate. In many countries where TB is endemic, the incidence of TB has either stagnated or declined more slowly than the deaths rate. This indicates that diagnosis and treatment have been delayed. According to the type of TB, appropriate treatment strategies should be adopted to avoid drug resistance (28). The production of sexual TB. Many factors will affect the prevention and control of TB, and there will be unpredictable results. For example, the recent pandemic of coronavirus disease 2019 (COVID-19) may reverse the progress made in TB prevention and control. According to WHO estimates, in 2020 alone, the number of deaths from TB worldwide may increase by 2 to 400,000, and in 2020 (January–June) Several countries (India, Indonesia, Philippines, and South Africa) that account for 44% of global TB have reported a significant drop in the number of confirmed cases, especially India. Indonesia and the Philippines have dropped by 25–30% compared to the same period in 2019 (2). Studies have reported that the cumulative number of deaths from TB in China, India and South Africa affected by COVID-19 is about 0.20 million, and the cumulative number of deaths from TB has increased by 8–14% (29).
Our research still has some limitations. (1) The data in GBD 2019 are estimates, and the lack of overall HIV-positive TB data is not conducive to the assessment of overall HIV-positive TB. (2) In 1990–2010, the data of change of HIV/AIDS-MDR-TB without XDR incidence, DALYs and deaths rate is insufficient in some countries and regions. (3) This study did not analyze the epidemiology of TB, the incidence of TB in various age groups, DALYs and deaths rates, including the status of potentially infected TB. Nevertheless, GBD2019 still shows us a wealth of data for researchers to use, macroscopically showing the trend and burden of TB. We conduct a comprehensive and systematic assessment of the global burden of TB, which provides vital information for reducing the burden of TB.
In 2017, low-income and middle-income countries spent US$10.90 billion (10.3–11.8) on TB and US$20.20 billion (17.0–25.0) on HIV/AIDS (30). World Health Organization predicts that the world's TB will be affected by 2022. At least US$13 billion per year is provided for prevention, diagnosis, treatment, and care (2). Access to treatment may reduce the number of deaths from TB. A lot of funds are still needed to support TB treatment, prevention, and control. Despite a concerted global effort to reduce the burden of TB, it still causes a huge burden of disease globally. Strengthening the health system to detect TB early and improve the quality of TB care, including timely and accurate diagnosis, early initiation of treatment, and regular follow-up are the priorities. In terms of the level of socio–demographic development, countries with a higher incidence of TB than expected should investigate the causes of backwardness and take remedial measures. To achieve the 2035 global target, public health cooperative organizations need to work harder to reduce TB incidence; DALYs, and deaths; expand TB preventive treatment; use new TB treatment options; and prevent and control HIV will help reduce TB (27).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
C-YJ, JiaZ, Z-hF, and YX: study conception and design. YX, JiaZ, PW, and J-hL: data acquisition and analysis. JieZ and B-NX: organize the article table section. W-qL and Y-YF: draw the picture. C-YJ: study supervision. Z-hF: administrative support. YX: drafting the manuscripts. C-YJ, JiaZ, and Z-hF: critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Starting Package of Xiang'an Hospital of Xiamen University (PM201809170010), Open project of Provincial Key Laboratory of Union Hospital Affiliated to Fujian Medical University in 2020 (Nos. XHZDSYS202004 and XHZDSYS202005), and Xiamen municipal Bureau of Science and Technology Grant (3502Z20174079), and the National Natural Science Foundation of China (Grant numbers: 82003178).
Acknowledgments
We thank all contributors to the Global Burden of Diseases 2019 Study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.905245/full#supplementary-material
Abbreviations
DS-TB, Drug-susceptible tuberculosis; MDR-TB without XDR, Multidrug-resistant tuberculosis without extensive drug resistance; XDR-TB, extensively drug-resistant tuberculosis; HIV/AIDS-DS-TB, HIV/AIDS-drug-susceptible tuberculosis; HIV/AIDS-MDR-TB without XDR, HIV/AIDS-multidrug-resistant tuberculosis without extensive drug resistance; HIV/AIDS-XDR-TB, HIV/AIDS-extensively drug-resistant tuberculosis; DALYs, disability-adjusted life years; SDI, sociodemographic Index; COVID-19, coronavirus disease 2019.
References
1. Sakula A. Centenary of the discovery of the Tubercle bacillus. Lancet. (1982) 1:750. doi: 10.1016/S0140-6736(82)92671-X
3. Nathavitharana RR, Friedland JS. A tale of two global emergencies: tuberculosis control efforts can learn from the Ebola outbreak. Eur Respir J. (2015) 46:293–6. doi: 10.1183/13993003.00436-2015
4. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736[20]30925-9
5. Kyu HH, Maddison ER, Henry NJ, Mumford JE, Barber R, Shields C, et al. The global burden of tuberculosis: results from the Global Burden of Disease Study 2015. Lancet Infect Dis. (2018) 18:261–84. doi: 10.1016/S1473-3099(17)30703-X
6. Kyu HH, Maddison ER, Henry NJ, Ledesma JR, Wiens KE, Reiner R, et al. Global, regional, and national burden of tuberculosis, 1990–2016: results from the Global Burden of Diseases, Injuries, and Risk Factors 2016 Study. Lancet Infect Dis. (2018) 18:1329–49. doi: 10.1016/S1473-3099(18)30625-X
7. Lee A, Xie YL, Barry CE, Chen RY. Current and future treatments for tuberculosis. BMJ. (2020) 368:m216. doi: 10.1136/bmj.m216
8. Marx FM, Cohen T, Menzies NA, Salomon JA, Theron G, Yaesoubi R. Cost-effectiveness of post-treatment follow-up examinations and secondary prevention of tuberculosis in a high-incidence setting: a model-based analysis. Lancet Glob Health. (2020) 8:e1223–e33. doi: 10.1016/S2214-109X(20)30227-8
9. Reid MJA, Goosby E. Patient-centered tuberculosis programs are necessary to end the epidemic. J Infect Dis. (2017) 216:S673–S4. doi: 10.1093/infdis/jix373
10. Odone A, Roberts B, Dara M, van den Boom M, Kluge H, McKee M. People- and patient-centred care for tuberculosis: models of care for tuberculosis. Int J Tuberc Lung Dis. (2018) 22:133–8. doi: 10.5588/ijtld.17.0608
11. Murray CJL, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. (1997) 349:1436–42. doi: 10.1016/S0140-6736(96)07495-8
12. Murray CJ, Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S. Comparative quantification of health risks conceptual framework and methodological issues. Popul Health Metr. (2003) 1:1. doi: 10.1186/1478-7954-1-1
13. Mangen MJ, Plass D, Havelaar AH, Gibbons CL, Cassini A, Muhlberger N, et al. The pathogen- and incidence-based DALY approach: an appropriate [corrected] methodology for estimating the burden of infectious diseases. PLoS ONE. (2013) 8:e79740. doi: 10.1371/annotation/caf33818-3453-4e30-b307-7526427b09b7
14. Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
15. Djalalinia S, Saeedi Moghaddam S, Moradi-Lakeh M, Naghavi M, Murray C, et al. Prevalence and years lived with disability of 310 diseases and injuries in Iran and its neighboring countries, 1990-2015: findings from Global Burden of Disease Study 2015. Arch Iran Med. (2017) 20:392–402.
16. Nomura S, Sakamoto H, Glenn S, Tsugawa Y, Abe SK, Rahman MM, et al. Population health and regional variations of disease burden in Japan, 1990–2015: a systematic subnational analysis for the Global Burden of Disease Study 2015. Lancet. (2017) 390:1521–38. doi: 10.1016/S0140-6736(17)31544-1
17. Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1260–344. doi: 10.1016/S0140-6736(17)32130-X
18. Liu C, Wang B, Liu S, Li S, Zhang K, Luo B, et al. Type 2 diabetes attributable to PM2.5: a global burden study from 1990 to 2019. Environ Int. (2021) 156:106725. doi: 10.1016/j.envint.2021.106725
19. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
20. Dicker D, Nguyen G, Abate D, Abate KH, Abay SM, Abbafati C, et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1684–735. doi: 10.1016/S0140-6736(18)31891-9
21. Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
22. Bell LCK, Noursadeghi M. Pathogenesis of HIV-1 and Mycobacterium tuberculosis co-infection. Nat Rev Microbiol. (2018) 16:80–90. doi: 10.1038/nrmicro.2017.128
23. Lange C, Dheda K, Chesov D, Mandalakas AM, Udwadia Z, Horsburgh CR. Management of drug-resistant tuberculosis. Lancet. (2019) 394:953–66. doi: 10.1016/S0140-6736(19)31882-3
24. Bisson GP, Bastos M, Campbell JR, Bang D, Brust JC, Isaakidis P, et al. Mortality in adults with multidrug-resistant tuberculosis and HIV by antiretroviral therapy and tuberculosis drug use: an individual patient data meta-analysis. Lancet. (2020) 396:402–11. doi: 10.1016/S0140-6736(20)31316-7
25. Harding E, WHO. global progress report on tuberculosis elimination. Lancet Respir Med. (2020) 8:19. doi: 10.1016/S2213-2600(19)30418-7
26. Frank TD, Carter A, Jahagirdar D, Biehl MH, Douwes-Schultz D, Larson SL, et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the global burden of diseases, injuries, and risk factors study 2017. Lancet HIV. (2019) 6:e831–e59. doi: 10.1016/S2352-3018(19)30196-1
27. MacNeil A, Glaziou P, Sismanidis C, Date A, Maloney S, Floyd K. Global Epidemiology of tuberculosis and progress toward meeting global targets - worldwide, 2018. MMWR Morb Mortal Wkly Rep. (2020) 69:281–5. doi: 10.15585/mmwr.mm6911a2
28. Tornheim JA, Dooley KE. The global landscape of tuberculosis therapeutics. Annu Rev Med. (2019) 70:105–20. doi: 10.1146/annurev-med-040717-051150
29. McQuaid CF, McCreesh N, Read JM, Sumner T, Group CC-W, Houben R, et al. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur Respir J. (2020) 56. doi: 10.1183/13993003.01718-2020
30. Micah AE, Su Y, Bachmeier SD, Chapin A, Cogswell IE, Crosby SW, et al. Health sector spending and spending on HIV/AIDS, tuberculosis, and malaria, and development assistance for health: progress toward Sustainable Development Goal 3. Lancet. (2020) 396:693–724. doi: 10.1016/S0140-6736(20)30608-5
Keywords: tuberculosis, sociodemographic index, disability-adjusted life years, global burden of disease (GBD), incidence rate
Citation: Xue Y, Zhou J, Wang P, Lan J-h, Lian W-q, Fan Y-Y, Xu B-N, Yin J-P, Feng Z-h, Zhou J and Jia C-Y (2022) Burden of tuberculosis and its association with socio-economic development status in 204 countries and territories, 1990–2019. Front. Med. 9:905245. doi: 10.3389/fmed.2022.905245
Received: 26 April 2022; Accepted: 24 June 2022;
Published: 22 July 2022.
Edited by:
Sree Bhushan Raju, Nizam's Institute of Medical Sciences, IndiaReviewed by:
David Twapokera Mzinza, Malawi University of Science and Technology, MalawiPaulo Hilario Nascimento Saldiva, University of São Paulo, Brazil
Copyright © 2022 Xue, Zhou, Wang, Lan, Lian, Fan, Xu, Yin, Feng, Zhou and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chi-Yu Jia, jiachiyu@qq.com; Jian Zhou, zhoujian1987817@163.com; Zi-hao Feng, feng.zihao@zs-hospital.sh.cn
†These authors have contributed equally to this work
 Yi Xue
Yi Xue Jie Zhou
Jie Zhou Peng Wang
Peng Wang Jun-hong Lan
Jun-hong Lan Wen-qin Lian1
Wen-qin Lian1  Yue-Ying Fan
Yue-Ying Fan Bei-Ni Xu
Bei-Ni Xu Jian Zhou
Jian Zhou Chi-Yu Jia
Chi-Yu Jia