- 1Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, United States
- 2University of Cagliari, Cagliari, Italy
- 3Istituto Superiore di Sanità,Rome, Italy
- 4Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy
- 5Università Vita Salute San Raffaele Milano, Milan, Italy
- 6Department of General Practice, University Hospital Wuerzburg, Wuerzburg, Germany
- 7Universidad de Antioquia, Medellín, Colombia
- 8Dipartimento di Sanità Pubblica e Malattie Infettive, Università La Sapienza, Rome, Italy
- 9Università degli Studi Milano-Bicocca, Milan, Italy
- 10New York State Psychiatric Institute, NewYork, NY, United States
- 11University of Catania, Catania, Italy
- 12Azienda Ospedaliero Universitaria di Cagliari, Cagliari, Italy
- 13Department of Public Health, School of Medicine, Faculty of Medicine, Universidad de Valparaiso, Valparaíso, Chile
Introduction: Italy is one of the high-income countries hit hardest by Covid-19. During the first months of the pandemic, Italian healthcare workers were praised by media and the public for their efforts to face the emergency, although with limited knowledge and resources. However, healthcare workers soon had to face new challenges at a time when the national health system was working hard to recover. This study focuses on this difficult period to assess the impact of the COVID-19 pandemic on the mental health of Italian healthcare workers.
Materials and Methods: Healthcare workers from all Italian regions [n = 5,502] completed an online questionnaire during the reopening phase after the first wave lockdown. We assessed a set of individual-level factors (e.g., stigma and violence against HCWs) and a set of workplace-level factors (e.g., trust in the workplace capacity to handle COVID-19) that were especially relevant in this context. The primary outcomes assessed were score ≥15 on the Patient Health Questionnaire-9 and score ≥4 on the General Health Questionnaire-12, indicators of clinically significant depressive symptoms and psychological distress, respectively. Logistic regression analyses were performed on depressive symptoms and psychological distress for each individual- and workplace-level factor adjusting for gender, age, and profession.
Results: Clinically significant depressive symptoms were observed in 7.5% and psychological distress in 37.9% of HCWs. 30.5% of healthcare workers reported having felt stigmatized or discriminated, while 5.7% reported having experienced violence. Feeling stigmatized or discriminated and experiencing violence due to being a healthcare worker were strongly associated with clinically significant depressive symptoms [OR 2.98, 95%CI 2.36–3.77 and OR 4.72 95%CI 3.41–6.54] and psychological distress [OR 2.30, 95%CI 2.01–2.64 and OR 2.85 95%CI 2.16–3.75]. Numerous workplace-level factors, e.g., trust in the workplace capacity to handle COVID-19 [OR 2.43, 95%CI 1.92–3.07] and close contact with a co-worker who died of COVID-19 [OR 2.05, 95%CI 1.56–2.70] were also associated with clinically significant depressive symptoms. Similar results were found for psychological distress.
Conclusions: Our study emphasizes the need to address discrimination and violence against healthcare professionals and improve healthcare work environments to strengthen the national health system's capacity to manage future emergencies.
Introduction
Italy is one of the high-income countries hit hardest by the Covid-19 pandemic, showing a mortality rate for SARS-CoV-2 among the highest in the world during the first wave in 2020 (1, 2). When the first cases of COVID-19 were confirmed in the country on 31 January 2020, Italy was preparing to face the pandemic with confidence (3). Despite the growing alarm for the decreases in the expenses allocated to the national healthcare system and the protests by citizens and service users' organizations against these cuts over the past years (4–6), official voices stated with pride that the Italian healthcare system was “one of the best in the world based on authoritative rankings,” and it would have been well prepared to give a right answer to the threat (5, 7).
The pandemic has revealed the excessive optimism of these statements and has produced a shocking awareness in healthcare workers (HCWs) of the fragility and vulnerability of the Italian healthcare system (8). During the first months of the pandemic, a substantial number of health professionals found themselves without basic personal protective equipment, with scarce opportunities to get tested for the virus, and with the additional challenges of working in a system with considerable organizational deficiencies that soon went into crisis (9–13). In 2020, according to the Italian National Institute for Insurance against Accidents at Work, around 70% of over 100,000 work accidents claims due to COVID-19 were from HCWs, and 60% of the fatal cases concerned nurses (14). This situation heavily affected the mental wellbeing of Italian HCWs, as shown in previous studies. Using data collected during the first months of the pandemic, Lasalvia et al. (11) reported that 53.8% [95% CI (51.0–56.6%)] of the HCWs in their study showed symptoms of post-traumatic distress, 50.1% (95% CI [47.9–52.3%]) symptoms of clinically relevant anxiety and 26.6% [95% (CI 24.7–28.5%)] of at least moderate depression. Similarly, Rossi et al. (15) conducted a study among HCWs during the first wave of the pandemic and found that 49.4% of the respondents showed symptoms of post-traumatic stress disorder, 24.7% symptoms of depression, and 19.8% symptoms of anxiety.
On 18 May 2020, the national lockdown, which heavily restricted the movement of the population except for necessity, work, and health circumstances for 69 days, was lifted. Although this was seen with joy by the general population, it raised concerns among HCWs, who were worried that reopening prematurely after the first wave could be a recipe for disaster. There were also concerns that the National Health System would not be able to cope with a new wave at a time when staff was working hard to recover. Moreover, while during the first months of the pandemic HCWs were praised by the media and the public and even applauded from balconies as “heroes,” this quickly changed after the reopening. Anger began to ferment in the community against the inefficiencies of the national healthcare system and HCWs, although victims themselves of these inefficiencies, began to be mistakenly seen as the culprits of the failures in addressing COVID-19. In a few weeks, they went from heroes to negligent professionals in the eyes of many persons, while a number of lawyers and prosecutors started to put their decisions and treatment choices under judiciary scrutiny (16). Although studies from other countries have shown the negative impact of stigma and violence related to COVID-19 on HCWs' mental wellbeing (17, 18), these factors have been neglected in previous research conducted in Italy. In the present paper, we used a large national sample of Italian HCWs to examine whether their mental wellbeing during the challenging reopening phase after lockdown was related to 1) individual-level factors such as stigma and violence against HCWs, and 2) workplace-level factors related to COVID-19.
Materials and Methods
Study Design
This cross-sectional study is part of a prospective international project entitled “The COVID-19 HEalth caRe wOrkErS (HEROES) study” (NCT04352634) (19), which includes participants from 25 countries across 4 continents and was jointly launched by Columbia University Mailman School of Public Health and Universidad de Chile School of Public Health (Faculty of Medicine), in collaboration with the Pan American Health Organization (PAHO) and with support from the World Health Organization (WHO). In Italy, the study was supported by the National Institute of Health.
Data were collected in all Italian regions during the reopening phase after the first wave lockdown, from May 2020 to July 2020 (follow-up assessments will be carried out at 18 and 24 months). Participants were clinical and non-clinical HCWs employed in in-patient or out-patient health facilities throughout the country. They were recruited through an invitation sent via email. A list of emails was previously obtained from: (1) HCWs national and/or local orders and organizations (the involvement of orders and organizations allowed to recruit health professionals working at the community level, such as general practitioners and HCWs employed in retirement homes and other facilities outside of the hospital system but heavily affected by COVID-19), (2) HCWs national and/or local unions (the involvement of unions allowed to recruit HCWs usually not organized in orders and organizations, such as cleaning staff, maintenance staff, and others), (3) selected health centers and hospitals. Particular attention was given to involve orders, organizations, unions, health centers, and hospitals and recruit participants from Italian areas differently affected by the COVID-19 pandemic in the North, Center, and South of the country. Further details on the sampling procedures can be found in the study protocol (19).
Measures
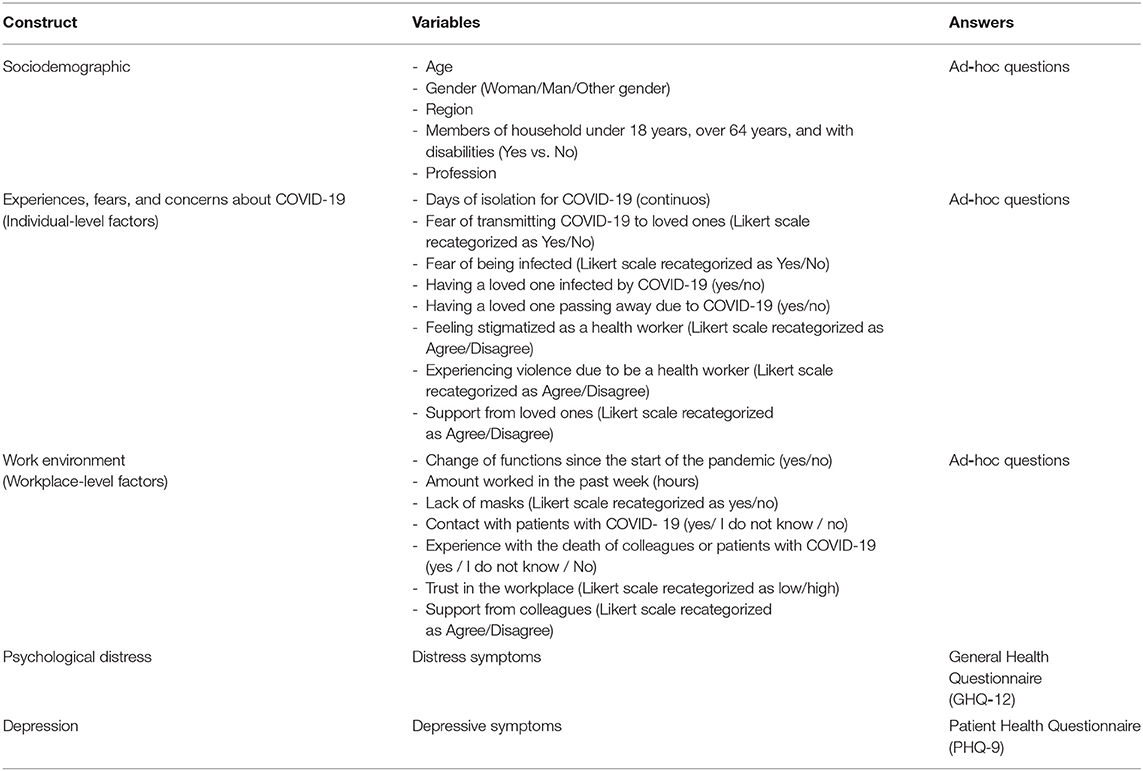
An on-line self-administered questionnaire including standardized measures and some items created ad hoc was used for data collection. The questionnaire included the following sociodemographic variables: gender, age, region, and members of household under 18 years, over 65 years, and with disabilities.
To assess mental wellbeing, we evaluated depressive symptoms and psychological distress. Depressive symptoms were measured by the Italian version of the 9-items Patient Health Questionnaire (PHQ-9) (20, 21). Total PHQ-9 scores range from 0 to 27. According to these scores, depression severity is categorized as “none or minimum” (0-4), “mild” (5-9), “moderate” (10-14), “moderately severe” (15-19), and “severe” (20-27). In this study, PHQ-9 scores ≥ 15 were categorized as indicative of clinically significant depressive symptoms (CSD), which suggest a high probability of major depression for which treatment is recommended (21). Psychological distress was measured by the Italian version of the General Health Questionnaire 12-Items (GHQ-12) (22, 23). Total GHQ-12 scores were calculated using the bimodal scoring method [0-0-1-1]. According to this method, GHQ-12 scores ≥ 4 were categorized as indicative of clinically significant psychological distress (GHQ+) (24). Cronbach's alphas were 0.87 for the PHQ-9 and 0.88 for the GHQ-12.
Individual-level covariates were measured as follows: Feeling stigmatized or discriminated against for the role as HCWs due to the pandemic (Agree, Disagree), Having experienced violence due to being a HCWs during the pandemic (Agree, Disagree), Fear of getting COVID-19 (Yes, No), Fear of infecting the loved ones (Yes, No), Having a loved one infected with COVID-19 (Yes, No), Having loved ones who provided support when needed (Yes, No). Workplace-level covariates were measured as follows: Days in isolation due to COVID-19 (0, 1-19, ≥ 20), hours worked per day on average (≥ 10, ≤ 9), Assignment to a new team or functions (Yes, No), Lack of masks at work (Yes, No), Close contact with patients who were suspected or confirmed cases of COVID-19 (Yes, No, I don't know), Close contact at work with someone who passed away due to COVID-19 (Yes, No, I don't know), Having cared for patients with COVID-19 that passed away (Yes, No, I don't know), Trust in the workplace capacity to manage COVID-19 (low, high), Having a reliable network of supportive colleagues at work (Agree, Disagree). Further details on variables included in the study can be found in Table 1 and the study protocol (19).
Analyses
First, respondents who did provide informed consent but did not continue the survey or did not work in a facility providing healthcare were excluded. Then, respondents who did not complete the survey questions on depressive symptoms and psychological distress were removed. Sensitivity analyses were performed to evaluate potential differences between completers and non-completers. Tabular analyses were used to examine clinically significant depressive symptoms and psychological distress by assessing frequencies for the whole sample and stratified by gender, age, and profession. To examine the association between the individual and workplace-level variables of interest shown in Table 1 (selected a priori from the literature or based on clinical and empirical grounds) on HCWs mental wellbeing, we conducted logistic regression models on depressive symptoms and psychological distress for each variable while controlling for gender, age, and profession. Results were presented as odds ratios (ORs) with 95% confidence intervals. All analyses were performed using SAS (version 9.4 for Windows).
Results
Characteristics of the Respondents
Overall, 5,502 healthcare workers were recruited at baseline. Eighty-nine respondents were excluded because they did provide informed consent but did not continue the survey or did not work in a facility providing healthcare (information on non-responders non-available). Then 1,093 respondents who did not complete the survey questions on depressive symptoms and psychological distress were removed (n = 1,093). In total, 4,320 healthcare workers (78.5%) completed the survey questions on depressive symptoms and psychological distress. There were no relevant differences between completers and non-completers regarding gender (completers: woman 70.8%, man 29.1, non-completers: woman 67.0, man 26.4) and median age (completers: 45, non-completers: 44). Questions on depressive symptoms and psychological distress were in the last section of the questionnaire, suggesting that missingness was mainly at random and due to the length of the questionnaire.
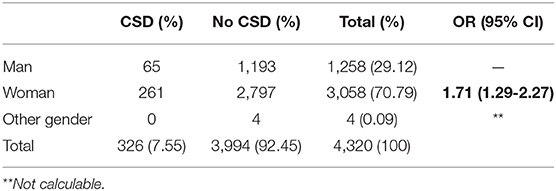
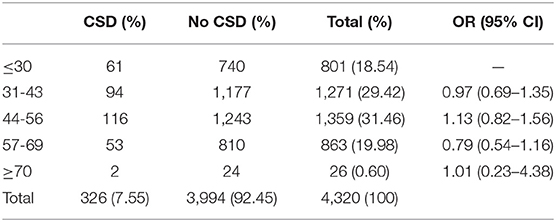
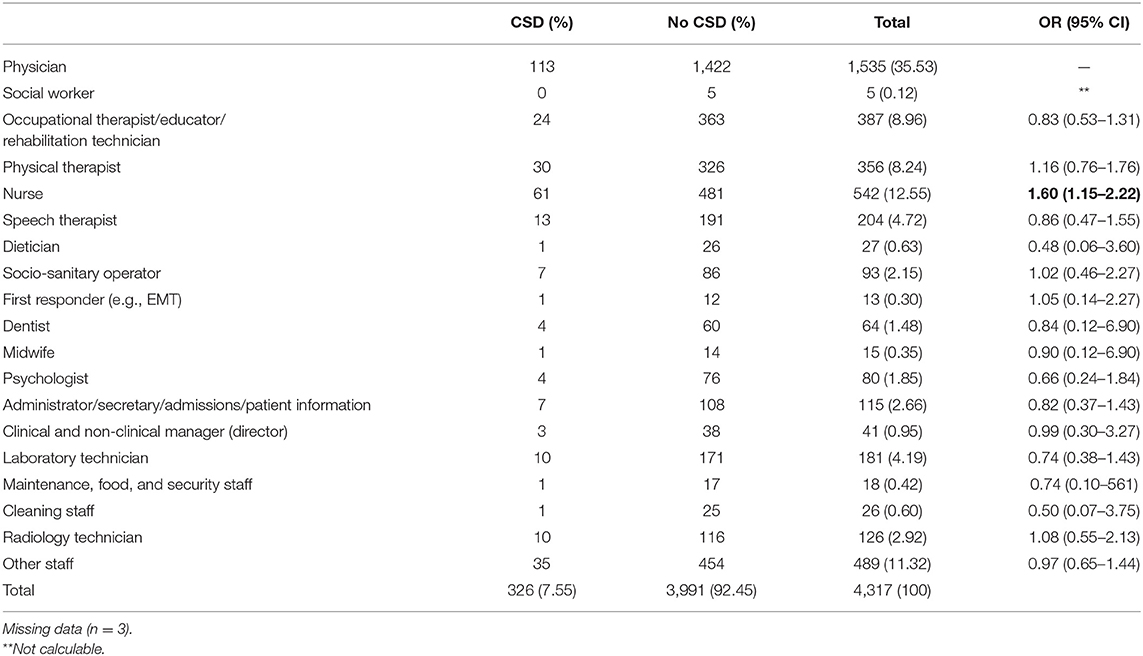
Tables 2–4 show respondents' characteristics, with clinically significant depressive symptoms (CSD) stratified by gender (Table 2), age (Table 3), and profession (Table 4). Overall, 70.79% of participants identified as women, 29.12% as men, and 0.09% as other gender. The median age was 45. Most respondents were physicians (35.53%), nurses (12.55%), occupational therapists, educators, and rehabilitation technicians (8.96%), physical therapists (8.24%), speech therapists (4.72%), laboratory technicians (4.19%), and other staff, including pharmacists, healthcare assistants, dental hygienists, public health workers, and surveillance personnel (11.32%). Clinically significant depressive symptoms were reported by 326 participants, 7.55% of the overall sample. Women were more likely than men to report CSD [OR = 1.71 95% CI (1.29-2.27)]. When comparing the different professions, only nurses reported higher CSD than physicians [OR = 1.60: 95%CI (1.15–2.22)]. Regarding psychological distress, 1,637 respondents (37.89% of the overall sample) screened positive at the GHQ-12, with women reporting higher psychological distress than men [OR = 1.56: 95% CI (1.36–1.89)]. Supplementary Materials 1–3 show respondents' characteristics, with clinically significant psychological distress stratified by gender (Supplementary Material 1), age (Supplementary Material 2), and profession (Supplementary Material 3). In addition, 30.51% of the participants reported having felt stigmatized or discriminated for their role as HCWs and 5.72% reported having experienced violence due to being a healthcare worker during the pandemic.
Association Between Healthcare Workers Individual- and Workplace-Level Factors and Clinically Significant Depressive Symptoms
Table 5 summarizes the results from regression analyses on depressive symptoms for individual-level factors. Feeling stigmatized or discriminated and experiencing violence due to being a HCW during the pandemic increased the likelihood of reporting CSD [OR = 2.98: 95% CI (2.36–3.77)] and [OR = 4.72: 95% CI (3.41–6.54), respectively]. Participants were more likely to report clinically significant depressive symptoms if they lived with persons older than 64 years [OR = 1.50: 95% CI (1.08–2.09)] or with disabilities [OR = 3.08: 95% CI (2.09–4.54)], or if they had a loved one infected with COVID-19 (OR = 1.78: 95% [CI 1.13–2.82]). On the contrary, having loved ones able to provide support when needed was a protective factor [OR = 0.26: 95% CI (0.20–0.35)].
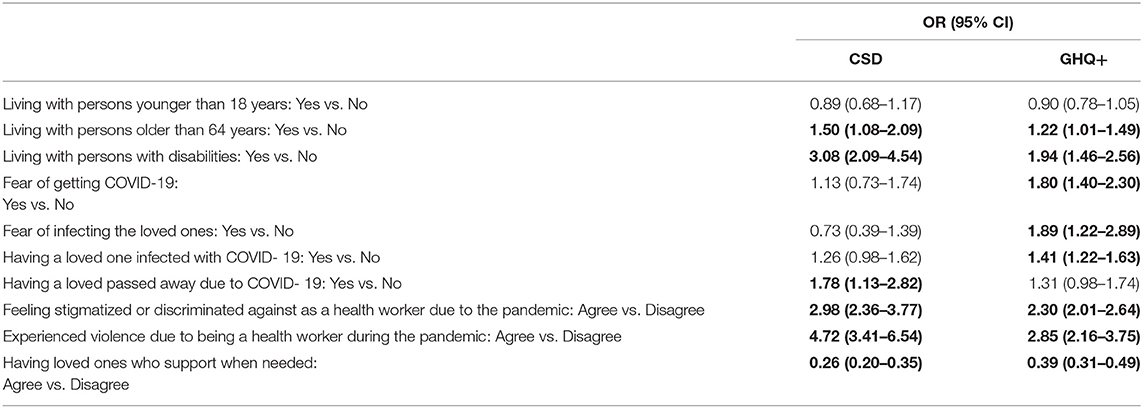
Table 5. Association between health workers individual-level factors and CSD (PHQ-9 ≥ 15) or GHQ+ (GHQ-12 ≥ 4).
Table 6 summarizes the results from regression analyses for workplace-level factors. Participants were more likely to show clinically significant depressive symptoms if they had spent up to 19 days [OR = 1.42: 95% CI (1.03–1.96)] or 20 or more days [OR = 1.52 95%CI (1.01–2.32)] in isolation due to COVID-19, or if they were assigned to a new team or functions [OR = 1.38: 95%CI (1.06–1.79)]. Furthermore, they were more likely to report clinically significant depressive symptoms if they were being close to patients who were suspected or confirmed cases of COVID-19 [OR = 1.39: 95% CI ([1.03–1.87)], if they had close contact at work with someone who later passed away due to COVID-19 [OR = 2.05: 95% CI (1.56–2.70)], or if they cared for patients with COVID-19 that then passed away [OR = 1.79: 95% CI (1.34–2.39).] In answering these three questions, even when respondents were not certain about the COVID-19 status of the patients or persons at work (in that period, it was not always possible to get COVID-19 tests in Italy, and many participants chose the option “I don't know”), they showed an increased risk of CSD. Having low levels of trust in the workplace capacity to manage COVID-19 increased the likelihood of reporting CSD [OR = 2.43: 95% CI (1.92–3.07)]. On the contrary, having a reliable network of supportive colleagues at work was a protective factor [OR = 0.31: 95% CI (0.24–0.39)].
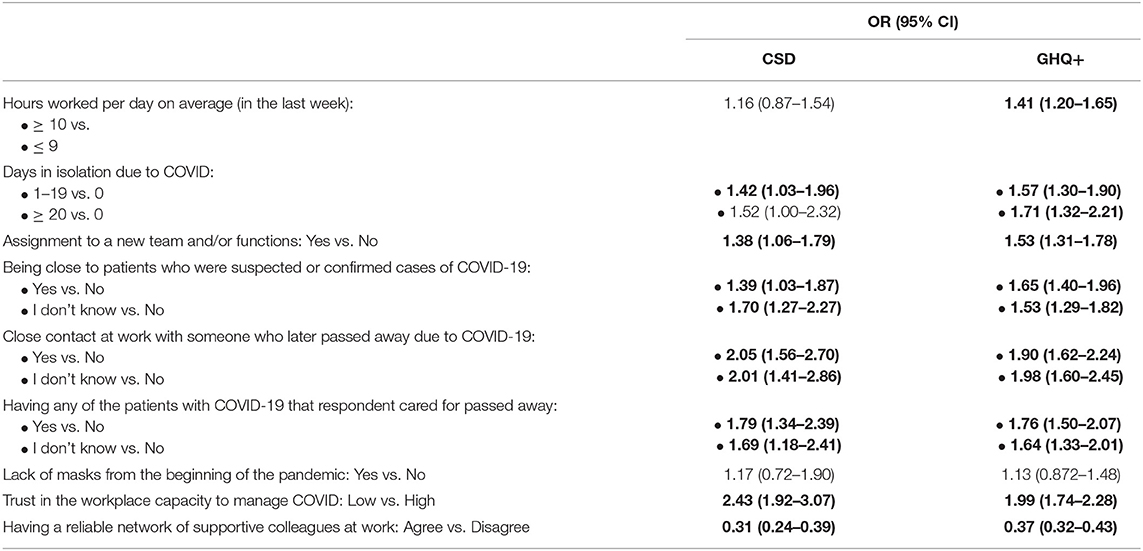
Table 6. Association between health workers workplace-level factors and CSD (PHQ-9 ≥ 15) or GHQ + (GHQ-12 ≥ 4).
Association Between Healthcare Workers Individual- and Workplace-Level Factors and Psychological Distress
Table 5 summarizes the results from regression analyses on psychological distress for individual-level factors. Feeling stigmatized or discriminated against and experiencing violence due to being a HCWs during the pandemic increased the likelihood of reporting GHQ + [OR = 2.30 95% CI (2.01-2.64)] and [OR = 2.85: 95% CI (2.16-3.75)], respectively). Participants were more likely to report clinically significant psychological distress if they lived with persons older than 64 years [OR = 1.22: 95% CI (1.01–1.49)] or with disabilities [OR = 1.94: 95% CI (1.46–2.56)]. Furthermore, they were more likely to show clinically significant psychological distress if they reported fear of getting COVID- 19 [OR =1.80 95%CI (1.40–2.30)] or infecting the loved ones [OR= 1.89: 95% CI (1.22–2.89)], or if they had a loved one infected with COVID-19 [OR= 1.41: 95% CI (1.22–1.63)]. On the contrary, having loved ones who provided support when needed was a protective condition [OR =0.39 95% CI (0.31–0.49)].
Table 6 summarizes the results from regression analyses for workplace-level factors. Participants were more likely to show clinically significant psychological distress if they had spent up to 19 days [OR = 1.57 95% CI (1.30–1.90)] or 20 or more days in isolation due to COVID-19 [OR = 1.71 95% CI (1.32–2.21)], or if they were assigned to a new team or functions [OR = 1.53 95% CI (1.31–1.78)]. Furthermore, they were more likely to show clinically significant psychological distress if they were being close to patients who were suspected or confirmed cases of COVID-19 [OR = 1.65: 95% CI (1.40–1.96)], if they had close contact at work with someone who later passed away due to COVID-19 [OR = 1.90: 95% CI (1.62–2.240)], or if they cared for patients with COVID-19 that then passed away (OR = 1.76: 95% CI [1.50–2.07]). In answering these three questions, even when respondents were not certain about the COVID-19 status of the patients or persons at work, they showed an increased risk of psychological distress. Having low levels of trust in the workplace capacity to manage COVID-19 increased the likelihood of reporting GHQ + (OR = 1.99: 95% CI [1.74–2.28]). On the contrary, having a reliable network of supportive colleagues at work was a protective factor (OR = 0.37: 95% CI [0.32–0.43]).
Discussion
The present study investigated the impact of the COVID-19 pandemic on the mental health of a large sample of Italian healthcare workers, analyzing the role of individual– and workplace–level factors in the reopening phase after the first, strict lockdown.
Among the individual-level factors examined, feeling stigmatized or discriminated against as a healthcare worker due to COVID-19 and having experienced violence due to being a healthcare worker during the pandemic were associated with both clinically significant depressive symptoms and psychological distress. It must be kept in mind that our study was conducted at the end of a period when HCWs were praised as “heroes”, and it was generally believed that the Italian community had gathered around them with great solidarity, while in other countries HCWs were being strongly discriminated and attacked (25, 26). Among several studies conducted during the COVID-19 first wave in Italy, only one in Lombardy assessed discrimination and violence experienced by HCWs, 25% reported episodes of discrimination against themselves, their colleagues, or their family members and even episodes of physical assault and vandalism. Our study demonstrates that during the reopening period after the first wave, discrimination and violence against HCWs were not isolated to specific “high-risk” areas but widespread throughout the national territory. Furthermore, they were strongly associated with clinically significant depressive symptoms and psychological distress among HCWs.
Numerous other individual-level factors were related to negative mental health outcomes. For instance, living with a person older than 64 years or with a disability was associated with clinically significant depressive symptoms and psychological distress. Older adults and persons with disabilities were found at higher risk of severe forms of COVID-19 (27, 28). The increased risk of infection of HCWs and the consequent risk of infecting their family members, coupled with the difficulty of adopting strategies such as physical distancing or isolation in situations where HCWs were also caregivers or supporters in family life, could explain the increased levels of psychological distress. Furthermore, being a caregiver or a supporter has been found to increase the risk of developing depression due to the constant demands caregivers need to face while providing care (29). This is even more the case during a pandemic when HCWs have to deal with additional demands not only at home but also at work. Fear of getting COVID-19, fear of infecting the loved ones, and having a loved one infected with COVID-19 were associated with clinically significant psychological distress but not depression. On the contrary, having a loved one pass away due to COVID-19 was associated with clinically significant depressive symptoms but not psychological distress. A relationship between the loss of a loved one and depression has been shown in several studies (30, 31). The COVID-19 pandemic has complicated such relationship by disrupting the usual experiences of grief. This situation led to increased levels of depression in people grieving loved ones passed due to COVID-19, including HCWs (32–34). Given that HCWs are also at higher risk of getting the infection and thus transmitting it, in many situations, they may have felt responsible for causing the death of their loved ones or experienced survivors guilt and this, in turn, may have led to depression (35). In contrast with the other variables examined, having loved ones able to support when needed was a powerful protective factor against depression and psychological distress among HCWs.
Almost all the workplace-level aspects we analyzed appear to be associated both with clinically significant depressive symptoms and psychological distress. Low trust in the workplace capacity to manage COVID-19 and having a reliable network of supportive colleagues at work were the factors with the strongest association. This is not a surprise considering that the financial cuts to the national health system left Italian health services with limited resources and personnel (8), and thus in a difficult position to face the pandemic effectively. This could also explain why the assignment to a new team and functions was associated with depressive symptoms in Italy but not, for instance, in a country such as Spain that, although close to Italy in terms of organization of services, did not experience the same lack of resources and personnel (36–38). When health services are understaffed, as in Italy, the changes of teams and functions are more frequent and stressful, and having a network of supportive colleagues at work becomes more critical to protect mental wellbeing (39). Interestingly, in contrast with previous research (40), our study found that working long hours was associated with psychological distress but not with depressive symptoms.
Another point worth mentioning is that our depressive symptoms and psychological distress estimates were lower than those of similar Italian and international studies conducted during the pandemic. We found that 7.55% of HCWs showed symptoms of clinically significant depressive symptoms and 37.89% of clinically significant psychological distress while other surveys carried out in Italy among health professionals reported estimates of depression in the whole sample ranging from 13.2% to 62% (41–44). A survey conducted within the framework of the COVID-19 HEROES initiative in Spain, a country close to Italy in terms of geography, culture, and organization of services, found that 27% of the HCWs interviewed screened positive at the PHQ-9 and 74% at the GHQ-12 (36). The lower estimates in our study can be explained by the fact that we collected data during the re-opening phase after lockdown, when the number of COVID-19 cases and thus the workload of HCWs were decreasing, while in Spain and the other studies cited data were collected during the first wave (36, 41, 42) or at the beginning of the second wave (43, 44). Furthermore, we decided to adopt a very high cut-off both for the PHQ-9 (scores ≥ 15) and the GHQ-12 (scores ≥ 4 using the bimodal scoring method), while for instance, the Spanish group adopted lower cut-offs (PHQ-9 > 9 and GHQ-12 > 2) (36). Even when applying the same cut-offs adopted in Spain, we still found lower, although closer, estimates (22.3% of the HCWs screening positive at the PHQ-9 and 45.74% at the GHQ-12). Scores of 15 or greater on the PHQ-9 have high specificity, though low sensitivity, for major depressive disorder (sensitivity: 0.56, specificity: 0.96, PPV: 51%) (21, 45). Similarly, scores ≥ 4 at the GHQ-12 using the bimodal scoring method indicate the likely presence of clinically significant psychological distress (24). Since we aimed to examine the association between individual and workplace-level factors and HCWs' mental wellbeing, we decided to adopt higher cut-offs to increase specificity and positive predictive value at the expense of sensitivity. Nevertheless, the prevalence of clinically significant psychological distress or depressive symptoms among the HCWs in our study is much higher than the prevalence of anxiety and depression found with less conservative cut-off scores in the general Italian population (46, 47) and in previous studies among Italian HCWs (48) before the pandemic.
Our study presents several strengths: the focus on the “reopening phase” after a strict lockdown, a phase of the pandemic overlooked in previous studies, the analysis of factors such as stigma and discrimination against HCWs previously thought peripheral in the Italian context, the inclusion of health professionals usually neglected in studies regarding the pandemic, such as non-clinical HCWs and HCWs employed outside the hospital system, the inclusion of HCWs from Italian areas differently affected by the pandemic (North, Center, and South), and the large sample size. However, our study is not without limitations. We used a non-probabilistic sampling approach, which may have hindered our findings' validity (49) and carries the risk of selection bias. The study's design was cross- sectional, and thus we cannot exclude reverse causation. In addition, we used self-report instruments and ad-hoc instruments that could introduce a bias in comparison with interview-based measures. However, we could not adopt a different methodology due to the COVID-19 restrictions at the time of data collection.
This study expands the literature on the psychological impact of the COVID-19 pandemic on healthcare workers. It shows that numerous individual and workplace-level factors were associated with clinically significant depressive symptoms and psychological distress among healthcare workers during the reopening phase after a strict lockdown. Our findings provide valuable information for policymakers, health service providers, and mental health professionals on the individual and workplace-level factors to target when developing and implementing interventions and preventive actions for future emergencies crises. In particular, the results of our study emphasize the need to address discrimination and violence against HCWs and improve healthcare work environments by eliminating or reducing risk conditions, enhancing social support by peers, and building trust in the healthcare institutions capacity to manage crisis situations in the future.
Data Availability Statement
The datasets presented in this article are not readily available because of restrictions in the Ethical Committee approval. Data can be obtained by MFM and MGC upon reasonable request. Requests to access the datasets should be directed to mfmoro@gmail.com.
Ethics Statement
The study was approved by the Ethics Committee of the Azienda Mista Ospedaliero-Universitaria of Cagliari, Italy. The research was conducted in compliance with the provisions that protect privacy in Europe (Articles 6 and 9 of EU Regulation No. 679). Informed consent was considered given when the health worker agreed to participate.
Author Contributions
MM, ES, FM, and RA coordinated the international COVID-19 HEROES study. MM and MC coordinated the study in Italy and obtained funding. MM and MC conducted the analysis with input from ES and AR. MM drafted the paper and with input from MC, ES, FM, AR, RA, GC, RP, VD, AP, PK, FR, GL, EP, AP, FC, AU, and VR finalized the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The COVID-19 HEROES study in Italy was funded by the Italian Ministry of Education, Universities and Research (Bando FISR 2020IP_05308) and Fondazione di Sardegna (Bando 2020).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all healthcare workers who participated in the study for their time and collaboration. The authors also acknowledge the following organizations and persons: Italian National Federation of Medical Boards, Provincial Medical Boards of Turin and Sassari, Società italiana di pedagogia medica (SIPEM), Società italiana interdisciplinare delle cure primarie (SIICP), Segretariato italiano Giovani Medici (SIGM), Sindacato Medici Italiani (SMI), Irene Bruschi, Alice Serafini, Pier Riccardo Rossi, Movimento Giotto, Ordine interprovinciale TSRM-PSTRP di Cagliari/Oristano, Federazione nazionale Ordini dei Tecnici sanitari di radiologia medica, delle professioni sanitarie tecniche, della riabilitazione e della prevenzione, and Roberta Famulari for their cooperation in the recruitment.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.867080/full#supplementary-material
References
1. John Hopkins University Coronavirus Resource Center (2021). Available online at: https://coronavirus.jhu.edu/map.html (accessed January 31).
2. Dorrucci M, Minelli G, Boros S, Manno V, Prati S, Battaglini M, et al. Excess mortality in italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Front Public Health. (2021) 9:669209. doi: 10.3389/fpubh.2021.669209
3. Ministero della Sanità della Repubblica Italiana. Piano Sanitario Nazionale in Risposta a Un'eventuale Emergenza Pandemica Da Covid-19 (2019).
4. Global Burden of Disease 2020 Health Financing Collaborator Network. Tracking development assistance for health and for COVID-19: a review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990-2050. Lancet. (2021) 398:1317–43. doi: 10.1016/S0140-6736(21)01258-7
5. OECD & European Observatory on Health Systems Policies. State of Health in the EU-Italy Country Health Profile 2019. (2019). Available online at: https://www.oecd.org/italy/italy-country-healthprofile-2019-cef1e5cb-en.htm (accessed January 31, 2022).
6. Mauro M, Giancotti M. Italian responses to the COVID-19 emergency: overthrowing 30 years of health reforms?. Health Policy. (2021) 125:548–52. doi: 10.1016/j.healthpol.2020.12.015
7. Pagella Politica. La sanità italiana è davvero un'eccellenza mondiale? (2020). Available online at: https://pagellapolitica.it/dichiarazioni/8542/la-sanita-italiana-e-davvero-uneccellenza-mondiale (accessed January 31).
8. Caimmi PP, Capponi A, Leigheb F, Occo FD, Sacco R, Minola M, et al. The hard lessons learned by the COVID-19 epidemic in italy: rethinking the role of the national health care service? J Epidemiol Glob Health. (2021) 11:266–70. doi: 10.2991/jegh.k.210420.001
9. Franzoi IG, Granieri A, Sauta MD, Agnesone M, Gonella M, Cavallo R, et al. Anxiety, post-traumatic stress, and burnout in health professionals during the COVID-19 pandemic: comparing mental health professionals and other healthcare workers. Healthcare. (2021) 9:635. doi: 10.3390/healthcare9060635
10. Kurotschka PK, Serafini A, Demontis M, Serafini A, Mereu A, Moro MF, et al. General practitioners' experiences during the first phase of the covid-19 pandemic in italy: a critical incident technique study. Front Public Health. (2021) 3:623904. doi: 10.3389/fpubh.2021.623904
11. Lasalvia A, Bonetto C, Porru S, Carta A, Tardivo S, Bovo C, et al. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol Psychiatr Sci. (2020) 30:1-28. doi: 10.1017/S2045796020001158
12. De Sio S, La Torre G, Buomprisco G, Lapteva E, Perri R, Corbosiero P, et al. Consequences of COVID19-pandemic lockdown on Italian occupational physicians' psychosocial health. PLoS ONE. (2021) 16:e0243194. doi: 10.1371/journal.pone.0243194
13. Di Mattei VE, Perego G, Milano F, Mazzetti M. The healthcare workers' wellbeing (benessere operatori) project: a picture of the mental health conditions of Italian healthcare workers during the first wave of the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:5267. doi: 10.3390/ijerph18105267
14. De Matteis S. COVID-19: are not all workers 'essential'?. Occup Environ Med. (2021) 78:305–6. doi: 10.1136/oemed-2020-107272
15. Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. (2020) 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
16. d'Aloja E, Finco G, Demontis R, Napoli PE, Fossarello M, Nioi M, et al. COVID-19 and medical liability: Italy denies the shield to its heroes. EClinicalMedicine. (2020) 25:100470. doi: 10.1016/j.eclinm.2020.100470
17. Mediavilla R, Fernández-Jiménez E, Andreo J. Association between perceived discrimination and mental health outcomes among health workers during the initial COVID-19 outbreak. Rev Psiquiatr Salud Ment. (2021) 18:S1888-989. doi: 10.1016/j.rpsm.2021.06.001
18. Tenorio Correia Silva A, Mascayano F, Valeri L. COVID-19 pandemic factors and depressive symptoms among primary care workersin São Paulo, Brazil. Am J Public Health. (2022) 112:786-94. doi: 10.2105/AJPH.2022.306723
19. Mascayano F, van der Ven E, Moro MF, Schilling S, Alarcón S. The impact of the COVID-19 pandemic on the mental health of healthcareworkers: study protocol for the COVID-19 HEalth caRe wOrkErS(HEROES) study. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:10257. doi: 10.1007/s00127-021-02211-9
20. Mazzotti E, Fassone G, Picardi A, Sagoni E, Ramieri L, Lega I, et al. Il Patient health questionnaire (PHQ) per lo screening dei disturbi psichiatrici: uno studio di validazione nei confronti della intervista clinica strutturata per il DSM-IV asse I (SCID-I). Ital J Psychopathol. (2003) 9:235–42.
21. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606-13. doi: 10.1046/j.1525-1497.2001.016009606.x
22. Bellantuono C, Fiorio R, Zanotelli R, Tansella M. Psychiatric screening in general practice in Italy. a validity study of the GHQ (General Health Questionnaire) Soc Psychiatry. (1987) 22:113–7. doi: 10.1007/BF00584015
23. Piccinelli M, Politi P. Struttura fattoriale della versione a 12 domande del general health questionnaire in un campione di giovani maschi adulti. Epidemiol Psichiatr Soc. (1993) 2:173–81. doi: 10.1017/S1121189X00006990
24. Rey JJ, Abad FJ, Barrada JR, Garrido LE, Ponsoda V. The impact of ambiguous response categories on the factor structure of the GHQ-12. Psychol Assess. (2014) 26:1021–30. doi: 10.1037/a0036468
25. Gonzalez-Rodriguez A, Labad J, Seeman MV. Schizophrenia and cancer. Curr Opin Support Palliat Care. (2020) 14:232-8. doi: 10.1097/SPC.0000000000000512
26. Bitencourt MR, Alarcao ACJ, Silva LL, Dutra AC, Caruzzo NM, Roszkowski I, et al. Predictors of violence against health professionals during the COVID-19 pandemic in Brazil: a cross-sectional study. PLoS ONE. (2021) 16:e0253398. doi: 10.1371/journal.pone.0253398
27. Ou M, Zhu J, Ji P, Li H, Zhong Z, Li B, et al. Risk factors of severe cases with COVID-19: a meta-analysis. Epidemiol Infect. (2020) 148:e175. doi: 10.1017/S095026882000179X
28. Sabatello m, Scott D, McDonald L. People with disabilities in COVID-19: fixing our priorities. Am J Bioeth. (2020) 20:187-90. doi: 10.1080/15265161.2020.1779396
29. DeokJu K. Relationships Between Caregiving Stress, Depression, and Self-Esteem in Family Caregivers of Adults with A Disability. Occupational Therapy International (2017).
30. Stroebe W, Abakoumkin G, Stroebe M. Beyond depression: yearning for the loss of a loved one. Omega. (2010) 61:85-101. doi: 10.2190/OM.61.2.a
31. Zisook S, Shear K. Grief and bereavement: what psychiatrists need to know. World Psychiatry. (2009) 8:67 – 74. doi: 10.1002/j.2051-5545.2009.tb00217.x
32. Robles R, Morales-Chainé S, Bosch A, Astudillo-García C. Mental health problems among Covid-19 frontline healthcare workers and the other country-level epidemics: the case of mexico. Int J Environ Res Public Health. (2021) 19:421. doi: 10.3390/ijerph19010421
33. Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low- and middle-income countries. Int J Environ Res Public Health. (2018) 15:2165. doi: 10.3390/ijerph15102165
34. Reitsma L, Boelen PA, de Keijser J, Lenferink LIM. Online treatment of persistent complex bereavement disorder, posttraumatic stress disorder, and depression symptoms in people who lost loved ones during the COVID-19 pandemic: study protocol for a randomized controlled trial and a controlled trial. Eur J Psychotraumatol. (2021) 12:1987687. doi: 10.1080/20008198.2021.1987687
35. Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M, et al. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1–12. doi: 10.1007/s40200-020-00643-9
36. Mediavilla R, Fernandez-Jimenez E, Martinez-Ales G, Moreno-Kustner B, Martinez-Morata I, Jaramillo F, et al. Role of access to personal protective equipment, treatment prioritization decisions, and changes in job functions on health workers' mental health outcomes during the initial outbreak of the COVID-19 pandemic. J Affect Disord. (2021) 295:405–9. doi: 10.1016/j.jad.2021.08.059
37. European Commission. European Semester Thematic Factsheet: Health Systems. European Commission (2019).
38. Puangsri P, Jinanarong V, Wattanapisit A. Impacts on and care of psychiatric patients during the outbreak of COVID-19. Clin Pract Epidemiol Ment Health. (2021) 17:52–60. doi: 10.2174/1745017902117010052
39. Sovold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, et al. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front Public Health. (2021) 9:679397. doi: 10.3389/fpubh.2021.679397
40. Luceno-Moreno L, Talavera-Velasco B, Garcia-Albuerne Y, Martin-Garcia J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:5514. doi: 10.3390/ijerph17155514
41. Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
42. Hummel S, Oetjen N, Du J, Posenato E. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study J Med Internet Res. (2021) 23:e24983. doi: 10.2196/24983
43. Lamiani G, Borghi L, Poli S, Razzini K, Colosio C, Vegni E, et al. Hospital employees' well-being six months after the COVID-19 outbreak: results from a psychological screening program in Italy. Int J Environ Res Public Health. (2021) 18:5649. doi: 10.3390/ijerph18115649
44. Ghio L, Patti S, Piccinini G, Modafferi C, Lusetti E, Mazzella M, et al. Anxiety, depression and risk of post-traumatic stress disorder in health workers: the relationship with burnout during COVID-19 pandemic in Italy. Int J Environ Res Public Health. (2021) 18:9929. doi: 10.3390/ijerph18189929
45. Negeri Z, Levis B, Sun Y. Depression Screening Data (DEPRESSD) PHQ group accuracy of the patient health questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis BMJ. (2021) 375:n2183. doi: 10.1136/bmj.n2183
46. Carrà G BF, Galanter M, Crocamo C. Untreated depression and non-medical use of prescription pain relievers: findings from the national survey on drug use and health 2008-2014. Postgrad Med. (2019) 131:52–9. doi: 10.1080/00325481.2019.1546533
47. Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. (2017) 210:119–24. doi: 10.1192/bjp.bp.116.188078
48. Carta MG, Preti A, Portoghese I, Pisanu E, Moro D. Risk for depression, burnout and low quality of life among personnel of a university hospital in Italy is a consequence of the impact one economic crisis in the welfare system? Clin Pract Epidemiol Ment Health. (2017) 13:156–67. doi: 10.2174/1745017901713010156
Keywords: healthcare workers, COVID-19, mental health, stigma, violence, depression, psychological distress, Italy
Citation: Moro MF, Calamandrei G, Poli R, Di Mattei V, Perra A, Kurotschka PK, Restrepo A, Romano F, La Torre G, Preti E, Mascayano F, Picardi A, Chiarotti F, Rapisarda V, Urban A, Alvarado R, Susser E and Carta MG (2022) The Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Workers in Italy: Analyzing the Role of Individual and Workplace-Level Factors in the Reopening Phase After Lockdown. Front. Psychiatry 13:867080. doi: 10.3389/fpsyt.2022.867080
Received: 31 January 2022; Accepted: 02 May 2022;
Published: 02 June 2022.
Edited by:
Samrat Singh Bhandari, Sikkim Manipal University, IndiaReviewed by:
Basudeb Das, Central Institute of Psychiatry, IndiaPankaj Kumar, All India Institute of Medical Sciences, India
Fahimeh Saeed, University of Social Welfare and Rehabilitation Sciences, Iran
Copyright © 2022 Moro, Calamandrei, Poli, Di Mattei, Perra, Kurotschka, Restrepo, Romano, La Torre, Preti, Mascayano, Picardi, Chiarotti, Rapisarda, Urban, Alvarado, Susser and Carta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Francesca Moro, mfmoro@gmail.com
†These authors have contributed equally to this work and share last authorship
 Maria Francesca Moro
Maria Francesca Moro Gemma Calamandrei
Gemma Calamandrei Ranieri Poli4
Ranieri Poli4 Valentina Di Mattei
Valentina Di Mattei Alessandra Perra
Alessandra Perra Peter Konstantin Kurotschka
Peter Konstantin Kurotschka Alexandra Restrepo
Alexandra Restrepo Ferdinando Romano
Ferdinando Romano Giuseppe La Torre
Giuseppe La Torre Emanuele Preti
Emanuele Preti Franco Mascayano
Franco Mascayano Angelo Picardi
Angelo Picardi Flavia Chiarotti
Flavia Chiarotti Antonio Urban
Antonio Urban Ruben Alvarado
Ruben Alvarado Ezra Susser
Ezra Susser Mauro Giovanni Carta
Mauro Giovanni Carta