Abstract
Background
Pharmaceutical Assistance (PA) is a dynamic and multidisciplinary process that aims to supply health systems, programs or services with quality medicines, enabling access and health care, in an efficient and timely manner. The objective of the study was to evaluate the profile of administrative processes for the treatment of PsA, identify the time elapsed in the flow of processes and its associated factors.
Methods
A cross-sectional study of medication requests for the treatment of PsA was carried out between November 2014 and December 2016. Linear regression was used to verify the factors associated with time to delivery.
Results
A total of 218 cases containing 250 drugs were analyzed. The median time between the medical appointment and the first dispensation was 66 days (interquartile range, 44–90). The State proceedings, which includes requesting the drug until the authorization of treatment, was the stage that most contributed to the total time spent. The factors associated with the longer time to delivery of medications were prescriptions coming from clinics and specialty centers, from dermatologists, non-authorized processes and non-persistent patients in the treatment in 12 months.
Conclusion
The median time to receive medicines for the PsA treatment in Belo Horizonte health region after a medical prescription was higher than 2 months. The time between the solicitation of the medicines and the authorization of the treatment in the SUS (State administrative procedure) was the main component of the total time spent.
Similar content being viewed by others
Background
Pharmaceutical Assistance is a dynamic and multidisciplinary process, which aims to supply health systems, programs, or services with medications of quality, enabling patients to access their required medications and the healthcare services they need. Its purpose is to support the health actions required by the community, which should be developed by means of the efficient and opportune provision of medications to inpatient and outpatient care [1]. It is defined as part of the right to health and has been implemented by a set of social and economic policies along the last years in Brazil [2].
In this sense, we could mention the creation of the National Policy of Medications (1998), of the Generic Medications Policy (1998), of the National Agency of Health Surveillance (1999), of the National Policy of Pharmaceutical Assistance (2004) and, more recently, in 2011, the creation of the National Commission of Incorporation of Health Technologies (NCIHT) as important measures in the building and consolidation of pharmaceutical assistance in Brazil [3]. Besides the creation of NCIHT, the Law 12,401 of 2011 has instituted also the ‘Clinical Protocols and Therapeutic Guidelines’ (CPTG) as a strategy to orientate and regulate the access to medications and health procedures in the ambit of the Specialized Component of Pharmaceutical Assistance (SCPA), responsible for the supply of high-cost medications [4].
In practical terms, the access to medications takes place by means of opening of an administrative process by the patient or his/her responsible, which takes place in the health unit designated by the state manager. This process contains the patient’s cadastral information, medical reports, laboratory and images results, and a standardize form (appraisal for request, evaluation, and authorization of drugs). An independent evaluator with formation in health sciences analyzes this documentation and the process could be accepted, dismissed or returned, according to criteria established by the CPTG. In case of acceptance, the standardize form originates an authorization of outpatient procedures of high cost/complexity, which corresponds to three billings /dispensations of medication by SCPA [5].
In the last years, there was a large focus on the incorporation of new technologies to the National Health System (Sistema Único de Saúde - SUS) [6]. However, despite the large advances in PA implementation, few studies have addressed the management processes involved in the access to such technologies, to the practical implementation of services, and to healthcare. This is particularly important given the cost of these new therapies. The amount spent with anti-TNF agents for the treatment of patients with PsA in the SUS between 2010 and 2015 was approximately US$ 300 million (dollar adjusted by purchasing power parity), corresponding to 90% of the total costs with PsA [7].
The present study was conducted to describe the profile of administrative processes for the treatment of PsA and to identify the time elapsed in the flow of processes in the Minas Gerais State, understood as the time elapsed between the prescription and the first dispensation of the medication and the factors associated to this.
Methods
Type of study
This is a cross-sectional study about the medication requests for treatment of PsA to the Minas Gerais Secretary of State for Health during the period between November 4th, 2014, date of publication of the first CPTG of PsA, and December 31st, 2016, with an ancillary analysis of medication persistence in 12 months.
Administrative processes
All of the administrative processes involving medications request for the treatment of PsA have been selected in the Belo Horizonte health region, which meets a population over five million inhabitants, distributed throughout 39 municipalities. The data collection was developed from the Information System of Management of Pharmaceutical Assistance (ISMPA), where the listing of registered patients and administrative processes digitalized between the years of 2014 and 2016 has been obtained. For processes not digitally available, a consultation to physically filed processes has been done close to the Superintendence of Pharmaceutical Assistance of the Minas Gerais Secretary of State for Health.
The variables that were analyzed at baseline were the information contained in the administrative processes, according to the checklist for the request of medicines for the PsA treatment,Footnote 1 being: i. sociodemographic profile (city, age, and sex), ii. clinical profile of patients [body mass index (BMI)], iii. Process characteristics (procedure of steps necessary to request approval and current situation - accepted, dismissed or under evaluation), iv. requested medications, v. profile of units responsible for the request (health establishment and prescriber). The information about the facility was complemented with data coming from the National Registration of Health Establishment.
Time of administrative procedure
To evaluate the time elapsed between the date of medication prescription by the physician and its first dispensation by the Pharmacy of Belo Horizonte health region, the following dates have been registered: T0 = date of medical prescription; T1 = date of administrative claim (registered at ISMPA); T8 = date of process sending to its original unit, after appraisal from the analyst (registered at ISMPA); T9 = date of the first dispensation (registered in the Information System of Hospital Management [ISHM]).
For the calculation of the total time between the medication prescription by the physician (T0) and the first dispensation of medication (T9), it was executed the subtraction of T9 date from T0 date. For the time between the medical prescription (T0) and the administrative claim / process opening (T1), it was executed the subtraction of T1 date from T0 date. To evaluate the time of administrative procedure in the State, which embraces the period from the administrative procedure opening (T1) up to sending to its original Regional Unit (T8), it was executed the subtraction of T8 date from T1 date. Finally, to calculate the time between the date of process output from the State (T8) and the first dispensation of the medication (T9), it was executed the subtraction of T9 date from T8 date. The processes flow has been built utilizing the Bizagi Modeler software version 3.2.6.094 (Fig. 1).
Statistical analysis
The categorical variables were described by means of the distribution of frequencies and the continuous variables by means of mean and standard deviation at baseline. The time spent in the request of medications was described by median and interquartile interval and, additionally, by mean and standard deviation.
The linear regression model was utilized to identify the independently associated variables with the time spent in the request of medications. A significance level of 20% has been adopted for the simple linear regression and another of 5% for the multiple linear regression. The explanatory variables were subdivided into two different groups; a) the proximal ones (cross-sectional variables): variables contained in the administrative processes (per requested process); and b) the distal ones (longitudinal variables): variable of persistence in the 12 months treatment, identified by means of medication dispensations registered on the ISHM (per requested medication; a patient could request for more than one medication). The therapy discontinuation has been defined as the absence of any medication dispensation after 90 days. The statistical analyzes were developed using the software STATA, version 15.1.
Results
As a total, 218 administrative processes containing requests for 250 medications have been analyzed. Among the biological disease modifying anti-rheumatic drugs (bDMARD), tumor necrosis factor alpha inhibitors (anti-TNF α) were the most requested ones, corresponding to 68% of the requests. Adalimumab was the most requested anti-TNF, followed by etanercept and infliximab. Between the conventional synthetic disease modifying anti-rheumatic drugs (csDMARD) (28.4%), the medications methotrexate and leflunomide were the most requested ones (Fig. 2).
Quantitative of processes requested and accepted at Belo Horizonte. Legend: csDMARD = conventional synthetic disease-modifying antirheumatic drugs; NSAID = Nonsteroidal anti-inflammatory drug. Proximal variables = cross-sectional variables, collected in the administrative processes. Distal variable = longitudinal variable, collected after 12 months in the information systems
Out of total processes, 89% were accepted and contained all documents and exams necessary for the evaluation. The mean age of patients was 52.3 years (12.4) and 56.9% were female patients (Table 1).
The larger part of requests came from rheumatologists (74.2%). In relation to the health unit originating the request, 43.4% of requests came from private practices and 32.6% from hospitals. The majority of requesting units were private (62.2%) and 63.7% of them were not accredited to public health service. Between the patients who started the treatment, 54.5% remained in the treatment up to 12 months (Table 1).
The median time between the medication prescription by the physician (T0) and its first dispensation (T9) was of 66 days; Interquartile Range [IQR 44–90] (mean of 75.2 days [standard deviation of 47.4]). Between the medication prescription by the physician (T0) and the process opening (T1), the median time was of 6 days, IQR 0–24 (mean of 13 days [SD 24.6]). The median time for the administrative procedure within the ‘Secretary of State for Health’, considered from the process opening (T1) in the regional unit up to process output, with its sending to the original regional unit (T8) was of 33 days; IQR 25–45 (mean of 40.1 days [SD 26.0]). Finally, the median time spent between the end of the administrative procedure (T8) and the first medication dispensation (T9) was of 19 days; IQR 14–27 (mean of 23.8 days [SD 34.6]) (Table 2). There was no difference between the total median time (T9 – T0) for the anti-TNF and csDMARD medication processes.
The factors associated to the time spent in the request of medications were: original unit, process status, medical specialty, and persistence in the treatment up to 12 months. Requests coming from clinics and medical specialty centers took 22.35 additional days as compared to requests from private practices. Dismissed processes (returned/dismissed/inactive) took 181.08 additional days as compared to accepted processes. Requests coming from dermatologists took 28.29 additional days as compared to requests from rheumatologists. Finally, requests of patients who did not persist in the treatment up to 12 months took 15.73 additional days as compared to patients who effectively persisted in the treatment (Table 3).
Discussion
In our study, the median time between the medical consultation and the first medication dispensation was of, approximately, 2 months (66 days). Such a time interval could be essential in the treatment of rheumatic diseases, mainly when the patient is without any current treatment or will begin his/her first drug treatment for the disease.
A total of 218 administrative processes have been analyzed, which contained requests for 250 medications. Adalimumab was the more requested anti-TNF, followed by etanercept. This profile of anti-TNF utilization is consistent with the literature, finding Adalimumab the most commonly utilized medication to treat PsA and other rheumatic diseases in Brazil [8,9,10].
The higher frequency of requests comes from rheumatologist physicians, and it is in concert with the CPTG of PsA. Such CPTG recommends that individuals with PsA are attended by a team in a specialized service, which counts on a rheumatologist, for his/her adequate diagnosis, treatment inclusion, and follow-up [11]. According to the European League Against Rheumatism (EULAR), rheumatologists are the specialists who should primarily treat the musculoskeletal manifestations of patients with PsA; and in the presence of clinically significant cutaneous involvement, a rheumatologist and a dermatologist should collaborate in the diagnosis and treatment management [12].
However, the literature describes the existence of difficulties in the early forwarding of patients to specialized physicians by the primary care physicians, mainly for patients of countryside small cities, as well as in the maintenance of treatment follow-up and management of patients after forwarding. This difficulty could impact the time up to correct diagnosis of the disease, in association with the time spent on medication supplying by SUS [13].
Clinical recommendations and guidelines mark the diagnosis delay as a great challenge that needs to be approached, as it negatively impacts the treatment result; so, strategies to promote the early forwarding and decrease the delay in diagnoses and inflammatory arthritis treatment have been proposed [14]. This is a problem that has been confronted in Brazil and one of the challenges found is represented by the concentration of rheumatologist physicians in the larger cities and the low availability of rheumatologists at SUS [15].
Despite the large increase in the public formation of rheumatologists by means of medical residences in the last years, the provision of such specialists at SUS is lower than that of private practices and well below than the level recommended in other countries. Internationally, the ideal proportions are pointed out as something between 52,000 and 85,000 inhabitants per rheumatologist. In 2013, Brazil had an approximate ratio of 118,000 inhabitants per rheumatologist, being that, at SUS, such ratio overcomes 400,000 users per rheumatologist. Therefore, SUS has proven to be inefficient to retain a sufficient number of these specialists, who, once finished the medical residence, migrate to private care [15].
Prolonged duration of symptoms in rheumatic diseases is associated with radiographic progression and a lower chance of sustained remission without the use of DMARD [16]. Then, it is observed that as early the treatment in rheumatic diseases as better the clinical results obtained [16, 17]. This is coherent with the observation, in this study, that patients who had larger time between the medication request and its supplying presented lower persistence to treatment in 12 months.
It was identified that the larger part of requests came from private practices, followed by hospitals. Most units requesting medication was private and were not accredited to the SUS. Such data reflect the profile of prescriptions of high-cost medications offered by SUS. It is valid to emphasize that the Belo Horizonte health region is the largest one all over the State, and it is placed in a central and metropolitan area. In this sense, the large number of requests coming from private practices and clinics, specialized units, and hospitals could be expected, and it demonstrates that the follow up of the patients in this setting is appropriate and regular, and allow the prescription of drugs that demand constant vigilance in terms of effectiveness and safety.
A recent study conducted in patients with PsA using biological medications, who were attended at Belo Horizonte health region, has demonstrated that the larger part of patients using such medications possesses, at least, complete high school (77.5%). No illiterate patient has been evaluated (0%) and, about 11% of them had incomplete elementary school. This indicates a possible access difficulty for patients with lower education, who that corroborates the large frequency of prescriptions coming from private units, mainly medical offices, as patients with higher education often use private health services more than the public ones [9]. In this sense, it is observed the existence of gaps and challenges that hamper the access of patient to an adequate follow-up among the different levels of health care [18].
The majority of processes obtained acceptance opinion, which corresponds to processes presenting the entire necessary documentation, with the mandatory exams for their evaluation and acceptance. In this sense, it is emphasized the importance of correct filling and accomplishment of all legal requisites to obtain the respective process acceptance. The proportion of processes acceptance for PsA was larger than that observed for Alzheimer disease and similar to that observed for renal transplantation [19, 20].
The awareness from the physician respecting to the CPTGs accomplishment and the correct filling of all documents approximate the assistant physician and the State, responsible for the medications supplying. An alternative allowing such integration would be the application of the academic detailing tool, which proposes the dissemination and communication to prescribers of the norms and operating conditions of health systems. Besides, it is possible to hear the unmet needs, doubts, and questionings from the physician directly attending the patient, respecting to difficulties found for the medication request [21].
As another challenge, it is observed that populations’ access to medicines is addressed mainly through fragmented, often vertical approaches usually focusing on supply, unrelated to the wider issue of access to health services and interventions [22]. In this case, alternatives to improve the articulation in the health service are needed. One proposal is the approximation of the pharmacist to the patient and physician with the purpose of assist to the pharmacotherapy and improve the information about access to medicines, with impact on quality and efficiency of health services [23].
Proposals of indicators to evaluate the SCPA management capacity have been elaborated to improve results in health [24]. In this sense, measures could be taken to improve the efficiency of medications requesting processes at SCPA. As a proposal, we could indicate in the first process step, between the medical consultation and the process opening (t0 to t1), the suggestion of computerizing the request for medicines with integration to ISMPA from the part of Secretary of State for Health. This way, the physician could forward the requests directly to the Regional Health Unit responsible for the process opening.
In the administrative procedure step (T1 to T8), a similar proposal could be indicated. If the process is digitally and electronically started by the physician, the processes sequence could follow in the same way, without requiring the use of a process on paper. So, this flow could result in higher efficiency for the service, for the physician, and for the patient. A temporary alternative to this proposal would be the computerization of physical processes in the Regional Superintendencies of Health with lower technological capacity, until the implementation of the initial proposal of computerization.
At last, the launch of the applicative “MG App” in 2018, available for Android and iOS, created to facilitate the access to State services can be used to to facilitate the access to information and state services, simplifying the problems resolution and the search for information in mobile phones and other mobile devices. In this applicative is possible: a) to consult medications standardized by the SUS in the state level; b) to follow-up the situation of medication request to SCPA, c) to consult the availability medications in the pharmacy stock; and d) to make scheduling of attendance in the regional pharmacies [25]. So, the time spent in the last step of the process could be reduced and the access to information could be improved for patients.
As a study limitation, it is indicated the occurrence of ignored information in the processes, which could be useful for analysis, besides the supposition that all information available was reliable. Another limitation is that the study was conducted only in the Belo Horizonte health region, responsible for a half of the processes in the State of Minas Gerais. So, the mean time up to dispensation could vary according to the analyzed health region. Despite such limitations, the study has identified relevant aspects that influence the access to medications for the treatment of PsA at SUS, and where interventions could be developed to improve the System efficiency. Besides, the results could be utilized as a comparator for other health regions or to verify the access to treatment of other health conditions in the ambit of SCPA.
Conclusion
The median time to receive medicines for the PsA treatment in Belo Horizonte health region after a medical prescription was higher than 2 months. The time between the solicitation of the medicines and the authorization of the treatment in the SUS (State administrative procedure) was the main component of the total time spent.
Availability of data and materials
The data that support the findings of this study are available from Minas Gerais Secretary of State for Health, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Minas Gerais Secretary of State for Health.
Notes
Available in: http://www.saude.mg.gov.br/formulariosceaf. (last updated version in February of 2019).
Abbreviations
- Anti-TNF:
-
Tumor necrosis factor-alpha inhibitors
- APAC:
-
Authorization of high complexity procedure
- BMI:
-
Body mass index
- CPTG:
-
Clinical protocols and therapeutic guidelines
- DMARD:
-
Disease modifying antirheumatic drugs
- EULAR:
-
European league against rheumatism
- IQR:
-
Interquartile range
- ISHM:
-
Information System of Hospital Management
- ISMPA:
-
Information System of Management of Pharmaceutical Assistance
- LME:
-
Appraisal for request, evaluation, and authorization of drugs (standardize form)
- NCIHT:
-
National Commission of Incorporation of Health Technologies
- PA:
-
Pharmaceutical assistance
- PsA:
-
Psoriatic arthritis
- SCPA:
-
Specialized Component of Pharmaceutical Assistance
- SD:
-
Standard deviation
- SUS:
-
Sistema Único de Saúde
References
Brum LFS. Assistência farmacêutica e acesso a medicamentos. Cad Saúde Pública. 2008;24(6):1457–8. https://doi.org/10.1590/S0102-311X2008000600028.
Costa EA, Araújo PS, Penaforte TR, et al. Conceptions on pharmaceutical services in Brazilian primary health care. Rev Saude Publica. 2017;51(suppl 2):5s. https://doi.org/10.11606/S1518-8787.2017051007107.
Guerra Junior AA, Acurcio FA. Política de Medicamentos e Assistência Farmacêutica. In: Acurcio FA, editor. Medicamentos: Políticas, Assistência Farmacêutica, Farmacoepidemiologia e Farmacoeconomia. Belo Horizonte: COOPMED; 2013. ISBN 978-85-7825-055-3.
Brasil. Presidência da República. Casa Civil. Subchefia para Assuntos Jurídicos. Lei n 12.401 de 28 de abril de 2011. Altera a Lei no 8.080, de 19 de setembro de 1990, para dispor sobre a assistência terapêutica e a incorporação de tecnologia em saúde no âmbito do Sistema Único de Saúde - SUS. Disponível em: http://www.planalto.gov.br/ccivil_03/_ato2011-2014/2011/lei/l12401.htm. Accessed 30 Jul 2018.
Brasil. Ministério da Saúde. Gabinete do Ministro. Portaria n° 2981 de 26 de novembro de 2009. Aprova o Componente Especializado da Assistência Farmacêutica. 2009. Anexo IV. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2009/prt2981_26_11_2009_rep.html. Accessed 30 Jul 2018.
Caetano R, Silva RMD, Pedro ÉM, et al. Incorporation of new medicines by the National Commission for incorporation of technologies, 2012 to June 2016. Cien Saude Colet. 2017;22(8):2513–25. https://doi.org/10.1590/1413-81232017228.02002017.
da Silva MRR, Dos Santos JBR, Almeida AM, et al. Biological therapy in the treatment of psoriatic arthritis: economic and epidemiological considerations. Expert Rev Clin Immunol. 2019 Jun;21:1–9. https://doi.org/10.1080/1744666X.2019.1631798.
Acurcio FA, Machado MA, Moura CS, et al. Medication Persistence of Disease-Modifying Antirheumatic Drugs and Anti-Tumor Necrosis Factor Agents in a Cohort of Patients With Rheumatoid Arthritis in Brazil. Arthritis Care Res. 2016;68(10):1489–96. https://doi.org/10.1002/acr.22840.
Da Silva MRR, dos Santos JBR, Almeida AM, et al. Effectiveness and safety of anti-TNF in psoriatic arthritis patients in Brazil: a post-incorporation analysis. J Comp Eff Res. 2018;7(10):989–1000. https://doi.org/10.2217/cer-2018-0017.
Dos Santos JB, Almeida AM, Acurcio FA, et al. Comparative effectiveness of adalimumab and etanercept for rheumatoid arthritis in the Brazilian public health system. J Comp Eff Res. 2016 Nov;5(6):539–49. https://doi.org/10.2217/cer-2016-0027.
Brasil. Ministério da Saúde. Secretaria de Atenção a Saúde. Portaria Conjunta n° 6/2017 - Publicada em 19/07/2017. Aprova o Protocolo Clínico e Diretrizes Terapêuticas da Artrite Psoriásica. Disponível em: http://conitec.gov.br/images/Relatorios/2017/Relatório_PCDT_Artrite_Psoriásica_Secretário_n°277.pdf. Accessed 30 Jul 2018.
Gossec L, Smolen JS, Ramiro S, et al. European league against rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016;75(3):499–510. https://doi.org/10.1136/annrheumdis-2015-208337.
Silva CR, Carvalho BG, Cordoni L. Júnior, Nunes EFPA. Difficulties in accessing services that are of medium complexity in small municipalities: a case study. Cien Saude Colet. 2017;22(4):1109–20. https://doi.org/10.1590/1413-81232017224.27002016.
Sørensen J, Hetland ML. All departments of rheumatology in Denmark. Diagnostic delay in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis: results from the Danish nationwide DANBIO registry. Ann Rheum Dis. 2015;74(3):e12. https://doi.org/10.1136/annrheumdis-2013-204867.
Albuquerque, CP; Santos-Neto, LL dos. Development of rheumatology training in Brazil: the option for a medical residency program. Rev. Bras. Reumatol., São Paulo, v. 57, n. 6, p. 507–513, dez. 2017. Doi: https://doi.org/10.1016/j.rbre.2016.04.001
van Nies JA, Krabben A, Schoones JW, et al. What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis. 2014;73(5):861–70. https://doi.org/10.1136/annrheumdis-2012-203130.
Raza K, Filer A. The therapeutic window of opportunity in rheumatoid arthritis: does it ever close? Ann Rheum Dis. 2015;74(5):793–4. https://doi.org/10.1136/annrheumdis-2014-206993.
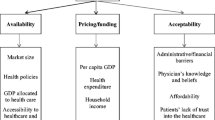
Viegas, APB; carmo, RF; Luz, ZMP. Fatores que influenciam o acesso aos serviços de saúde na visão de profissionais e usuários de uma unidade básica de referência. Saude soc., São Paulo, v. 24, n. 1, p. 100–112, 2015. Doi: https://doi.org/10.1590/S0104-12902015000100008.
Almeida DES, Ceccato MGB, Guerra Júnior AA, Acurcio FA. Avaliação normativa do processo de prescrição e dispensação de imunossupressores para pacientes transplantados renais no estado de Minas Gerais, Brasil, 2008. Epidemiologia e Serviços de Saúde. 2013;22(4):651–60. https://doi.org/10.5123/S1679-49742013000400011.
Almeida-Brasil CC, Costa Jde O, Aguiar VC, et al. Access to medicines for Alzheimer's disease provided by the Brazilian unified National Health System in Minas Gerais state, Brazil. Cad Saude Publica. 2016;32(7):e00060615. https://doi.org/10.1590/0102-311X00060615.
Costa JD, Almeida-Brasil CC, Godman B, et al. Implementation of clinical guidelines in Brazil: should academic detailing be used? J Pharm Health Serv Res. 2016;7:105–15. https://doi.org/10.1111/jphs.12133.
Bigdeli M, Jacobs B, Tomson G, et al. Access to medicines from a health system perspective. Health Policy Plan. 2013 Oct;28(7):692–704. https://doi.org/10.1093/heapol/czs108.
Morrow NC. Pharmaceutical policy part 1 the challenge to pharmacists to engage in policy development. J Pharm Policy Pract. 2015;8(1):4. https://doi.org/10.1186/s40545-015-0027-5.
Rover MRM, Peláez CMV, Faraco EB, Farias MR, Leite SN. An evaluation of governance capacity of the specialized component of pharmaceutical services in Brazil. Cien Saude Colet. 2017;22(8):2487–99. https://doi.org/10.1590/1413-81232017228.01602017.
Governo do Estado de Minas Gerais. Secretaria de Estado de Saúde. Subsecretaria de Políticas e Ações de Saúde. Superintendência de Assistência Farmacêutica. Diretoria de Medicamentos de Alto Custo. Guia Prático de Execução do Componente Especializado da Assistência Farmacêutica (Ceaf). 2018, Versão 1.2, pag 66.
Acknowledgements
The authors are grateful for the institutional support of the Minas Gerais Secretary of State for Health, and the Health Ministry by means of Institutional Program of Development of the SUS (PROADI-SUS).
Funding
This work was supported by National Council for Scientific and Technological Development (CNPq), Brazil (grant number 471819/2013–1) and FAPEMIG, the Minas Gerais State Research Foundation, Brazil (grant number PPM-0015-15 and 03799–16).
Author information
Authors and Affiliations
Contributions
MRRS collected data, analyzed the data and wrote the manuscript; dos JBRS collected data, analyzed the data, contributed with the discussion, and critical reviewed the manuscript; AMA, JAT and FAA designed the study, contributed with the discussion and critical reviewed the manuscript; AMK contributed with the discussion and critical reviewed the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is an integrated part of a project that was approved by the Institutional Review Board/Independent Ethics Committee of Federal University of Minas Gerais, appraisal codes ETIC 0069.0.203.000-1 and CAAE 44121315.2.0000.5149.
Consent for publication
Not applicable.
Competing interests
Adriana Maria Kakehasi has received personal or institutional support from Abbvie, Janssen, Pfizer, Roche and UCB; has delivered speeches at scientific events sponsored by Janssen, Eli Lilly, Pfizer and UCB. Financial competing interest: none. Michael Ruberson Ribeiro da Silva has worked and Jéssica Barreto Ribeiro dos Santos works in Minas Gerais Secretary of State for Health. The other authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
da Silva, M.R.R., dos Santos, J.B.R., Almeida, A.M. et al. Access to high-cost medications for psoriatic arthritis in the National Health System in Brazil: the long path up to dispensation. Adv Rheumatol 59, 48 (2019). https://doi.org/10.1186/s42358-019-0091-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-019-0091-7