Abstract
Post-mortem imaging has a high acceptance rate amongst parents and healthcare professionals as a non-invasive method for investigating perinatal deaths. Previously viewed as a ‘niche’ subspecialty, it is becoming increasingly requested, with general radiologists now more frequently asked to oversee and advise on appropriate imaging protocols. Much of the current literature to date has focussed on diagnostic accuracy and clinical experiences of individual centres and their imaging techniques (e.g. post-mortem CT, MRI, ultrasound and micro-CT), and pragmatic, evidence-based guidance for how to approach such referrals in real-world practice is lacking. In this review, we summarise the latest research and provide an approach and flowchart to aid decision-making for perinatal post-mortem imaging. We highlight key aspects of the maternal and antenatal history that radiologists should consider when protocolling studies (e.g. antenatal imaging findings and history), and emphasise important factors that could impact the diagnostic quality of post-mortem imaging examinations (e.g. post-mortem weight and time interval). Considerations regarding when ancillary post-mortem image-guided biopsy tests are beneficial are also addressed, and we provide key references for imaging protocols for a variety of cross-sectional imaging modalities.
Similar content being viewed by others
Key points
-
Alternatives to a standard ‘invasive’ autopsy may include less invasive alternatives such as using only post-mortem imaging (termed a ‘non-invasive autopsy’) or the addition of image-guided organ biopsies (known as a ‘minimally invasive autopsy’).
-
Early gestational losses (< 20-week gestation) require specialist high-resolution imaging (e.g. micro-CT or high-field MRI) due to small foetal size.
-
Post-mortem ultrasound and MRI are useful for imaging larger foetuses (> 20-week gestation), but unenhanced CT is usually unhelpful in this clinical context, due to limited intrinsic soft tissue detail.
Background
Following the loss of a baby, autopsy is the single most useful investigation after death, yielding additional information or diagnosis in 40–70% of cases [1, 2], of which up to 50% may not have been clinically suspected [3,4,5]. Whilst > 90% of parents are offered an autopsy, the majority refuse this investigation, leading to low autopsy uptake rates (30–40%) [6]. Reasons for refusal include dislike of the invasive procedure, wanting to ‘protect’ the child from further harm as well as religious and cultural beliefs (Table 1) [7]. As a result, many parents do not obtain important information regarding reasons behind their pregnancy loss (and potential future pregnancy losses), and some have reported regretting their decision not to proceed with an autopsy, feeling that many questions remain unanswered [8]. There are also other benefits for performing a perinatal autopsy for the medical community and society at large, including epidemiological information, improved understanding of perinatal pathologies and quality control management (Fig. 1).
In many institutions, at the time of perinatal loss, parents are usually only provided with the binary option of a standard (invasive) autopsy or no further post-mortem investigation. This ‘all-or-nothing’ approach is now slowly being supplemented in some specialist centres with the choice of a ‘less invasive autopsy’ (LIA) which involves performing post-mortem imaging (instead of dissection of the body) and proceeding with minimally invasive tissue sampling (via image-guided organ biopsies) where necessary. Nevertheless, when and how to perform the most appropriate imaging for different clinical scenarios can be difficult for radiologists who infrequently encounter these situations, especially given the lack of published guidelines for reference.
This review aims to help the general and specialist paediatric radiologist understand the advantages and disadvantages of different perinatal post-mortem imaging options to allow for a more open and informed discussion with referring clinicians and bereaved parents. It is structured in a format that addresses commonly encountered queries surrounding the promise and reality of post-mortem imaging, and we provide a pragmatic, evidence-based protocol to address the majority of clinical scenarios that are likely to arise.
Less Invasive Autopsy (LIA): What is it and how is it different to a standard autopsy?
Many parents perceive a standard ‘invasive’ autopsy to only involve the dissection of organs within their child’s body. In fact, standard autopsy consists of many additional non-invasive components, including external inspection of the body, placental examination as well as ancillary investigations such as genetic testing (Fig. 2).
Components of different types of perinatal autopsy. A ‘less invasive autopsy’ (LIA) is an umbrella term for all procedures that use imaging instead of dissection for internal examination at autopsy. Where tissue sampling is also performed in a less invasive way (e.g. image-guided biopsy or laparoscopically assisted biopsy), the study is referred to as a ‘minimally invasive autopsy’ (MIA). Where no incisions are made to the body, and only imaging is acquired, this is termed a ‘non-invasive autopsy’ (NIA) [6]
‘Less invasive autopsy’ (LIA) is an umbrella term generally used to indicate any post-mortem examination where the internal examination (i.e. body dissection) is replaced with cross-sectional post-mortem imaging. The same non-invasive components (as described for the standard autopsy) are often carried out. Where tissue sampling is required (and parental consent provided), image-guided needle biopsies or a laparoscopic approach may be used via small incisions. This allows ancillary tests to be performed (e.g. genetic analysis) as well as histological assessment of targeted organs or lesions. Where image-guided tissue samples are acquired, the investigation is termed a ‘minimally invasive autopsy’ (MIA) [6].
What is the aim of perinatal post-mortem imaging?
The reasons for perinatal losses can be broadly classified into those relating to maternal health issues (e.g. thrombophilia), placental and cord abnormalities, obstetric complications and acquired (infection) or congenital foetal anomalies [9]. Within developed countries, the commonest referral indications for post-mortem imaging relate to assessment of developmental foetal anomalies and perinatal complications (e.g. intracranial haemorrhage). Identification of these pathologies can help understand the reasons for foetal demise or better characterise antenatal imaging findings, particularly where there was a termination of pregnancy.
It is important to bear in mind when counselling parents and clinicians that despite thorough investigations, there remain a significant proportion of perinatal deaths in which the cause for foetal demise remains ‘undetermined’ despite standard autopsy [10, 11]. In addition, some pathologies, such as infection, cannot be radiologically excluded in any cases as typical findings (e.g. pulmonary consolidation) can mimic normal expected post-mortem changes [12]. This should not be used as a reason to refuse performing post-mortem imaging (more to temper any unrealistic expectations), as many parents report feeling a sense of relief and reassurance by an unremarkable result, absolving them of guilt and blame for their loss.
What imaging modalities are best suited for perinatal post-mortem imaging?
Different imaging modalities have different advantages and disadvantages according to the clinical scenario and are also gestational age dependent, largely due to issues related to image resolution. Table 2 provides a summary of factors to take into consideration when deciding which post-mortem imaging modality to conduct, and Fig. 3 provides a visual overview of which studies are most likely to be diagnostic at different gestational ages and sizes.
Typical estimated gestational ages and post-mortem weights where various post-mortem imaging modalities could be used to provide diagnostic quality examinations. ** Technically, radiographs and CT can be performed at any age after 8-week gestation (when the foetal skeleton beings to ossify), but in practice they are best reserved for specific clinical situations, such as for suspected skeletal abnormalities or trauma [57]
In general, for mid-second and third trimester perinatal losses (i.e. > 20-week gestation), whole-body post-mortem ultrasound (PMUS) or MRI (PMMR) is the most appropriate tools. This is in contrast to adult post-mortem imaging where CT is the commonest modality. For perinatal deaths, the lack of internal soft tissue contrast makes CT a less helpful tool [13].
Smaller foetuses, weighing less than 500 g (post-mortem bodyweight) or aged less than 18-week gestation, are more challenging to image with standard imaging technology [14], and specialist techniques are required such as high-field MRI (> 7 T) or ‘microfocus computed tomography’ (i.e. micro-CT)[15]. Local availability will largely determine what can be provided at each specialist centre, sometimes requiring a referral to be made to another centre.
Although the time interval between foetal delivery and post-mortem imaging (i.e. the ‘post-mortem interval’) has not been reported as a major factor in diagnostic post-mortem imaging quality, the degree of maceration does (relating to time between intra-uterine foetal demise and delivery, so-called intra-uterine retention time). This has been reported to be the most significant factor in acquiring a diagnostic quality post-mortem ultrasound study [16, 17] due to the degree of tissue breakdown and laxity of skull sutures. It would therefore be helpful to preferentially acquire an MRI where maceration is known to be extensive (usually when the intra-uterine retention time is estimated > 24 h).
It is therefore important to consider the following when assessing referrals for post-mortem imaging:
-
What is the post-mortem weight of the foetus?
-
What was the time interval between the last reported foetal movements and the delivery of the baby?
-
Were there foetal abnormalities detected during the pregnancy at ultrasound or MRI?
-
Has there been any previous history of perinatal loss, particularly with congenital abnormalities that could be recurrent (e.g. inheritable skeletal dysplasias)?
-
Has the placenta already been examined and provided a clear cause for the perinatal loss (e.g. florid chorioamnionitis)?
-
What imaging modalities are available locally; would this case require a referral to a specialist centre for post-mortem imaging?
A pragmatic, evidence-based protocol is provided in the form of a flowchart in Fig. 4, to help guide referrers and radiologists to which imaging modality would be best suited for different clinical scenarios. It is important to recognise that whilst referrers may state a gestational age for the foetus, this is not usually as helpful as knowing the post-mortem weight in determining the appropriate imaging study.
Recommended post-mortem imaging flowchart for non-invasive investigation of perinatal loss. Small foetuses present a challenge for post-mortem imaging, and care should be taken when interpreting imaging results in this cohort. A foetus weighing over 500 g provides the greatest likelihood for a diagnostic quality 1.5 T MRI study [14], and those weighing < 300 g are best suited for micro-CT or high-field MRI [32]. Where neither MRI nor micro-CT is available, ultrasound may be attempted but there is a higher likelihood of a false or non-diagnostic result [26, 58]. Foetuses weighing between 300 and 500 g have been reported to take > 7 days to iodinate and therefore delay micro-CT imaging. If available, 3 T MRI could be attempted for this foetal cohort [22]
How accurate are the different post-mortem imaging modalities?
An infographic is provided (Fig. 5) summarising the latest published research for each imaging modality, and comparisons between different tools where available. In conducting this review of the research, we searched the PubMed, Embase and Google Scholar databases for search terms including ‘post-mortem’, ‘autopsy’ with ‘imaging’ and ‘perinatal’, ‘foetal’ or ‘neonatal’. The studies included here were chosen as being representative of the literature based on having the largest sample size population for the relevant imaging modality studied, and preference was given to systematic reviews or studies comparing two or more modalities in the same population group to enable comment for differences in diagnostic accuracy. Opinion pieces, non-human studies and case reports were excluded.
MRI
In the largest prospective paediatric post-mortem imaging study to date (the ‘MARIAS’ study [18], including 400 children, of whom 277 (69%) were perinatal losses), there was > 90% concordance for overall diagnosis compared to standard autopsy (sensitivity of 89.7%, specificity of 95%), particularly for abnormalities of the heart, brain and musculoskeletal system. High accuracy rates have been similarly found in subsequent publications using different perinatal populations [19,20,21], and where available, it has been shown that performing post-mortem MRI at 3 T results in higher concordance rates with autopsy than 1.5 T MRI [22] (77% vs. 69%, respectively).
MRI has also been reported to provide clinically useful information where neuropathology was non-diagnostic [23]; however, it has now been suggested that where an (antenatal) foetal brain MRI has been performed, this is more likely to yield useful information for diagnosing complex neurological conditions [24] rather than the post-mortem MRI.
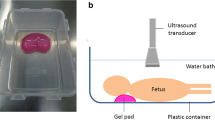
Ultrasound
When the imaging is of diagnostic quality, ultrasound has been reported to have a similar accuracy to both 1.5 T [25] and 3 T MRI [26], with an estimated overall sensitivity of 73% and specificity 97% (based on a systematic review of 455 perinatal losses)[27]. The highest sensitivity rates were found for brain imaging (84%) and lowest for cardiothoracic abnormalities (51%). It is important to note that extensive maceration reduces the diagnostic quality of the imaging, particularly for brain imaging [16, 17]. Where there is maceration or a need to confirm and characterise an underlying cardiac anomaly, post-mortem MRI may be the more appropriate imaging modality.
CT
In a subset of cases from the MARIAS study that underwent both 1.5 T MRI and CT (n = 82) [13], it was found that CT generated a greater number of non-diagnostic studies (22% versus 5%) and the overall accuracy rate was also lower (59% versus 63% where both CT and MRI studies were of diagnostic quality). For these reasons, CT is rarely performed in perinatal post-mortem imaging, but may be more useful in older children, particularly where there is a traumatic or forensic history [28].
Micro-CT
Two of the largest case series published comparing foetal micro-CT with standard autopsy [15, 29], both demonstrated high sensitivity and specificity rates for overall diagnosis (94–100% sensitivity, 90–100% specificity) [15, 29]. The main drawback, however, was the requirement for tissue staining with an iodinated contrast medium which caused some residual discolouration of the foetus and tissue shrinkage [30] and can take several days for full iodination to occur, depending on the size of the foetus. There is also a current lack of availability of this tool within healthcare settings [31].
High-field MRI
This remains a specialist tool only available in some research centres. A recent systematic review [32] only found three publications where whole body post-mortem foetal MRI was performed using a high field (7–11 T). The largest of these studies [33] (n = 17) reported complete agreement between 9.4 T MRI and standard autopsy. Contrast staining of the foetus is not required (unlike for micro-CT); however, scanning times can be lengthy taking hours in some cases.
When would additional tissue sampling be beneficial over imaging alone?
In many cases (60% of intra-uterine deaths), the foetal death is unexplained despite even a standard ‘invasive’ autopsy [10]. Where a cause exists, this is frequently identified through non-invasive means (i.e. 38% intrauterine deaths via placental and clinical assessment) [10]. A recent publication assessing outcomes from > 5000 paediatric autopsies has shown that histological tissue sampling only provides the cause of death in a minority of perinatal cases when no clinical or macroscopic abnormality of the organ is identified, and where placental tissue was available for examination [34] (i.e. low likelihood of histological abnormality where the organ appeared normal at inspection or post-mortem imaging). Furthermore, where antenatal ultrasound and post-mortem MRI results are concordant, the additional value of an autopsy is low (< 5%) [35]. Therefore, the greatest benefit for tissue sampling is clearly where there is a structural anomaly for further investigation, and for obtaining samples for ancillary investigations.
Image guidance is preferred over ‘blind’ percutaneous needle biopsies that use surface landmarks to locate organs, as there is a low tissue targeting success rate (< 52%). Ultrasound-guided biopsies are more successful (76.1%) and can be performed via the umbilical vein mitigating incisions to the body [36]. Laparoscopically guided tissue sampling yields the highest success rates (> 80%) [37] but can be difficult to perform in small foetuses, and necessitates small incisions and more expensive equipment not commonly found in many mortuaries. It is important prior to conducting any tissue sampling that parental consent has been provided for this.
Published protocols for paediatric and perinatal post-mortem imaging techniques
A recommended post-mortem MRI imaging protocol has been devised via an expert consensus survey conducted by the European Society of Paediatric Radiology (ESPR)[38]. An abbreviated protocol can also be followed if MRI scanner time is particularly limited [39]. A more comprehensive article on the different post-mortem MRI sequences is also provided and highly recommended [40].
The ESPR and the International Society for Forensic Radiology and Imaging (ISFRI) have published recommendations for paediatric post-mortem CT imaging [41]; however, these are typically applied to forensic childhood cases rather than perinatal deaths. Where post-mortem ultrasound is performed, two articles in Insights into Imaging describe how to conduct, report and recognise common developmental pathologies [42].
A step-by-step guide for conducting post-mortem micro-CT imaging has been published [31], and currently, high-field MRI still remains predominantly a research tool, with only a few centres describing their methodology [32, 43].
Stakeholder perceptions of the less invasive autopsy
How do healthcare professionals perceive the less invasive autopsy?
Healthcare professionals (e.g. obstetricians, pathologists, midwives) have reportedly found it helpful to be able to provide a greater variety of post-mortem examination options (e.g. imaging) to parents when consenting for autopsies in general [44]. Their main concerns regarding less invasive approaches relate to those of missed diagnoses and the ability for the post-mortem imaging to be provided locally.
How do parents perceive the less invasive autopsy?
In general, acceptance rates are high. In one study, it was reported that 91% of 859 parents surveyed indicated they would consent to a less invasive autopsy over standard autopsy if they had been given the choice [45]. Almost half (46%) preferred imaging with organ tissue sampling, 31% preferred imaging alone and 14% preferred standard autopsy.
Parents valued post-mortem imaging because it allows the baby to ‘rest in peace’ and put parents ‘more at ease’, but also valued approaches where tissue samples were obtained via a small incision, as they were considered a ‘good compromise’ between the least and most invasive approaches.
Religious parental groups have also expressed support for post-mortem imaging examinations as a religiously acceptable replacement over body dissection, as long as the body can be returned swiftly for burial. Minimally invasive options were less acceptable, although preferable to the standard autopsy, and some religious parents would consider this option if there had been multiple pregnancy losses [46, 47] (Table 1).
What is the best way to consent parents for post-mortem imaging?
It is important that consent is conducted in a sensitive and compassionate manner. Some bereaved parents will have clear views regarding their level of acceptance for invasiveness of a standard autopsy; however, a subset will be undecided. ‘Decisional drivers’ [48] include an open approach by a trusted practitioner, adequate time for deliberation and adopting an individualised approach (both in the required depth and amount of information provided). There is rarely a ‘correct’ answer, and each parent will need to feel supported in their personal patient journey [46]. It may be helpful to highlight relevant charity groups for additional emotional support.
On a practical level, permission to perform post-mortem imaging is included as part of the standard autopsy consent form at our institution to minimize additional paperwork [49]. Parental consent is also sought at the same time for the use of post-mortem images in research, teaching, audit and education. This avoids repeated, unnecessary and potentially distressing discussions with parents.
Preparing a department for perinatal post-mortem imaging referral practice
Having a pre-defined plan of what services can be provided and how referrals can be made through multi-disciplinary team discussions are vital. Several articles on the initial experiences of other centres in developing a paediatric post-mortem imaging service have been written, which contain useful information for further reading [50,51,52,53,54,55,56].
Some key points to consider include:
-
Identifying which imaging modalities are available locally for post-mortem imaging and which members of staff (both radiologists and radiographers/sonographers) would be comfortable to be involved in the process (e.g. vetting referrals, protocolling and reporting imaging studies).
-
Clarifying the availability and procedure for external referrals to specialist centres for other post-mortem imaging modalities that are not available locally (e.g. micro-CT or high-field MRI).
-
Determining whether an expedited investigation can be performed, if required (e.g. within 24 h for religious reasons)
-
Availability of funding streams to maintain a post-mortem imaging service, and for the training of radiologists and radiographers in setting up such a service (e.g. attendance at courses, conferences and observership at centres which regularly carry out paediatric post-mortem imaging).
-
There may be additional medicolegal requirements depending on the jurisdiction in which post-mortem imaging is being performed.
Conclusions
Perinatal post-mortem imaging can provide a non-invasive method for death investigation, but can also aid in MIA or provide additional information if a full autopsy is needed. A variety of tools and their advantages and drawbacks are addressed in this article, with a suggested flowchart to help guide radiologists unfamiliar with the best tools to use in different perinatal death settings. Key aspects from the perinatal history include gestational age, antenatal anomalies (in particular cardiac and brain malformations) as well as more pragmatic details regarding availability of different scanners locally. Key challenges for post-mortem imaging still remain regarding local scanner availability, appropriate parental consent and funding streams.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated. Summary of findings from the previously published articles is provided already in figures within this review.
Abbreviations
- CT:
-
Computed tomography
- MIA:
-
Minimally invasive autopsy
- MRI:
-
Magnetic resonance imaging
- PACS:
-
Picture archiving and communications system
- PM Micro-CT:
-
Post-mortem microfocus computed tomography
- PMCT:
-
Post-mortem computed tomography
- PMMR:
-
Post-mortem magnetic resonance imaging
- PMSS:
-
Post-mortem skeletal survey
- PMUS:
-
Post-mortem ultrasound
References
Nese N, Bulbul Y (2018) Diagnostic value of perinatal autopsies: analysis of 486 cases. J Perinat Med 46:175–181
Gordijn SJ, Erwich JJ, Khong TY (2002) Value of the perinatal autopsy: critique. Pediatr Dev Pathol 5:480–488
Widmann R, Caduff R, Giudici L et al (2017) Value of postmortem studies in deceased neonatal and pediatric intensive care unit patients. Virchows Arch 470:217–223
Nayak SS, Shukla A, Lewis L et al (2015) Clinical utility of fetal autopsy and its impact on genetic counseling. Prenat Diagn 35:685–691
Rodriguez MA, Prats P, Rodriguez I, Cusi V, Comas C (2014) Concordance between prenatal ultrasound and autopsy findings in a tertiary center. Prenat Diagn 34:784–789
Shelmerdine SC, Hutchinson JC, Arthurs OJ, Sebire NJ (2020) Latest developments in post-mortem foetal imaging. Prenat Diagn 40:28–37
Lewis C, Hill M, Arthurs OJ, Hutchinson C, Chitty LS, Sebire NJ (2018) Factors affecting uptake of postmortem examination in the prenatal, perinatal and paediatric setting. BJOG 125:172–181
Heazell AE, McLaughlin MJ, Schmidt EB et al (2012) A difficult conversation? The views and experiences of parents and professionals on the consent process for perinatal postmortem after stillbirth. BJOG 119:987–997
Nijkamp JW, Sebire NJ, Bouman K, Korteweg FJ, Erwich J, Gordijn SJ (2017) Perinatal death investigations: What is current practice? Semin Fetal Neonatal Med 22:167–175
Man J, Hutchinson JC, Heazell AE, Ashworth M, Levine S, Sebire NJ (2016) Stillbirth and intrauterine fetal death: factors affecting determination of cause of death at autopsy. Ultrasound Obstet Gynecol 48:566–573
Basu MN, Johnsen IBG, Wehberg S, Sorensen RG, Barington T, Norgard BM (2018) Causes of death among full term stillbirths and early neonatal deaths in the Region of Southern Denmark. J Perinat Med 46:197–202
Arthurs OJ, Barber JL, Taylor AM, Sebire NJ (2015) Normal perinatal and paediatric postmortem magnetic resonance imaging appearances. Pediatr Radiol 45:527–535
Arthurs OJ, Guy A, Thayyil S et al (2016) Comparison of diagnostic performance for perinatal and paediatric post-mortem imaging: CT versus MRI. Eur Radiol 26:2327–2336
Jawad N, Sebire NJ, Wade A, Taylor AM, Chitty LS, Arthurs OJ (2016) Body weight lower limits of fetal postmortem MRI at 1.5 T. Ultrasound Obstet Gynecol 48:92–97
Hutchinson JC, Kang X, Shelmerdine SC et al (2018) Postmortem microfocus computed tomography for early gestation fetuses: a validation study against conventional autopsy. Am J Obstet Gynecol 218:445.e441-445.e412
Shelmerdine SC, Langan D, Mandalia U, Sebire NJ, Arthurs OJ (2020) Maceration determines diagnostic yield of fetal and neonatal whole body post-mortem ultrasound. Prenat Diagn 40:232–243
Kang X, Resta S, Cos Sanchez T, Carlin A, Bevilacqua E, Jani JC (2019) Impact of the delay between fetal death and delivery on the success of postmortem ultrasound following termination of pregnancy. J Matern Fetal Neonatal Med:1–6.
Thayyil S, Sebire NJ, Chitty LS et al (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet (London, England) 382:223–233
Ashwin C, Hutchinson JC, Kang X et al (2017) Learning effect on perinatal post-mortem magnetic resonance imaging reporting: single reporter diagnostic accuracy of 200 cases. Prenat Diagn 37:566–574
Whitby EH, Offiah AC, Cohen MC (2015) Initial experiences of a minimally invasive autopsy service. A report of the techniques and observations in the first 11 cases. Pediatr Dev Pathol 18:24–29
Leadbetter KZ, Vesoulis ZA, White FV et al (2017) The role of post-mortem MRI in the neonatal intensive care unit. J Perinatol 37:98–103
Kang X, Cannie MM, Arthurs OJ, Segers V, Fourneau C, Bevilacqua E, Cos Sanchez T, Sebire NJ, Jani JC (2017) Post-mortem whole-body magnetic resonance imaging of human fetuses: a comparison of 3-T vs. 1.5-T MR imaging with classical autopsy. Eur Radiol 27:3542–3553
Arthurs OJ, Thayyil S, Pauliah SS et al (2015) Diagnostic accuracy and limitations of post-mortem MRI for neurological abnormalities in fetuses and children. Clin Radiol 70:872–880
Goergen SK, Alibrahim E, Govender N et al (2019) Diagnostic assessment of foetal brain malformations with intra-uterine MRI versus perinatal post-mortem MRI. Neuroradiology 61:921–934
Shelmerdine SC, Sebire NJ, Arthurs OJ (2021) Diagnostic accuracy of postmortem ultrasound vs 1.5T postmortem MRI for non-invasive perinatal autopsies. Ultrasound Obstet Gynecol 57(3):449–458
Kang X, Cos Sanchez T, Arthurs OJ et al (2019) Postmortem fetal imaging: a prospective blinded comparison study of 2-dimensional ultrasound with MR imaging. Ultrasound Obstet Gynecol 54(6):791–799
Shelmerdine S, Langan D, Sebire NJ, Arthurs O (2019) Diagnostic accuracy of perinatal post-mortem ultrasound (PMUS): a systematic review. BMJ Paediatr Open 3:e000566
Shelmerdine SC, Davendralingam N, Palm L et al (2019) Diagnostic accuracy of postmortem CT of children: a retrospective single-center study. AJR Am J Roentgenol 1–13
Shelmerdine SC, Simcock IC, Hutchinson JC et al (2020) Postmortem microfocus computed tomography for noninvasive autopsies: experience in >250 human fetuses. Am J Obstet Gynecol 224(1):103.e1–103.e15
Vickerton P, Jarvis J, Jeffery N (2013) Concentration-dependent specimen shrinkage in iodine-enhanced microCT. J Anat 223:185–193
Simcock IC, Shelmerdine SC, Hutchinson JC, Sebire NJ, Arthurs OJ (2021) Human fetal whole-body postmortem microfocus computed tomographic imaging. Nat Protoc.
Dawood Y, Strijkers GJ, Limpens J, Oostra RJ, de Bakker BS (2020) Novel imaging techniques to study postmortem human fetal anatomy: a systematic review on microfocus-CT and ultra-high-field MRI. Eur Radiol 30:2280–2292
Thayyil S, Cleary JO, Sebire NJ et al (2009) Post-mortem examination of human fetuses: a comparison of whole-body high-field MRI at 9.4 T with conventional MRI and invasive autopsy. Lancet (London, England) 374:467–475
Lewis C, Hutchinson JC, Riddington M et al (2019) Minimally invasive autopsy for fetuses and children based on a combination of post-mortem MRI and endoscopic examination: a feasibility study. Health Technol Assessm (Winchester England) 23:1–104
Shelmerdine SC, Arthurs OJ, Gilpin I et al (2019) Is traditional perinatal autopsy needed after detailed fetal ultrasound and post-mortem MRI? Prenat Diagn 39:818–829
Shelmerdine SC, Hutchinson JC, Ward L et al (2020) INTACT (INcision-less TArgeted Core Tissue) biopsy procedure for perinatal autopsy. Ultrasound Obstet Gynecol 55:667–675
Hutchinson C, Shelmerdine SC, Lewis C et al (2019) Feasibility and experience of the MinImAL procedure: minimally invasive perinatal and paediatric autopsies with laparoscopically assisted tissue sampling. Ultrasound Obstet Gynecol 54:661–669
Whitby E, Offiah AC, Shelmerdine SC et al (2021) Current state of perinatal postmortem magnetic resonance imaging: European Society of Paediatric Radiology questionnaire-based survey and recommendations. Pediatr Radiol 51(1):792–799
Shelmerdine SC, Singh M, Norman W, Jones R, Sebire NJ, Arthurs OJ (2019) Automated data extraction and report analysis in computer-aided radiology audit: practice implications from post-mortem paediatric imaging. Clin Radiol 74:733.e711-733.e718
Norman W, Jawad N, Jones R, Taylor AM, Arthurs OJ (2016) Perinatal and paediatric post-mortem magnetic resonance imaging (PMMR): sequences and technique. Br J Radiol 89:20151028
Shelmerdine SC, Gerrard CY, Rao P et al (2019) Joint European Society of Paediatric Radiology (ESPR) and International Society for Forensic Radiology and Imaging (ISFRI) guidelines: paediatric postmortem computed tomography imaging protocol. Pediatr Radiol 49:694–701
Shelmerdine SC, Sebire NJ, Arthurs OJ (2019) Perinatal post-mortem ultrasound (PMUS): radiological–pathological correlation. Insights Imaging 10:81
Thayyil S, Cleary JO, Sebire NJ et al (2009) Post-mortem examination of human fetuses: a comparison of whole-body high-field MRI at 9·4 T with conventional MRI and invasive autopsy. The Lancet 374:467–475
Lewis C, Hill M, Arthurs OJ, Hutchinson JC, Chitty LS, Sebire N (2018) Health professionals’ and coroners’ views on less invasive perinatal and paediatric autopsy: a qualitative study. Arch Dis Child 103:572–578
Lewis C, Riddington M, Hill M, Arthurs OJ et al (2019) Availability of less invasive prenatal, perinatal and paediatric autopsy will improve uptake rates; a mixed methods study with bereaved parents. BJOG 126(6):745–753
Lewis C, Latif Z, Hill M, Riddington M, Lakhanpaul M, Arthurs OJ (2018) “We might get a lot more families who will agree”: Muslim and Jewish perspectives on less invasive perinatal and paediatric autopsy. PLoS ONE 13:e0202023
Ben Taher M, Pearson J, Cohen M, Offiah AC (2018) Acceptability of post-mortem imaging among Muslim and non-Muslim communities. Br J Radiol 91:20180295
Lewis C, Riddington M, Hill M et al (2019) “The communication and support from the health professional is incredibly important”: A qualitative study exploring the processes and practices that support parental decision-making about postmortem examination. Prenat Diagn 39:1242–1253
Judge-Kronis L, Hutchinson JC, Sebire NJ, Arthurs OJ (2016) Consent for paediatric and perinatal postmortem investigations: implications of less invasive autopsy. J Forensic Radiol Imaging 4:7–11
Cohen MC, Whitby E, Fink MA, Collett JM, Offiah AC (2015) Running a postmortem service—a business case and clinical experience. Pediatr Radiol 45:501–508
Alison M (2015) Postmortem imaging in paediatric radiology—the French perspective. Pediatr Radiol 45:482
Arthurs OJ, van Rijn RR, Taylor AM, Sebire NJ (2015) Paediatric and perinatal postmortem imaging: the need for a subspecialty approach. Pediatr Radiol 45:483–490
Ruder TD (2015) What are the greatest challenges or barriers to applying post-mortem imaging in pediatric radiology? Pediatr Radiol 45:479
Hatch GM (2015) What are the greatest challenges or barriers to applying post-mortem imaging in pediatric radiology? Pediatr Radiol 45:480
Chapman S (2015) What are the greatest challenges and/or barriers to applying postmortem imaging in paediatric radiology? Pediatr Radiol 45:478
Cain TM (2015) What are the greatest challenges or barriers to applying postmortem imaging in paediatric radiology? Pediatr Radiol 45:481
Arthurs OJ, Calder AD, Kiho L, Taylor AM, Sebire NJ (2014) Routine perinatal and paediatric post-mortem radiography: detection rates and implications for practice. Pediatr Radiol 44:252–257
Kang X, Shelmerdine SC, Hurtado I et al (2019) Postmortem examination of human fetuses: comparison of two-dimensional ultrasound with invasive autopsy. Ultrasound Obstet Gynecol 53:229–238
Rutty G (2010) Religious attitudes to death and post-mortem examinations. In: Burton JL, Rutty G (eds) The hospital autopsy: a manual of fundamental autopsy practice. CRC Press, London, pp 39–58
Funding
I.C.S. is funded by an National Institute for Health Research (NIHR) Clinical Doctoral Research Fellowship (ICA-CDRF-2017-03-53). C.L. is funded by an NIHR Advanced Fellowship (NIHR-300099). O.J.A is funded by an NIHR Career Development Fellowship (NIHR-CDF-2017-10-037). The authors receive funding from the Great Ormond Street Children’s Charity and the Great Ormond Street Hospital NIHR Biomedical Research Centre. This article presents independent research funded by the NIHR, and the views expressed are those of the author(s) and not necessarily those of the NHS, NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing and editing of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was not required for the writing of this review article. Individual studies referenced in this review have all received ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shelmerdine, S.C., Hutchinson, J.C., Lewis, C. et al. A pragmatic evidence-based approach to post-mortem perinatal imaging. Insights Imaging 12, 101 (2021). https://doi.org/10.1186/s13244-021-01042-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-021-01042-1