Abstract
Background
Current vital statistics of birth population and neonatal outcome in China lacked information and definition of deaths at delivery and during hospitalization, especially for extreme preterm (EPT) birth. This study aims to delineate the prevalence of neonatal hospitalization, neonatal and infant mortality rates (NMR, IMR) and associated perinatal risks based on all livebirths in Huai’an, an evolving sub-provincial region in eastern China.
Methods
This retrospective cohort study established a comprehensive database linking information of whole regional livebirths and neonatal hospitalization in 2015, including deaths at delivery and EPT livebirths. The primary outcomes were NMR and IMR stratified by gestational age (GA) and birthweight (BW) with 95% confidence intervals. Causes of the neonatal and infant deaths were categorized according to the International Statistical Classification of Diseases 10th version, and population attributable fractions of GA and BW strata were analyzed. Perinatal risks of infant mortalities in continuum periods were estimated by Cox regression models.
Results
Among the whole livebirth population (59056), 7960 were hospitalized (prevalence 13.5%), with 168 (2.8‰) in-hospital deaths. The NMR was 3.6 (3.2, 4.1)‰ and IMR 4.9 (1.4, 4.5)‰, with additionally 35 (0.6‰) deaths at delivery. The major causes of infant deaths were perinatal conditions (2.6‰, mainly preterm-related), congenital anomalies (1.5‰), sudden unexpected death in infancy (0.6‰) and other causes (0.2‰). The deaths caused by preterm and low BW (LBW) accounted for 50% and 40% of NMR and IMR, with 20-30% contributed by EPT or extremely LBW, respectively. Multivariable Cox regression analysis revealed that peripartum factors and LBW strata had strong association with early- and late-neonatal deaths, whereas those of GA < 28 weeks were highly associated with postneonatal deaths. Congenital anomalies and neonatal hospitalization remained high death risks over the entire infancy, whereas maternal co-morbidities/complications were modestly associated with neonatal but not postneonatal infant mortality.
Conclusions
The NMR, IMR, major causes of deaths and associated perinatal risks in continuum periods of infancy, denote the status and quality improvement of the regional perinatal-neonatal care associated with socioeconomic development. The study concept, applicability and representativeness may be validated in other evolving regions or countries for genuine comparison and better maternal-infant healthcare.
Similar content being viewed by others
Background
As China has been dramatically progressing in maternal and child healthcare in the past decades with growing economy and social welfare in transition [1,2,3], the under 5 mortality rate (per 1000 livebirths) has declined steadily from 53.7 in 1990 to 8.6 in 2019, with infant mortality rate (IMR) from 42.1 to 6.8, and neonatal mortality rate (NMR) from 29.5 to 3.9 [4], respectively. The foremost achievement is the substantial reduction of maternal and infant death of perinatal causes by early surveillance for high-risk pregnancy, centralized hospital delivery, prevention of preterm birth, and early postnatal care of critically ill infants [1,2,3, 5]. All these are contributed by the improved perinatal-neonatal care infrastructure and universal health insurance policy in effect since 2010 [1, 5].
Currently reported epidemiological data of NMR and IMR in China are derived from either selective hospital birth registries or sampling of nationwide birth surveillance, the Maternal and Child Health Surveillance System (MCHSS) [1,2,3, 6, 7], for making maternal-infant health policies [3, 7]. However, these data sources have limited function in exploring causation of perinatal-neonatal care and outcome due to stratified sampling of data collection, incompleteness and inconsistency of definitions for informative data, and exclusion of births below 28 weeks of gestational age (GA) [1,2,3, 6, 7]. It results in altered source of population and difficulty for comparison of vital statistics especially in very or extremely preterm birth in reference to the relevant international reports [8,9,10]. Besides, the lack of integrated information of maternal/pregnancy factors, birth status and in-hospital care of neonates hinders the exploration of risk factors and their impact, as contributing coefficient and probability through regression models, on adverse outcome associated with major morbidities leading to neonatal and infant deaths [1,2,3, 6, 7]. By now, there are rare epidemiological studies towards perinatal, neonatal and infant outcomes with comprehensive antenatal, peripartum and postnatal information based on a whole regional livebirth population in China. It might also restrain the evaluation of efficiencies of perinatal-neonatal and infant healthcare systems under local socioeconomic status (SES) and medical resource settings.
In 2010 and 2015, we conducted two prospective studies of perinatal-neonatal outcome assessment, based on complete birth population in Huai’an, through unified definitions and inclusion of almost all births under 28 weeks as extreme preterm [11,12,13,14]. With these efforts, we attempted to provide comprehensive vital statistic data on perinatal and neonatal mortality rates, with estimation of perinatal risks and outcome based on whole birth population from a sub-provincial (prefectural) region. The source population constituted approximately 0.4% of the annually nationwide livebirth population (15 million in 2015), and likely represented contemporaneous perinatal-neonatal care in certain proportion of sub-provincial regions and population as well as SES in China. From the 2015 study [13, 14], we moved forward to focus on detailed information of neonatal hospitalization and long-term outcomes of survival through infancy. We assumed that both IMR and NMR and potentially causal relations associated with perinatal risks may be derived, that the reliability and applicability of methodology be tested as a paradigm in vital statistics. We aimed to construct livebirth population-based norm of survival in analyzing regional NMR, IMR and associated relative risks of perinatal origin for genuine comparison with international data sources.
Methods
Study population, data sources and ethics approval
The source population included the whole regional livebirths with maternal and neonatal information from all obstetrical departments, neonatal wards and/or neonatal intensive care units (NICU) in Huai’an, by prospective data collection from 1 January to 31 December in 2015 [13, 14]. To obtain death information of all liveborn infants, we retrieved all death reports in the original birth database to identify the major causes of deaths of livebirths at delivery, as well as all hospitalized neonatal case records by redefining causes of in-hospital deaths. For those infant deaths without admission into, or after discharge from, any neonatal ward or NICU were classified as out-of-hospital deaths, which were derived from regional death report system (MCHSS) after verification of corresponding clinical records. By integrating the data of all infant deaths from the two sources, a new integrated database was established as a cohort linking information of livebirths, neonatal hospitalization and/or infant death for final analysis [15]. Works of retrospective data collection and analysis were conducted in 2018-2021. A study flow chart of the cohort linkage, data of infants excluded and included are shown in Fig. 1.
The study protocol was approved by the ethics committee of Children’s Hospital of Fudan University, and adopted by the Huai’an Women and Children’s Hospital and all other participating hospitals in Huai’an [13,14,15]. As no specific intervention was applied, informed consent from parents/guardians was waived.
Definitions of variables
Definitions regarding vital statistics were based on the original survey [13, 14] and diagnoses of any diseases were defined and categorized according to established clinical diagnostic criteria and the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) [16]. Briefly, livebirth was defined as birth presenting with any signs of life, such as breaths, heart beating, pulsation of the umbilical cord, or definite movement of voluntary muscles [16]. Perinatal variables included maternal and neonatal demographics and medical conditions. Maternal demographic characteristics and SES such as maternal age, urban or rural residency, educational level and prenatal care were included. Inadequate prenatal care was defined as fewer than six visits (half of the recommended average times) to any prenatal care facility during the pregnancy [17]. In addition, major co-morbidities/complications of pregnancy were included such as hypertensive disorder of pregnancy (HDP), gestational diabetes of mellitus (GDM), moderate-to-severe anemia, prelabor rupture of membrane (PROM), abnormalities of placenta and umbilical cord, antenatal steroids, multiple births, amniotic fluid (AF) contamination, fetal distress and mode of delivery [14]. As for neonatal variables, GA was classified with 6 subgroups: 25+ 0- 27+ 6 weeks (extreme preterm or EPT, no livebirths in GA < 25 weeks), 28+ 0-31+ 6 weeks (very preterm, VPT), 32+ 0-36+ 6 weeks (moderate-late preterm), 37+ 0-38+ 6 weeks (early term), 39+ 0-41+ 6 weeks (full term), > 42+ 0 weeks (post-term); and birthweight (BW) with 5 subgroups: < 1000 g (extremely low BW, ELBW), 1000-1499 g (very low BW, VLBW), 1500-2499 g (low BW), 2500-3999 g (normal BW), > 4000 g (macrosomia) [16]. GA < 37 weeks and BW < 2500 g were defined as preterm and LBW, respectively. Other variables for neonatal status and exposed risks included sex, small for GA (SGA), resuscitation at delivery room (DR), Apgar score, congenital anomalies, and neonatal hospitalization. The need for in-hospital care was defined as admissions into any neonatal ward or NICU within neonatal period (0-27 postnatal days) for term births or within adjusted GA of preterm infants equivalent to 28 postnatal days for term births. All the above-mentioned perinatal and neonatal diagnoses or definitions were consistent with previous studies [11,12,13,14,15].
As for the cohort outcome, neonatal mortality as deaths within 28 postnatal days (PND) and infant mortality was defined as deaths during infancy (0-364 PND). Besides, infant deaths were classified into three periods: 0-6 days as early neonatal deaths (including deaths at delivery); 7-27 days as late neonatal deaths; and 28-364 days as postneonatal deaths. The causes of death were classified into 4 main categories with respective codes following ICD-10 guidelines: (1) perinatal conditions, P00-P96; (2) congenital anomalies, Q00-Q99; (3) sudden unexpected death in infancy (SUDI), V01-Y89 and R00-R99; and (4) other causes, all other codes [16, 18].
Statistical analysis
Statistical analysis was performed using SPSS 23.0 (IBM, Chicago, IL), with figures produced by GraphPad PRISM 6.02 (GraphPad Software, La Jolla, CA). Data are presented as number (n) and rate in percent (%) or per thousand (‰). For descriptive analysis, we compared basic characteristics between the cohorts with or without neonatal hospitalization in those of preterm or non-preterm (term and post-term) with Pearson Chi-square test or Fisher exact test for group comparison, as well as of all livebirths with the adjustment of preterm by Cochran-Mantel-Haenszel tests. The total NMR and IMR were calculated by the number of deaths referring to total livebirths with further analyzed by GA or BW strata as well as cause-specific classification. The 95% confidence interval (CI) of rate was estimated by a null multilevel Poisson model with empirical, robust standard errors but no explanatory variables [19]. GA or BW stratified survival during neonatal and postneonatal periods was determined using Kaplan-Meier survival analysis.
The relative risk (RR) and 95% CI of GA and BW for neonatal and infant mortality were estimated by a generalized linear model of Poisson regression with robust variance [19, 20], with GA 39-41 weeks and BW 2500-3999 g as reference, respectively. Population attributable fraction (PAF) of each subgroups was calculated as: PAFi = pi*(RRi - 1)/[1 + Σn i = 1pi*(RRi - 1)]. RRi and pi respectively represented relative risk and prevalence in the target population for the ith level of risk factors, with n as the total number of exposure levels [21]. This equation evaluated the proportional reduction expected in the subgroup individuals if the known level of risk factors were eliminated from the target population. An example of this calculation was shown in additional file 1.
Uni- and multivariable Cox regression models were used to examine the hazard ratio (HR) and 95%CI of perinatal risks associated with infant mortality. Perinatal risks included all the maternal and neonatal factors mentioned above. Selected adjustments were based on the final step of multivariable regression model with backward stepwise selection. Since the proportionality assumption was violated in the infant mortality analyses, the follow-up time was also split into early-, late-neonatal and postneonatal periods as defined above. All the survivals at the initial days of each period entered the cohort and were analyzed. The validity of the proportionality assumptions of the Cox model of deaths in these three periods was evaluated by testing Schoenfield residuals [22, 23]. P < 0.05 was considered statistically significant.
Results
Descriptive analysis for livebirth cohort
In the current cohort of the whole regional birth population, 59,056 livebirths were included (by excluding 189 stillbirths). There were 213 neonatal and 291 infant deaths, with the livebirth prevalence of NMR and IMR were 3.6‰ (95% CI 3.2‰, 4.1‰), and 4.9‰ (4.4‰, 5.5‰), respectively. Among all livebirths, 35 died at delivery with the incidence of 0.6‰ (0.4‰, 0.8‰). The incidence rates of preterm and LBW were 4.3% (4.1%, 4.4%) and 3.1% (3.0%, 3.3%), respectively. Totally, 7960 neonates were hospitalized [13.5% (13.2%, 13.8%)] and 168 [2.8‰ (2.5‰, 3.3‰)] died during their hospitalization, which contributed to 57.7% of the total infant deaths (Table 1).
Table 1 lists the basic information of perinatal characteristics and infant outcome among hospitalized and non-hospitalized neonates by preterm or non-preterm (term and post-term) strata. In comparison to non-preterm livebirths, those livebirths with GA < 37 weeks presented with higher rates of mothers with early or late childbearing, less rural residency and lower education level, as well as more co-morbidities/complications, such as HDP, GDP, PROM, abnormalities of placenta, antenatal steroids, and cesarean delivery, regardless of hospitalization (P < 0.05). Compared to those without hospitalization, hospitalized neonates generally presented higher prevalence of maternal co-morbidities/complications, LBW, low Apgar scores, rigorous DR resuscitation and congenital anomalies, especially in those of preterm (P < 0.05). As for the outcome, infants with neonatal hospitalization accounted for 69.4% (202/291) of total infant deaths, with 71.9% (110/153), 93.3% (56/60) and 46.2% (36/78) as early-, late-neonatal and postneonatal mortalities, respectively. For those without hospitalization, deaths of preterm infants were 90.0% occurred at delivery (27/30), but of term ones mainly at postneonatal period (39/59, 66.1%).
GA and BW stratified NMR and IMR
Table 2 lists the stratified rates for NMR and IMR by GA and BW strata, with the detailed numbers of each week listed in Table S1 and BW in increment of 250 g in Table S2. There were 77.2% (1941/2514) of preterm and 73.5% (1358/1848) LBW hospitalized, with 81.5% and 84.0%, respectively, admitted on the first postnatal day. Since the large proportion of DR deaths existed in newborns of GA < 28 weeks (12/54, 22.2%) and BW < 1000 g (14/34, 41.2%), in-hospital rates of EPT (74.1%) and ELBW (58.8%) were relatively lower than other preterm and LBW strata (70-90%) (Table S1, S2). The IMR for preterm and LBW were 4.9% (123/2514) and 7.0% (129/1848) while for those of GA < 32 weeks and BW < 1500 g, 27.0% (86/319) and 31.7% (78/246), respectively, with > 80% occurred in the neonatal period.
Table 2 also demonstrates RR and PAF of neonatal and infant mortality by GA and BW strata. It showed that both preterm and LBW had higher risks of deaths, and contributed to a population level risk (PAF) of neonatal deaths of 50% and infant deaths of 40%, respectively. In both neonatal and infant periods, although the RR of EPT or ELBW were the highest (RR > 200), the small proportion constituted a relatively lower PAF (10%) than those of VPT and VLBW (RR > 50, PAF 15-25%). Notably, early term infants presented a PAF of 10.7% for NMR and 7.6% for IMR even with small RR, whereas macrosomia was associated with decreased death risk with PAF < 0.
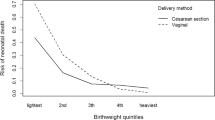
Figure 2 shows the GA or BW stratified neonatal and postneonatal survival, which suggested that deaths within 28 PND accounted for large part (> 70%) of total infant deaths. The 50% of one-year survival rates of all livebirths were at GA 25-27 weeks and BW < 1000 g, while the total survival rates for those with GA 28-31 weeks and BW 1500-1499 g were > 75%, and > 95% for those with GA > 32 weeks and BW > 1500 g.
Causes of neonatal and infant mortality
As Table 3 and Fig. 3 shown, the major cause categorized IMR were perinatal conditions (2.6‰), congenital anomalies (1.5‰), SUDI (0.6‰) and other causes (0.2‰). Perinatal conditions contributed to 65.7% NMR and 53.3% IMR while that for congenital anomalies, 31.9% and 30.9%, respectively. In preterm and LBW deaths, perinatal conditions accounted for 80.5% (99/123) and 76.0% (98/129) IMR, respectively, especially in those with GA < 32 weeks (77/86, 89.5%) and BW < 1500 g (73/78, 93.6%). The proportion of congenital anomalies increased with GA and BW advancing. The deaths due to SUDI and other causes, though very few, occurred mainly in term and normal BW infants and postneonatal period. Out-of-hospital deaths occurred mainly in term, regular BW and postneonatal period, together with that of SUDI and congenital anomalies being the main causes of infant deaths (Table S3).
Multivariable adjusted perinatal risks
The multivariable Cox regression analyses of adjusted HR (aHR) of perinatal risks associated with infant mortality over different periods are shown in Table 4 (with univariable analyses listed in Table S4). In early neonatal period, BW < 1000 g and low Apgar score were associated with high risks (aHRs > 10) for deaths, while moderate risks (aHRs 3-5) were found in GA < 32 weeks, BW 1000-1499 g, congenital anomalies and neonatal hospitalization. Both maternal high education level and antenatal steroids markedly lowered the risks for early neonatal deaths, whereas abnormality of umbilical cord and AF contamination had increased risks (aHRs 2). In late neonatal period, death risks were strongly associated with BW < 1500 g, GA > 42 weeks, congenital anomalies and neonatal hospitalization (aHRs ranged from 9 to 90). In postneonatal period, aHR of GA < 28 weeks was as high as 33.31 (12.23, 90.72), whereas BW in strata contributed less significantly to the death hence being removed from the multivariable model. Maternal education > 9 years was also associated with lower risks with aHR of 0.59 (0.36, 0.97). A moderate-to-strong association of congenital anomalies [aHR 6.90 (3.61, 13.19)] and neonatal hospitalization [aHR 3.30 (1.91, 5.71)] with death was also shown in posteneonatal period. SGA was only significantly associated with early neonatal death in the univariable regression analysis (HR 2.81), but not associated with either neonatal or infant death in the multivariable analysis.
Discussion
This cohort study reported the neonatal and infant mortality rates based on all livebirths and hospitalized neonatal population in Huai’an in 2015. The major findings revealed the survival outcome of all hospitalized livebirths along with those non-hospitalized. It showed the regional NMR and IMR with further stratification by GA and BW, and the major causes of infant deaths as perinatal conditions and congenital anomalies in the target population. Perinatal risks associated with the mortalities over whole infancy period were low GA and BW, congenital anomalies and neonatal hospitalization, whereas maternal SES and pregnancy co-morbidities/complications presented mild risks. This is an important progression in that the potentially causal relations between infant mortality and perinatal risks were clearly depicted. Our effort to the establishment of concept and methodology for the current data file should be complementary to the previous achievements through nationwide campaign [1,2,3, 6, 7, 11,12,13,14].
Representativeness of the source populations
Huai’an is an emerging rural prefectural region of Jiangsu province, with a population of 5.6 million, approximately 0.4% of the total national population (1.37 billion), 56.1% urban residents, gross domestic production (GDP) of 274.5 billion Chinese Yuan (CNY, 6.2 = 1 USD), contributing to approximately 0.4% of total national GDP (67.67 trillion CNY) in 2015 [24, 25]. The average GDP per capita at 56,575 CNY in Huai’an was modestly above the corresponding national average (49,228 CNY), or in the third quartile range [24, 25]. Based on this SES background, we managed to have set up the linkage of livebirths and hospitalized neonatal data with perinatal information as source population basis for the infant outcomes in this whole sub-provincial region. As reported from this survey, the NMR and IMR in Huai’an were 3.6‰ and 4.9‰, whereas the nationally reported corresponding data were 5.4‰ and 8.1‰, respectively, in 2015 [24]. As there should exist large regional variations in China, our data file should have minimized over- or underestimation of the real status due to hospital sampling, lower efficient care standard, criteria of vital statistics excluding GA < 28 weeks births, or inaccurate livebirth counting at delivery, among other bias and confounding factors [1,2,3, 6–7]. Our previous participations of nationwide multi-center studies on the management and outcome of neonatal respiratory failure verified that the neonatal care level of Huai’an was above the national average [26,27,28], taken the regional SES into account [24, 25]. We thereby assumed that the regional maternal-infant healthcare, as reflected by the neonatal and infant outcome, may represent up to 20% of the sub-provincial (prefectural) regions, or 25% of the population, in other words, standing at the third quartile of SES and maternal-infant healthcare level of the country, mainly in the eastern, coastal provinces [2, 6, 24].
Neonatal care in regional perinatal-neonatal network infrastructure
In comparison with the 2010 study, the hospitalized rate and in-hospital deaths rate in Huai’an were both higher in 2015 (13.5% vs. 11.3%, 2.8‰ vs. 2.4‰) [11]. These were associated with more centralized hospital delivery, adequate prenatal care for high-risk pregnancy, increased preterm livebirths [11,12,13,14]. It highlighted the progress of regional maternal and child healthcare coupling with the implementation of universal health insurance for maternal-infant healthcare since 2010 as well as the substantial SES advancement [24, 25]. In the current study, neonatal hospitalization was associated with maternal co-morbidities/complications, but marked associations were found with neonatal factors of moderate-to-severe morbidities such as being preterm birth, LBW, low Apgar scores, rigorous DR resuscitation and congenital anomalies. It indicated the efficiency of perinatal-neonatal healthcare system in the management of very and critically ill neonates as the most very and extremely preterm births were vigorously handled at birth and adequately hospitalized. Such information is not available from hospital admission-based sample population for neonatal and infant outcome in China [29, 30]. This study’s methodology and outcome measurements may serve as a paradigm for other evolving regions and countries to evaluate inter-regional or inter-institutional perinatal-neonatal healthcare efficiency and quality improvement.
Causes-specific infant mortalities
As for the causes of infant death, perinatal risks and congenital anomalies accounted for 80% (mainly preterm and term infants, respectively). Prevalence of congenital anomalies differed in regions since it was closely related to SES and maternal status as well as diagnostic capacity [11, 13, 31, 32]. In this study, the prevalence of congenital anomalies was 13.4 per 1000 livebirths which was doubled from 6.8 per 1000 births in 2010 [11], a difference due to the inclusion of those diagnosed during hospitalization beyond first postnatal week or not [11, 12]. Although there was an apparently upward trend, it was still lower than financially well-off regions [31, 33] when the higher mortality rates remained [34, 35]. It is imperative to have a unified definition for reporting birth, livebirth, perinatal or hospitalization related birth defects or congenital anomalies, in order to estimate prevalence and causation of NMR and IMR in the context of prenatal screening and precise diagnostic process postnatally through early infancy [36]. The relative burden of mortality due to SUDI was a profound challenge in postneonatal infancy, calling for proper parental training through enhanced community-based, family-centered, maternal-infant healthcare.
Perinatal risks associated with neonatal and infant mortality
The fact that maternal low education level and rural residency had higher risks of neonatal and postneonatal mortalities reflected the impact of SES on parental attitude towards critically ill newborns and financial support for ongoing medical care [11,12,13,14, 22]. In contrast, maternal morbidities only had modest impact on neonatal, but not the postneonatal, infant deaths. Our previous studies also demonstrated that high-risk pregnancy had an ambiguous association with perinatal mortality [12, 14]. Even in well developed countries, severe maternal morbidities conferred increased risks of infant mortality [RR 2.93 (2.51, 3.41)] [37]. In-depth analyses are needed to explore the severity of maternal morbidities in relation to infant outcome in resource-limited, evolving regions and countries.
Unlike the aforementioned maternal risk factors, neonatal morbidities had more profound and persistent effects on livebirth outcome. As reported, severe neonatal morbidities still exerted 3-4 times higher risks for postneonatal to under-5 mortalities [23] and increased need for rehospitalization between 1 and 6 years of age [38]. Recently, a large cohort study in Sweden also suggested that perinatal factors such as moderate or late preterm, SGA, malformations, low Apgar scores and admission to neonatal care were all associated with long-term neurodevelopmental disorder [39]. In the current study, preterm and LBW attributed to as high as 40-50% population level risks to neonatal and infant deaths. Moreover, early term infants still exerted 8-10% PAF even with small RR of deaths. Despite that those with GA < 32 weeks and BW < 1500 g presented with > 70% survival rates, lower GA and BW remained potent predictors for both neonatal and postneonatal mortalities as expected. To be noted, both neonatal and infant survival rates for livebirths of EPT were about 40-50%, and 20-30% of ELBW in current study, which were significantly lower than 80-90% reported by developed countries [9, 10, 40]. The highest RR and HR of EPT/ELBW for neonatal and infant death also indicated that the survival improvements for extremely premature infants remained the big challenge for local perinatal-neonatal care system. It is intriguing that SGA was not a risk for either neonatal or infant death in our multivariable Cox regression models. In general, SGA (< 3rd percentile) may be modestly associated with increased risks by 1-2 times in both neonatal and postneonatal mortality [41, 42]. However, recent study based on the whole livebirths in US and Norway reported that SGA was poorly predictive of neonatal mortality and cerebral palsy, while GA and BW predicted well [43]. The inconsistent definitions of SGA, and the inclusion of GA and BW in the adjusted model might contribute to the variations.
Strengths and limitations
This study carried out a comprehensive analysis of outcome of livebirth, neonatal hospitalization and perinatal risks associated with neonatal and infant mortalities depicted in the early-, late-neonatal and postneonatal periods of infancy. With the PAF as part of the datafile, population-level prevalence and risks of neonatal and infant death in GA and BW categories were derived, which should be served as a quantitative indicator for inter-regional comparisons of the care efficiency of those with small GA or BW. The four major categories of causes of all infant death recommended by WHO ICD-10 were simple and convenient to operate. The source population was representative with regard to SES and perinatal-neonatal care standard, which may facilitate the extrapolation of the findings and serve as a benchmark for future study to validate.
Although we managed to minimize bias by scrutinizing clinical case records, retrospective linkage of database might be insufficient to the quality assurance in terms of accuracy and completeness. Even so, the proportion of unlinked livebirths was low (< 1%) and the linkage of all deaths was optimally managed. Besides, the consistence of data sources and underlying diseases for those out-of-hospital deaths might be influenced due to insufficient information of postneonatal hospitalization. However, with the unified morbidity and mortality definitions, analysis of the specific causes of in-hospital deaths should be applicable. Finally, variations of clinical practice standard across the network hospitals might exist under current cause categories of infant deaths. While its representativeness as source population and potentially causal relations of the risks to the outcome requires further validation, the merit of study concept, methodology and outcome measurements should be applicable in evolving regions and countries for evaluation of maternal-infant healthcare improvement taking SES into consideration.
Conclusions
This cohort study provided a comprehensive and detailed data file of the outcome of livebirths and hospitalized neonates, depicting as NMR, IMR, and major causes of infant death associated with perinatal, neonatal and postneonatal risks in particular periods of infancy, in Huai’an, China. It reflects the progression and efficiency of contemporary maternal-infant healthcare with universal insurance policy in a particular regional livebirth population. The study concept, applicability and representativeness may be adopted and validated by other evolving regions or even amplified for provincial annual birth size (of 10-100 million residents in most of the 31 provinces/autonomous regions) for the same purpose.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available due to other concurrent studies based on the datasets but are available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Amniotic fluid
- aHR:
-
Adjusted hazard ratio
- BW:
-
Birthweight
- CI:
-
Confidence interval
- CNY:
-
Chinese Yuan
- DR:
-
Delivery room
- ELBW:
-
Extremely low birthweight
- EPT:
-
Extreme preterm
- GA:
-
Gestational age
- GDM:
-
Gestational diabetes of mellitus
- GDP:
-
Gross domestic production
- HR:
-
Hazard ratio
- ICD:
-
International Statistical Classification of Diseases
- HDP:
-
Hypertensive disorder of pregnancy
- IMR:
-
Infant mortality rate
- LBW:
-
Low birthweight
- MCHSS:
-
Maternal and Child Health Surveillance System
- NICU:
-
Neonatal intensive care units
- NMR:
-
Neonatal mortality rate
- PAF:
-
Population attributable fraction
- PND:
-
Postnatal days
- PROM:
-
Prelabor rupture of membrane
- RR:
-
Relative risk
- SES:
-
Socioeconomic status
- SGA:
-
Small for gestational age
- SUDI:
-
Sudden unexpected death in infancy
- VLBW:
-
Very low birthweight
- VPT:
-
Very preterm
References
Feng X, Guo S, Hipgrave D, Zhu J, Zhang L, Song L, et al. China’s facility-based birth strategy and neonatal mortality: a population-based epidemiological study. Lancet. 2011;378:1493–500.
He C, Liu L, Chu Y, Perin J, Dai L, Li X, et al. National and subnational all-cause and cause-specific child mortality in China, 1996-2015: a systematic analysis with implications for the Sustainable Development Goals. Lancet Glob Health. 2017;5:186–97.
Wang Y, Li X, Zhou M, Luo S, Liang J, Liddell CA, et al. Under-5 mortality in 2851 Chinese counties, 1996-2012: a subnational assessment of achieving MDG 4 goals in China. Lancet. 2016;387:273–83.
United Nations Inter-agency Group for Child Mortality Estimation. Available from: http://www.childmortality.org/data/. Accessed 6 July 2021.
Sun B, Shao X, Cao Y, Xia S, Yue H. Neonatal-perinatal medicine in a transitional period of China. Arch Dis Child Fetal Neonatal Ed. 2013;98:440–4.
Liang J, Mao M, Dai L, Li X, Miao L, Li Q, et al. Neonatal mortality due to preterm birth at 28-36 weeks’ gestation in China, 2003-2008. Paediatr Perinat Epidemiol. 2011;25:593–600.
Zhao P, Han X, You L, Zhao Y, Yang L, Liu Y. Effect of basic public health service project on neonatal health services and neonatal mortality in China: a longitudinal time-series study. BMJ Open. 2020;10:e034427.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84.
Norman M, Hallberg B, Abrahamsson T, Björklund LJ, Domellöf M, Farooqi A, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;321:1188–99.
Haumont D, Modi N, Saugstad OD, Antetere R, NguyenBa C, Turner M, et al. Evaluating preterm care across Europe using the eNewborn European Network database. Pediatr Res. 2020;88:484–95.
Sun L, Yue H, Sun B, Han L, Qi M, Tian Z, et al. Estimation of birth population-based perinatal-neonatal mortality and preterm rate in China from a regional survey in 2010. J Matern Fetal Neonatal Med. 2013;26:1641–8.
Sun L, Yue H, Sun B, Han L, Tian Z, Qi M, et al. Estimation of high risk pregnancy contributing to perinatal morbidity and mortality from a birth population-based regional survey in 2010 in China. BMC Pregnancy Childbirth. 2014;14:338.
Wang H, Yue H, Sun B, Zhu X, Niu H, Qi T, et al. Birth population survey in Huai'an in 2015: perinatal-neonatal mortality and preterm birth rate in emerging regions in China. J Matern Fetal Neonatal Med. 2020;33:838–46.
Zhu X, Niu H, Wang H, Li X, Qi T, Ding W, et al. High risk pregnancy associated perinatal morbidity and mortality: a second birth population-based survey in Huai’an in 2015. BMC Pregnancy Childbirth. 2019;19:224.
Guo X, Li X, Qi T, Pan Z, Zhu X, Wang H, et al. A birth population-based survey of preterm morbidity and mortality by gestational age. BMC Pregnancy Childbirth. 2021;21:291.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 1993.
Debessai Y, Costanian C, Roy M, El-Sayed M, Tamim H. Inadequate prenatal care use among Canadian mothers: findings from the Maternity Experiences Survey. J Perinatol. 2016;36:420–6.
Bairoliya N, Fink G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study. PLoS Med. 2018;15:e1002531.
Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6.
Shah R, Mullany LC, Darmstadt GL, Talukder RR, Rahman SM, Mannan I, et al. Neonatal mortality risks among preterm births in a rural Bangladeshi cohort. Paediatr Perinat Epidemiol. 2014;28:510–20.
WHO Quantifying the contribution of risk factors to the burden of disease. http://www.who.int/healthinfo/global_burden_disease/metrics_paf/en/. Accessed 6 July 2021.
Ezeh OK, Agho KE, Dibley MJ, Hall JJ, Page AN. Risk factors for postneonatal, infant, child and under-5 mortality in Nigeria: a pooled cross-sectional analysis. BMJ Open. 2015;5:e006779.
Stephens AS, Lain SJ, Roberts CL, Bowen JR, Nassar N. Association of gestational age and severe neonatal morbidity with mortality in early childhood. Paediatr Perinat Epidemiol. 2016;30:583–93.
National Bureau of Statistics of China. Available from: http://www.stats.gov.cn/. Accessed 6 July 2021. (in Chinese).
Statistical yearbook by Huaian government. Available from: http://www.huaian.gov.cn/col/. Accessed 6 July 2021. (in Chinese).
Wang H, Gao X, Liu C, Yan C, Lin X, Yang C, et al. Morbidity and mortality of neonatal respiratory failure in China: surfactant treatment in very immature infants. Pediatrics. 2012;129:e731–40.
Wang YF, Liu CQ, Gao XR, Yang CY, Shan RB, Zhuang DY, et al. Effects of inhaled nitric oxide in neonatal hypoxemic respiratory failure from a multicenter controlled trial. Chin Med J. 2011;124:1156–63.
Wang H, Gao X, Liu C, Yan C, Lin X, Dong Y, et al. Surfactant reduced the mortality of neonates with birth weight ⩾1500 g and hypoxemic respiratory failure: a survey from an emerging NICU network. J Perinatol. 2017;37:645–51.
Wei KL, Yang YJ, Yao YJ, Du LZ, Wang QH, Wang RH, et al. Epidemiologic survey on hospitalized neonates in China. Transl Pediatr. 2012;1:15–22.
Kong X, Xu F, Wu R, Wu H, Ju R, Zhao X, et al. Neonatal mortality and morbidity among infants between 24 to 31 complete weeks: a multicenter survey in China from 2013 to 2014. BMC Pediatr. 2016;16:174.
Zhang X, Chen L, Wang X, Wang X, Jia M, Ni S, et al. Changes in maternal age and prevalence of congenital anomalies during the enactment of China’s universal two-child policy (2013-2017) in Zhejiang Province, China: An observational study. PLoS Med. 2020;17:e1003047.
Xiong L, Xu Z, Wang H, Liu Z, Xie D, Wang A, et al. The association between ambient air pollution and birth defects in four cities in Hunan province, China, from 2014 to 2016. Medicine (Baltimore). 2019;98:e14253.
Li Y, Liu XH, Wang FY, Zhao XL, Zhang X, Zhang YP. Analysis of the birth defects among 61 272 live born infants in Beijing. Beijing Da Xue Xue Bao. 2009;41:414–7.
Cao H, Wang J, Li Y, Li D, Guo J, Hu Y, et al. Trend analysis of mortality rates and causes of death in children under 5 years old in Beijing, China from 1992 to 2015 and forecast of mortality into the future: an entire population-based epidemiological study. BMJ Open. 2017;7:e015941.
Huang YH, Wu QJ, Li LL, Li D, Li J, Zhou C, et al. Different extent in decline of infant mortality by region and cause in Shenyang. China Sci Rep. 2016;6:24527.
Best KE, Rankin J, Dolk H, Loane M, Haeusler M, Nelen V, et al. Multilevel analyses of related public health indicators: The European Surveillance of Congenital Anomalies (EUROCAT) public health indicators. Paediatr Perinat Epidemiol. 2020;34:122–9.
Aoyama K, Park AL, Davidson AJF, Ray JG. Severe maternal morbidity and infant mortality in Canada. Pediatrics. 2020;146:e20193870.
Stephens AS, Lain SJ, Roberts CL, Bowen JR, Simpson JM, Nassar N. Hospitalisations from 1 to 6 years of age: effects of gestational age and severe neonatal morbidity. Paediatr Perinat Epidemiol. 2015;29:241–9.
Jöud A, Sehlstedt A, Källén K, Westbom L, Rylander L. Associations between antenatal and perinatal risk factors and cerebral palsy: a Swedish cohort study. BMJ Open. 2020;10:e038453.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–25.
Ludvigsson JF, Lu D, Hammarström L, Cnattingius S, Fang F. Small for gestational age and risk of childhood mortality: a Swedish population study. PLoS Med. 2018;15:e1002717.
Wilcox AJ, Cortese M, McConnaughey DR, Moster D, Basso O. The limits of small-for-gestational-age as a high-risk category. Eur J Epidemiol. 2021;36:985–91.
Acknowledgements
The authors thank the cooperation from the Huai’an perinatal-neonatal study group members, specifically to Drs. M. Zhang, H. Guan, J. Yang, S. Li, K. Zhu, C. Tang, M. Dong, Y. Yin, X. Cao, J. Zhang, H. Liu, Z. Xu, C. Gao and Y. Heng; and contribution of Drs S. Luo and M. Chen in data collection is highly appreciated. The authors are very grateful to Dr. Guoyou Qin, the Department of Biostatistics, School of Public Health of Fudan University, for his critical review of all the data analysis, presentation and interpretation.
CONSORTIUM NAME.
Huai’an Perinatal-Neonatal Study Group.
Members:
Zhaojun Pan2; Guofang Zheng2; Sufang Ding1; Xiaoqiong Li3; Tingting Qi3; Xiaoqin Zhu4; Hui Wang4; Weijie Ding4; Hongni Yue2,4; Zhaofang Tian5; Muling Zhang5; Haijun Wang6; Yaodong Yin6; Honghua Guan7; Juan Yang7; Yongjian Wu8; Tao Xu9; Chunhong Tang10; Maotian Dong10; Chunhua Zhang11; Chunqin Dong12; Sumei Zhou13; Yani Lei14; Shouzhong Li15; Keyan Zhu15; Xia Zhao16; Bi Xue17; Zhaoxia Wang18; Shucheng Wang19; Hong Liu20; Zhou Xu20; Chuntao Yuan21; Xihui Cao22; Jianya Zhang22; Bu Xu23; Wenlong Lin23; Cui Gao24; Yongbo Heng24; Lei Wang25; Moqing Wang25.
Affiliations:
7Huai’an Second People’s (General) Hospital, Huai’an, Jiangsu, China; 8Huai’an Traditional Chinese Medicine Hospital, Huai’an, Jiangsu, China; 9PLA 82nd General Hospital (uniformed service), Huai’an, Jiangsu, China; 10Huai’an District Hospital, Huai’an, Jiangsu, China; 11Huai’an District Maternity Hospital, Huai’an, Jiangsu, China; 12Huai’an District Xinqu Hospital, Huai’an, Jiangsu, China; 13Huai’an City Xiehe Hospital, Huai’an, Jiangsu, China; 14The First Division of Huaian First People’s (General) Hospital, Huai’an, Jiangsu, China; 15Huaiyin District Hospital, Huai’an, Jiangsu, China; 16Huaiyin District Maternity Hospital, Huai’an, Jiangsu, China; 17Lianshui Second People’s (General) Hospital, Huai’an, Jiangsu, China; 18Lianshui County Third People’s (General) Hospital, Huai’an, Jiangsu, China; 19Lianshui County Traditional Chinese Medicine Hospital, Huai’an, Jiangsu, China; 20Hongze County Traditional Chinese Medicine Hospital, Huai’an, Jiangsu, China; 21Hongze County Maternity Hospital, Huai’an, Jiangsu, China; 22Xuyi County People’s (General) Hospital, Huai’an, Jiangsu, China; 23Xuyi County Traditional Chinese Medicine Hospital, Huai’an, Jiangsu, China; 24Jinhu County People’s (General) Hospital, Huai’an, Jiangsu, China; 25Jinhu County Traditional Chinese Medicine Hospital, Huai’an, Jiangsu, China.
Authors’ contributors
Yaling Xu executed the study protocol, data collection and analysis, drafted and revised manuscript; Xiaojing Guo engaged in data collection and analysis, and critically revised manuscript; Zhaojun Pan, Guofang Zheng, Xiaoqiong Li, Tingting Qi supervised and validated clinical data collection and analysis, and reviewed manuscript; Xiaoqin Zhu, Hui Wang, Weijie Ding, Zhaofang Tian, Haijun Wang carried out data collection and analysis, and reviewed manuscript; Hongni Yue conceptualized and designed the study, coordinated and supervised data collection and analysis, and critically revised manuscript; Bo Sun conceptualized and designed the study, supervised data analysis, and critically revised manuscript.
Funding
Supported by a grant from the Project of Maternal and Child Health Care by Jiangsu Provincial Commission of Health (F201402 [Yue H]), and from the Laboratory of Neonatal Diseases, National Commission of Health, and Children’s Hospital of Fudan University [Sun B].
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethics committee of Children’s Hospital of Fudan University approved the study design and protocol, and waived the need for consent (#2019-194). The same study design and protocol was also adopted and approved by ethics committee of Huai’an Women and Children’s Hospital and all participated hospitals in accordance with the Chinese regulations for clinical practice and investigation (www.nhc.gov.cn). The permissions and the names of the ethics committees and scientific committees (institutional review board) of the major participating hospitals are referred to reference 14 (Zhu X, et al. BMC Pregnancy Childbirth. 2019; 19(1): 224).
Consent for publication
Not applicable.
Competing interests
All the authors have declared no any financial and non-financial competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary method for population attributable fraction (PAF) of polytomous variable
Additional file 2 Table S1
Gestational age (GA) stratified rates of hospitalization and mortality
Additional file 3 Table S2
Birthweight (BW) stratified rates of hospitalization and mortality
Additional file 4 Table S3
Information of delivery room, in-hospital and out-of-hospital deaths
Additional file 5 Table S4
Univariable analysis of perinatal risk factors for infant mortality at different periods by Cox regression model
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, Y., Guo, X., Pan, Z. et al. Perinatal Risks of Neonatal and Infant Mortalities in a Sub-provincial Region of China: A Livebirth Population-based Cohort Study. BMC Pregnancy Childbirth 22, 338 (2022). https://doi.org/10.1186/s12884-022-04653-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04653-8