Abstract
Elderly patients aged 65 or older with acute myeloid leukemia (AML) have poor prognosis. The risk stratification based on genetic alteration has been proposed in national comprehensive cancer network (NCCN) guideline but its efficacy was not well verified especially in real world elderly patients. The nutritional status assessment using controlling nutritional status (CONUT) score is a prognostic biomarker in elderly patients with solid tumors but was not examined in elderly AML patients. We performed prospective analysis of genetic alterations of 174 patients aged 65 or older with newly diagnosed AML treated without hematopoietic stem cell transplantation (HSCT) and developed simplified CONUT (sCONUT) score by eliminating total lymphocyte count from the items to adapt AML patients. In this cohort, both the NCCN 2017 risk group and sCONUT score successfully stratified the overall survival (OS) of the elderly patients. A multivariable analysis demonstrated that adverse group in NCCN 2017 and high sCONUT score were independently associated with poor 2-year OS. Both risk stratification based on NCCN 2017 and sCONUT score predict prognosis in the elderly patients with newly diagnosed AML.
Similar content being viewed by others
Introduction
Elderly patients aged 65 or older with acute myeloid leukemia (AML) are often ineligible for hematopoietic stem cell transplantation (HSCT) and generally have a poor prognosis. Although this patient population represents majority of AML patients, currently used prognostic indices are mostly derived from younger patient data. Analysis of large-scale real world data of the elderly patients is warranted to confirm the efficacy of these prognostic indices. The prognostic risk classification based on national comprehensive cancer network (NCCN) Guidelines Version3. 2017; NCCN 20171 is widely used; however, the impact of this classification on the prognosis of such elderly AML patients is unclear. While nutritional status assessment using controlling nutritional status (CONUT) score2 based on serum level of albumin (Alb), total-cholesterol (T-chol), and total lymphocyte count (TLC) has been shown to predict prognosis of elderly patients with solid tumors and hematological malignancies such as multiple myeloma and malignant lymphoma3,4,5,6,7,8, its prognostic significance in elderly patients with AML remains to be clarified. In the current study, we aimed to determine the prognostic value of NCCN 2017 and nutritional status in elderly patients with newly diagnosed AML.
Patients and methods
Patients
Hokkaido Leukemia Net (HLN) prospectively collects AML samples from hospitals of North Japan Hematology Study Group (NJHSG). In this study, we focused on newly diagnosed AML patients aged 65 or older treated without HSCT and investigated cytogenetic and molecular abnormality of leukemic cells including FLT3-ITD, NPM1, CEBPA, and KIT, as previously described9. The presence of TP53 mutation was not determined in the present study. We stratified the patients into favorable, intermediate, and adverse risk groups based on NCCN 2017. A total of 174 patients aged 65 or older with AML treated without HSCT from 2010 to 2018 were enrolled in this study (Fig. S1). The study was conducted in compliance with the ethical principles based on the Declaration of Helsinki and was approved by the institutional review board of Hokkaido University Hospital (No. 015-0344). Written consent was obtained from each patient for the study participation.
Risk indices
The CONUT score was calculated from Alb (g/dL), T-chol (mg/dL) and TLC (/μL), as previously reported2 (Table 1A). Since AML patients often present low lymphocyte counts10, we developed simplified CONUT (sCONUT) score by eliminating TLC from evaluation criteria (Table 1B). The patients with score 3 or more at diagnosis were defined as high group. We also evaluated the following nutritional index for patients with evaluable data based on previous reports. The geriatric nutritional risk index (GNRI) score11 was calculated as 1.489 × Alb (g/L) + 41.7 × weight (kilograms)/ideal body weight, with ideal weight was calculated according to the Lorentz equations. The prognostic nutritional index (PNI) score12 was calculated as 10 × Alb (g/dL) + 0.005 × TLC (/μL). For GNRI and PNI, we defined the patients with higher score than median score as high group and patients with lower score as low group. The information about the weight and height (meters) was taken on the day of admission for all patients.
Statistical analysis
Overall survival (OS) was calculated from the day of diagnosis until death or last follow-up. The probability of OS was estimated using a Kaplan–Meier method, and differences between patient groups were analyzed using the log-rank test. The baseline patient characteristics were tabulated to check imbalance in the demographic information. The risk factor at diagnosis for OS was evaluated by multivariable Cox regression using stepwise variable selection. Death within 2-years from the day of diagnosis was defined as censoring for the Cox regression model. The differences of the treatment regimens were evaluated by X2-test. All P values were 2-sided and a P-value of 0.05 was used as the cutoff for statistical significance. All statistical analyses were performed with IBM SPSS Statistics 26 software.
Results
Patient characteristics
Baseline patient characteristics were listed in Table 2. A median patient age at diagnosis was 72 years, ranging from 65 to 93 years. All patients were investigated their cytogenetic and molecular abnormalities of leukemic cells, including FLT3-ITD, NPM1, CEBPA, and KIT at diagnosis. According to the NCCN 2017 stratification1, 22%, 58%, and 20% of the patients were classified their risk status as favorable, intermediate, and adverse, respectively. Both the body height and weight at diagnosis were available in 137 patients, and the median body mass index (BMI) was 24 ranging from 14 to 34. For blood sample test, complete blood count and differential white blood count were available in all 174 patients. The median TLC was 1.6 × 109/L, which was consistent with that in a previous study of AML patients10. Serum albumin levels at diagnosis were available in 152 patients with 4.0 g/dL as median level, ranging from 1.8 to 5.9 g/dL. Serum total cholesterol levels at diagnosis were available in 112 patients with 140 mg/dL as median level, ranging from 81 to 248 mg/dL. According to the CONUT scores2, 21%, 52%, 25%, and 2% of the patients were classified as normal, mild, moderate and severe group, respectively. For sCONUT scores, 68% of the patients were classified as low group and 32% as high group. Induction therapy based on decision of each physician varied according to risk factors of the disease and general status of patients. As shown in Table 2, 86.3% of the patients were initially treated with chemotherapy. The remaining 13.2% of the patients were treated with best supportive care. Overall, 57 patients achieved CR (33%; Table 2). The median OS was 15.2 months and the 5-year OS was 24.8% (Fig. 1).
The prognostic risk classification based on NCCN 2017
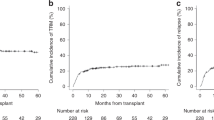
The risk classification based on NCCN 2017 successfully stratified the overall survival of the patients (5-year OS; favorable group, 41.5% vs. intermediate group, 22.5% vs. adverse group, 4.38%, P = 0.00000161, Fig. 2A).
CONUT score and sCONUT score as a prognostic biomarker
Based on the classic CONUT score classification, we found that OS was lower in moderate and severe groups, which was not significant (5-year OS; normal group, 18.6%; mild group, 22.3%; moderate group, 11.7%; severe group, 0.%, respectively, P = 0.0881, Fig. S2). This score did not work as a prognostic indicator with statistical significance. We hypothesized that inclusion of lymphocyte count, which was usually low in AML patients10, hampered to stratify prognosis in AML patients. We therefore developed the sCONUT score by simply omitting TLC from the 3 factors of the CONUT score. For sCONUT score, which stratify patients into 2 groups depend on scoring of 2 parameters, OS was significantly lower in patients with high sCONUT score than in those with low sCONUT score (5-year OS; 26.5% vs. 9.97%, P = 0.00145, Fig. 2B). Then, we investigated if the sCONUT score could further stratify risks of the patients in each NCCN 2017 risk group. While there were no significant prognostic impacts of the sCONUT score in patients with adverse and intermediate risk groups (Fig. 3A,B), there was a tendency in favorable risk group that patients with high sCONUT score had poorer prognosis than patients with low score (5-year OS; 42.3% vs. 0%, P = 0.0667, Fig. 3C). Because the poor nutritional status might be related to best supportive care option without chemotherapy, we further investigated subgroup analysis depends on treatment option. The significantly larger proportion of patients with high sCONUT score were treated without chemotherapy than the patients with low sCONUT score (33.3% vs. 8.2%, P = 0.0029, Fig. S3(A), S3(C)). On the other hand, we found no significant difference of the percentage of the patients treated without chemotherapy between NCCN-2017 risk groups (favorable; 18.2%, intermediate; 13.8%, adverse; 12.5%, P = 0.816, Fig. S2(D)). We additionally analyzed the outcome in patients treated with or without chemotherapy. In patients treated with chemotherapy, sCONUT score could stratify 89 patients into 2 groups with significantly different outcomes; sCONUT low (n = 67), sCONUT high (n = 22) (2-year OS, 42.1% vs. 21.6%, P = 0.0315, Fig. S3(E)). We found that all patients treated without chemotherapy had dismal prognosis, died within 300 days after diagnosis, and sCONUT score did not divide the prognosis (P = 0.152, Fig. S1(F)).
Univariate and multivariable analyses of clinical prognostic factors
We analyzed various prognostic factors for OS (Table 2). In a univariate analysis, GNRI score, PNI score and CONUT score were not associated with poor 2-year OS. On the other hand, higher age, adverse risk group based on NCCN 2017 classification, high sCONUT score, and not reached complete remission (CR) after first induction chemotherapy were associated with poor 2-year OS. We therefore performed multivariable analysis that included higher age, adverse risk group based on NCCN 2017 classification, high sCONUT score, and non-CR. In this multivariable analysis, adverse group in NCCN 2017 risk classification, and high sCONUT score and non-CR were independently associated with poor 2-year OS (NCCN 2017; HR 3.16; 95% CI 1.87–5.36, P = 0.0000189, simplified CONUT score; HR 1.76; 95% CI 1.11–2.78, P = 0.0163; non-CR; 2.82; 95% CI 1.70–5.71, P = 0.0000669; log-rank, Table 3).
Discussion
AML occurs in all age groups and is most common in patients older than 65 years13. Despite the development of lower-intensity treatment due to the discovery of novel agents, there is still no standard treatment of choice for the elderly patients with high risk AML14. However, some elderly patients are successfully treated with intensive chemotherapy. Hence, it is crucial to find prognostic biomarkers for elderly patients with newly diagnosed AML. Most commonly used prognostic risk classification, NCCN 2017 was developed based on data of younger patients1. In the current study, we find that the NCCN 2017 is also feasible for elderly patients with 65 years old or older.
The nutritional status assessments using GNRI; BMI and serum level of Alb, PNI; serum level of Alb and TLC, and CONUT score; serum level of Alb, TLC and T-chol, are developed to predict tolerability to cancer treatment in the elderly patients with solid tumors3,4,15,16,17. Recently, the CONUT score has been shown to predict prognosis in patients with some hematological malignancies5,6,7,8. However, the prognostic value in AML remained to be determined. In the current study, we clarified that these previously developed nutritional scores did not clearly stratify survival for elderly patients with newly diagnosed AML. We therefore developed the sCONUT score by simply omitting TLC from the 3 factors of the CONUT score as mentioned above. The sCONUT scoring can predict the prognosis of the elderly patients with AML. The sCONUT score is a useful and simple risk classification that can be easily calculated based on the result of blood sample test at diagnosis independent from NCCN disease risk score based on genetic alteration. It is important to know both disease factor and host nutritional status independently affect outcome in elderly AML patients. Especially for the elderly patients, assessment of nutritional status could be prioritized than disease risk assessment, as we showed that even patients with favorable risk group by NCCN 2017 classification could be further divided by nutritional status (Fig. 3C). Additionally, we demonstrated that the larger number of patients in sCONUT high groups were treated without chemotherapy compared with patients in sCONUT low groups and in patients treated with chemotherapy, sCONUT score could stratify 89 patients into 2 groups with significantly different outcomes. These results show that sCONUT score would be useful as a prognostic biomarker which directly affects the treatment choice of physicians and predict the prognosis of the patients treated with chemotherapy. Although assessment of general status is important especially in elderly patients, the assessment could be subjective and systematic scoring of geriatric analysis or fit status were too complicated to perform in clinical practice. sCONUT is a simple, objective and useful nutritional prognostic score that can be easily assessed in clinical practice and have a great potential as the indicator for choosing appropriate induction therapy in elderly AML patients. Our study has some limitations. Our cohort has limited sample size, lack of data about the consolidation therapy, and some patients lack biochemical data due to questionnaire-based retrospective data collection. Our real-world cohort includes heterogeneous patients with various comorbidities. It is obvious that comorbidities would have a huge impact on the nutritional status. We did not assess background complications resulting in poor nutritional status in each patient. Further investigation for comorbidity is needed in the future studies. At least, it was demonstrated that high sCONUT score at diagnosis is a poor prognostic factor in elderly AML patients and this is a notable result which can lead to future investigation.
In conclusion, we report that the prognostic risk classification based on AML disease status using NCCN Guidelines 2017 and new assessment scoring of patients’ nutritional status based on the sCONUT score can easily stratify elderly patients with newly diagnosed AML.
References
O’Donnell, M. R. et al. Acute myeloid leukemia, version 3.2017, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 15, 926–957. https://doi.org/10.6004/jnccn.2017.0116 (2017).
Ignacio de Ulibarri, J. et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 20, 38–45 (2005).
Takagi, K., Domagala, P., Polak, W. G., Buettner, S. & Ijzermans, J. N. M. The controlling nutritional status score and postoperative complication risk in gastrointestinal and hepatopancreatobiliary surgical oncology: a systematic review and meta-analysis. Ann. Nutr. Metab. 74, 303–312. https://doi.org/10.1159/000500233 (2019).
Ryo, S. et al. The controlling nutritional status score serves as a predictor of short- and long-term outcomes for patients with stage 2 or 3 gastric cancer: analysis of a multi-institutional data set. Ann. Surg. Oncol. 26, 456–464. https://doi.org/10.1245/s10434-018-07121-w (2019).
Kamiya, T. et al. The prognostic value of the controlling nutritional status score in patients with multiple myeloma. Leuk Lymphoma https://doi.org/10.1080/10428194.2020.1749608 (2020).
Nagata, A. et al. Clinical impact of controlling nutritional status (CONUT) score on the prognosis of patients with diffuse large B-cell lymphoma. Hematol. Oncol. https://doi.org/10.1002/hon.2732 (2020).
Okamoto, S. et al. Clinical impact of the CONUT score in patients with multiple myeloma. Ann. Hematol. 99, 113–119. https://doi.org/10.1007/s00277-019-03844-2 (2020).
Ureshino, H. et al. Clinical impact of the CONUT score and mogamulizumab in adult T cell leukemia/lymphoma. Ann. Hematol. 98, 465–471. https://doi.org/10.1007/s00277-018-3502-7 (2019).
Hidaka, D. et al. Wilms tumor 1 expression at diagnosis correlates with genetic abnormalities and polymorphism but is not independently prognostic in acute myelogenous leukemia: a hokkaido leukemia net study. Clin. Lymphoma Myeloma Leuk https://doi.org/10.1016/j.clml.2018.07.291 (2018).
Le Jeune, C. et al. Initial absolute lymphocyte count as a prognostic factor for outcome in acute myeloid leukemia. Leuk Lymphoma 55, 855–862. https://doi.org/10.3109/10428194.2013.813504 (2014).
Bouillanne, O. et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 82, 777–783. https://doi.org/10.1093/ajcn/82.4.777 (2005).
Onodera, T., Goseki, N. & Kosaki, G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85, 1001–1005 (1984).
Dohner, H., Weisdorf, D. J. & Bloomfield, C. D. Acute myeloid leukemia. N. Engl. J. Med. 373, 1136–1152. https://doi.org/10.1056/NEJMra1406184 (2015).
Kantarjian, H. et al. Intensive chemotherapy does not benefit most older patients (age 70 years or older) with acute myeloid leukemia. Blood 116, 4422–4429. https://doi.org/10.1182/blood-2010-03-276485 (2010).
Li, W. et al. Controlling nutritional status (CONUT) score is a prognostic factor in patients with resected breast cancer. Sci. Rep. 10, 6633. https://doi.org/10.1038/s41598-020-63610-7 (2020).
Zhao, Y. et al. The geriatric nutrition risk index versus the mini-nutritional assessment short form in predicting postoperative delirium and hospital length of stay among older non-cardiac surgical patients: a prospective cohort study. BMC Geriatr. 20, 107. https://doi.org/10.1186/s12877-020-1501-8 (2020).
Xiao, F. K., Wang, L., Zhang, W. C., Wang, L. D. & Zhao, L. S. Preoperative Prognostic Nutritional Index is a Significant Predictor of Survival in Esophageal Squamous Cell Carcinoma Patients. Nutr Cancer https://doi.org/10.1080/01635581.2020.1757129 (2020).
Acknowledgements
The authors thank all researchers in North Japan Hematology Study Group (NJHSG). We would like to thank Shinichi Fujisawa, Kaori Sato, Satoshi Oguri (Hokkaido University Hospital, Department of Laboratory and Transfusion) for sample analysis and all medical staff who provided dedicated care for the patients.
Author information
Authors and Affiliations
Contributions
H.Senjo and M.O. designed the study, analyzed data, and wrote the paper. S.Yokoyama and D.Hidaka analyzed gene mutations and managed data integrity. M.O. organized Hokkaido Leukemia Net and recruit patients. S.Yamamoto, Y.T., Y.H., T.N., A.M., S.O., H.Sakai, T.I., T.M., Y.K., M.K., H.K., and H.I. performed recruitment and treatment of patients. D.Hashimoto, T.K. and T.T. supervised the study and gave approve to final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Senjo, H., Onozawa, M., Hidaka, D. et al. A novel nutritional index “simplified CONUT” and the disease risk index independently stratify prognosis of elderly patients with acute myeloid leukemia. Sci Rep 10, 19400 (2020). https://doi.org/10.1038/s41598-020-76250-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76250-8
This article is cited by
-
High CRP-albumin ratio predicts poor prognosis in transplant ineligible elderly patients with newly diagnosed acute myeloid leukemia
Scientific Reports (2022)
-
Utility of a modified Controlling Nutritional Status score in mortality risk assessment of patients on hemodialysis
International Urology and Nephrology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.