Abstract
Purpose
Ureaplasma species are associated with urogenital infections, infertility and adverse pregnancy outcomes as well as neonatal infections. Involvement of the central nervous system in adults is extremely rare. We report an unusual case of a brain abscess secondary to otitis media with Ureaplasma parvum in a patient with granulomatosis with polyangiitis (GPA).
Methods
Imaging and laboratory findings, treatment decisions, and outcome of this case are explicated.
Results
A young adult with GPA presented with progredient earache after ambulant diagnosis of otitis media. Despite different courses of broad-spectrum antibiotic therapy, she developed meningoencephalitis due to mastoiditis following temporal abscess formation. Mastoidectomy and neurosurgical abscess removal were performed. Standard cultures of cerebrospinal fluid, blood and intracranial abscess material, as well as polymerase chain reaction (PCR) for common bacterial and viral meningitis pathogens remained negative. Only eubacterial PCR of intracranial abscess material returned positive for Ureaplasma parvum. The patient finally improved under antibiotic therapy with moxifloxacin and doxycycline.
Conclusion
Ureaplasma species are rare causative pathogens in immunocompromised patients. They should be considered in patients with humoral immunodeficiencies with culture-negative infections failing standard therapy. Eubacterial PCR should be performed in early states of infection in these patients for immediate diagnosis and initiation of appropriate treatment to prevent adverse outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case report
A 25-year-old female presented with progredient unilateral earache after ambulant diagnosis of otitis media and three days of treatment with amoxicillin (1 g three times daily). Due to a refractory status of granulomatosis with polyangiitis (GPA), she received a fourfold immunosuppression consisting of prednisolone (5 mg once daily), azathioprine (200 mg once daily), methotrexate (20 mg once weekly) and rituximab (500 mg every 6 months, last 5 months ago).
Otoscopy showed extensive inflammation of the external ear, without signs of mastoiditis. Two days after paracentesis and therapy adjustment to ampicillin/sulbactam (3 g three times daily), she presented with progredient headache, meningism and encephalopathy with aphasia.
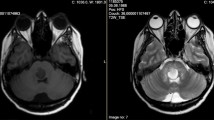
Cerebrospinal fluid (CSF) assessment showed lymphocytic pleocytosis (49 white blood cells/mm3). Cranial computed tomography (CT) indicated mastoiditis with slight bone destruction of the temporal lobe. Treatments with ceftriaxone (2 g twice daily), ampicillin (2 g six times daily) and acyclovir (750 mg three times daily) were started for acquired meningoencephalitis due to mastoiditis. Immunotherapy was stopped and mastoidectomy was performed immediately. Cultures of CSF and blood, as well as multiplex real-time polymerase chain reaction (PCR) for common bacterial meningitis pathogens (Haemophilus influenzae, Neisseria meningitidis, Streptococcus agalactiae, Streptococcus pneumoniae, Listeria monocytogenes and Escherichia coli), enzyme-linked immunosorbent assay (ELISA) for Borrelia burgdorferi and Treponema pallidum as well as PCR for common meningitis viruses (Cytomegalovirus, Epstein-Barr virus, Herpes simplex virus 1/2, Varicella-zoster virus and Enterovirus) remained negative. Histopathology showed a florid abscessing inflammation in the mastoid and chronic granulating inflammation in the ear canal. No granulomas were found. A postoperative magnetic resonance imaging (MRI) demonstrated a temporal meningoencephalitis without abscess formation (Fig. 1). Headache and aphasia improved postoperatively.
A Early cerebritis, axial fluid attenuated inversion recovery (FLAIR)-weighted MRI. B Early cerebritis, axial contrast-enhanced T1-weighted MRI. C Temporal abscess formation, axial fluid attenuated inversion recovery FLAIR-weighted MRI. D Temporal abscess formation, axial contrast-enhanced T1-weighted MRI. E Abscess relapse with herniation, axial FLAIR-weighted MRI. F Abscess relapse with herniation, axial contrast-enhanced T1-weighted MRI
On day 8 post mastoidectomy clinical conditions deteriorated. The patient presented with fever and reduced level of consciousness. An MRI scan identified a new temporal abscess formation, and neurosurgical abscess removal was performed. Due to insufficient improvement, antibiotic therapy was changed to ceftazidime (2 g three times daily), vancomycin (through levels of 15–20 mg/L) and metronidazole (500 mg three times daily).
Cultures of intracranial abscess material as well as PCR for Staphylococcus aureus remained negative, while eubacterial PCR of intracranial abscess material returned positive for Ureaplasma parvum (1/1 samples) on day 7 after intracranial abscess surgery (day 15 post mastoidectomy). By then, a new abscess had developed that required hemicraniectomy due to herniation. Real-time PCR confirmed U. parvum-DNA of secondary abscess material (2/2 samples).
Real-time PCR for Mycoplasma and Ureaplasma species confirmed U. parvum-DNA in 2/2 samples of secondary abscess material, while PCR for Mycoplasma genitalum and hominis as well as Ureaplasma urealyticum remained negative.
The patient improved under therapy with moxifloxacin (400 mg once daily) and doxycycline (200 mg loading dose, 100 mg twice daily). She was weaned from tracheostomy and percutaneous endoscopic gastrostomy. The intracranial abscess formation regressed. When transferred to rehabilitation after 10 weeks of in-patient treatment, she was fully awake and orientated, with moderate aphasia. Pr3-ANCA levels remained low, indicating a remission of GPA. Restart of immunosuppressants was deferred until significant increase of pr3ANCA levels.
No apparent signs of any genitourinary infections were apparent during the course of infection. PCR for Mycoplasma and Ureaplasma species remained negative in cervical smear. Noteworthy, urogenital examination was not performed until two weeks of calculated therapy with moxifloxacin and doxycycline.
Discussion
We report a rare case of intracranial abscess secondary to otitis media by U. parvum in an adult patient with granulomatosis with polyangiitis (GPA) and fourfold immunosuppression.
Ureaplasma species frequently colonize the genitourinary tract of asymptomatic women. Its presence is linked to urogenital infections, infertility and adverse pregnancy outcomes as well as neonatal infections. Extragenital infections in adults have been described to cause postoperative infections or invasive infections of immunocompromised hosts, predominantly with humoral immunodeficiencies [1].
Ureaplasma species frequently colonize the genitourinary tract of asymptomatic women. Its presence has been linked to urogenital infections, infertility and adverse pregnancy outcomes as well as neonatal infections [1]. Meningitis in newborns is usually associated with the transmission of Ureaplasma either in utero or perinatal [2]. Extragenital infections in adults are rare. They have been described to cause postoperative infections [3,4,5] or invasive infections of an immunocompromised host, predominantly with humoral immunodeficiencies [6]. Another risk factor are prosthetic implants [6].
Involvement of the central nervous system is extremely rare. Only few cases in adults have been described. Previous case reports mainly described ventriculitis and meningitis [7,8,9,10]. Recent reports are connected to neurosurgical complications in immunocompetent patients [8,9,10]. Another case of meningitis due to U. urealyticum has been reported in context of immunosuppression and kidney transplantation [7]. A superinfected hematoma, which developed after the explantation of the rejected kidney graft, has been suggested as focus of hematogenous spread.
In our case intracranial Ureaplasma infection presented with temporal abscess formation. To the best of our knowledge, only one case with intracranial abscess formation in adults with U. urealyticum has been described in a patient in remission of Burkitt’s lymphoma [11]. Although the rituximab-containing treatment was administered three years ago, hypogammaglobulinemia was still present in this patient. Hypogammaglobulinemia as a risk factor for Ureaplasma infections was as well descried in a patient with U. urealyticum meningitis and Good’s syndrome [12].
The point of entry for extragenital Ureaplasma infections mostly remains unclear. In the previously mentioned cases of postoperative Ureaplasma infections a hematogenous systemic spread from the genitourinary tract after insertion of a urinary catheter was proposed. After neurosurgery a perioperative contamination is suggestive but not proofed in previous reports [8, 9]. In our case we presume infection per continuitatem leading to the temporal abscess formation. In line with this, MRI scans suggested primary cerebritis in direct contact to the mastoid and showed unilateral leptomeningeal contrast enhancement. Interestingly no granulomas were found in pathological work-up of the mastoid.
Ureaplasma are fastidious bacteria that lack a cell-wall and are therefore intrinsically resistant to antibiotics that infer with cell wall synthesis like β-lactam or glycopeptides antibiotics. They do not grow on routine media or appear on gram stain. Therefore, diagnosis is challenging. A specialized culture or PCR assay must be employed. Our case report highlights the importance of eubacterial PCR in cultures without growth. Eubacterial PCR or alternative next-generation sequencing (NGS) should be performed early in immunocompromised patients to identify rare and elusive pathogens and prevent adverse outcomes due to delayed diagnosis. Until now NGS is not routinely applied in diagnostics, but recent research highlights its potential to identify multiple pathogenic microorganisms from one sample, advantageous especially in usually polymicrobial infections like brain abscesses [13, 14].
Conclusion
Ureaplasma parvum is a very rare causative pathogen responsible for invasive CNS infections in immunocompromised patients. Eubacterial PCR should be performed in early states of infection in these patients for immediate diagnosis and initiation of appropriate treatment to prevent adverse outcomes.
Ureaplasma species should be considered in patients with humoral immunodeficiencies with culture-negative infections failing standard therapy as well as in implant infections and postoperative cases.
Data availability statement
Anonymized data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Gwee A, Curtis N. Ureaplasma—Are you sitting comfortably? J Infect. 2014;68:19–23. https://doi.org/10.1016/j.jinf.2013.09.027.
Wang Q, Wang K, Zhang Y, et al. Neonatal Ureaplasma parvum meningitis: a case report and literature review. Transl Pediatr. 2020;9:174–9. https://doi.org/10.21037/tp.2020.02.04.
Lucke K, Kuster SP, Bertea M, Ruef C, Bloemberg GV. A deep sternal wound infection caused by Ureaplasma urealyticum. J Med Microbiol. 2010;59:1254–6. https://doi.org/10.1099/jmm.0.022814-0.
García-de-la-Fuente C, Miñambres E, Ugalde E, Sáez A, Martinez-Martinez L, Fariñas MC. Post-operative mediastinitis, pleuritis and pericarditis due to Mycoplasma hominis and Ureaplasma urealyticum with a fatal outcome. J Med Microbiol. 2008;57:656–7. https://doi.org/10.1099/jmm.0.47632-0.
Walkty A, Lo E, Manickam K, Alfa M, Xiao L, Waites K. Ureaplasma parvum as a cause of sternal wound infection. J Clin Microbiol. 2009;47:1976–8. https://doi.org/10.1128/JCM.01849-08.
Jhaveri VV, Lasalvia MT. Invasive Ureaplasma infection in patients receiving rituximab and other humoral immunodeficiencies—a case report and review of the literature. Open Forum Infect Dis. 2019;6:ofz399. https://doi.org/10.1093/ofid/ofz399.
Geissdörfer W, Sandner G, John S, Gessner A, Schoerner C, Schröppel K. Ureaplasma urealyticum meningitis in an adult patient. J Clin Microbiol. 2008;46:1141–3. https://doi.org/10.1128/JCM.01628-07.
Pailhoriès H, Chenouard R, Eveillard M, et al. A case of Ureaplasma parvum meningitis in an adult after transphenoidal ablation of craniopharyngioma. Int J Infect Dis. 2019;84:5–7. https://doi.org/10.1016/j.ijid.2019.04.024.
Saje A, Velnar T, Smrke B, et al. Ureaplasma parvum ventriculitis related to surgery and ventricular peritoneal drainage. J Infect Chemother. 2020;26:513–5. https://doi.org/10.1016/j.jiac.2019.12.017.
Xing N, Zhao Z, Li Q, et al. Ureaplasma parvum meningitis following atypical choroid plexus papilloma resection in an adult patient: a case report and literature review. BMC Infect Dis. 2021;21:1276. https://doi.org/10.1186/s12879-021-06975-y.
Deetjen P, Maurer C, Rank A, Berlis A, Schubert S, Hoffmann R. Brain abscess caused by Ureaplasma urealyticum in an adult patient. J Clin Microbiol. 2014;52:695–8. https://doi.org/10.1128/JCM.02990-13.
Zhang T, Li H, Hou S, et al. Case report of Ureaplasma urealyticum meningitis in a patient with thymoma and hypogammaglobulinaemia. BMC Infect Dis. 2021;21:1142. https://doi.org/10.1186/s12879-021-06831-z.
Hu HL, Guo LY, Wu HL, Feng WY, Chen TM, Liu G. Evaluation of next-generation sequencing for the pathogenic diagnosis of children brain abscesses. J Infect. 2019;78:323–37. https://doi.org/10.1016/j.jinf.2019.01.003.
Stebner A, Ensser A, Geißdörfer W, Bozhkov Y, Lang R. Molecular diagnosis of polymicrobial brain abscesses with 16S-rDNA-based next-generation sequencing. Clin Microbiol Infect. 2021;27:76–82. https://doi.org/10.1016/j.cmi.2020.03.028.
Acknowledgements
We would like to express our sincere gratitude toward all colleagues who cared for the patient.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the case report as well as analysis and interpretation of data. The first draft of the manuscript was written by Marie Madlener and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
M. Madlener has no relevant financial or non-financial interests to disclose. M. Breuninger has no relevant financial or non-financial interests to disclose. A. Meißner has no relevant financial or non-financial interests to disclose. H. Stetefeld has no relevant financial or non-financial interests to disclose. S. Telentschak has no relevant financial or non-financial interests to disclose. T. Wille has no relevant financial or non-financial interests to disclose. T. van Eimeren has no relevant financial or non-financial interests to disclose. N. Jung has received lecture fees from Gilead, Infectopharm, MSD, Bayer and Labor Stein and travel grants from Gilead, Basilea, Correvio, Pfizer and Novartis and grants from an observational study from Infectofos.
Ethical approval
This case report was conducted following the 1964 Declaration of Helsinki and its subsequent amendments.
Consent to publish
The participant has consented to the submission of the case report to the journal.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Madlener, M., Breuninger, M., Meißner, A. et al. Brain abscess with Ureaplasma parvum in a patient with granulomatosis with polyangiitis. Infection 51, 779–782 (2023). https://doi.org/10.1007/s15010-022-01966-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01966-w