Abstract
Background
Recent evidence confirmed that the maximum energy in metastatic breast cancer progression is supplied by fatty acid oxidation (FAO) governed by a rate-limiting enzyme, carnitine palmitoyltransferase 1 (CPT1). Therefore, the active limitation of FAO could be an emerging aspect to inhibit breast cancer progression. Herein, for the first time, we have introduced quercetin (QT) from a non-dietary source (Mikania micrantha Kunth) to limit the FAO in triple-negative breast cancer cells (TNBC) through an active targeting of CPT1.
Methods
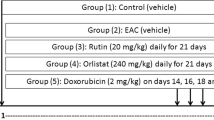
Molecular quantification of QT was confirmed through high-performance thin-layer chromatography (HPTLC). Computational docking analyses predicted the binding affinity of QT to CPT1. Cell-based seahorse energy efflux investigated the mitochondrial respiration rate, glycolytic function and ATP production rate. Real-time quantitative reverse transcription polymerase chain reaction (qRT-PCR) investigated the FAO-associated gene expression. Matrigel cell invasion and fluorescence-activated cell sorting analyses investigated anti-metastatic and apoptotic cell death induction activities, respectively. In vivo antitumor activities were checked using the female breast cancer mice (BALB/c) model.
Results
QT resulted in a significant reduction in the intracellular mitochondrial respiration and glycolytic function, limiting extensive ATP production. In turn, QT elevated the reactive oxygen species (ROS) and depleted antioxidant levels to induce anti-metastatic and cell apoptosis activities. qRT-PCR resulted in active healing of altered FAO-associated gene expression which was well predicted through the successful in silico molecular binding potentiality of QT to CPT1. Subsequently, QT has shown excellent in vivo antitumor activities through the altered lipid profile and oxidative stress-healing capabilities.
Conclusions
All the obtained data significantly grounded the fact that QT could be a promising metabolism-targeted breast cancer therapeutic.
Graphical abstract







Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- ACC:
-
Acetyl-CoA carboxylase
- AMPK:
-
Activated protein kinase
- ATP:
-
Adenosine triphosphate
- C/EBPα:
-
CCAAT-enhancer-binding protein a
- CPT1:
-
Carnitine palmitoyltransferase 1
- DCF:
-
Dichlorofluorescein
- DCFDA:
-
2′,7′-Dichlorofluorescein diacetate
- ELISA:
-
Enzyme-linked immunosorbent assay
- ER:
-
Estrogen receptor
- ETC:
-
Electron transport chain
- FAO:
-
Fatty acid oxidation
- FASN:
-
Fatty acid synthase
- FFA:
-
Free fatty acid
- HBSS:
-
Hanks’ balanced salt solution
- HER-2:
-
Human epidermal growth factor receptor 2
- LCFA:
-
Long chain fatty acid
- MMP:
-
Matrix metalloproteinase
- PPARγ:
-
Peroxisome proliferator-activated receptor-gamma
- PR:
-
Progesterone receptor
- qRT-PCR:
-
Real-time quantitative reverse transcription polymerase chain reaction
- QT:
-
Quercetin
- TCA:
-
Tricarboxylic acid
- TMB:
-
3,3′,5,5′-Tetramethylbenzidine
- TNBC:
-
Triple-negative breast cancer
- XP:
-
Extra-precision
References
Anders CK, Abramson V, Tan T, Dent R. The evolution of triple-negative breast cancer: from biology to novel therapeutics. Am Soc Clin Oncol Educ Book. 2016;35:34–42.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
The cancer genome atlas network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70.
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (er)-negative, progesterone receptor (pr)-negative, and her2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer registry. Cancer. 2007;109:1721–8.
Koundouros N, Poulogiannis G. Reprogramming of fatty acid metabolism in cancer. Br J Cancer. 2020;122:4–22.
Ma Y, Temkin SM, Hawkridge AM, Guo C, Wang W, Wang XY, Fang X. Fatty acid oxidation: an emerging facet of metabolic transformation in cancer. Cancer Lett. 2018;435:92–100.
Monaco ME. Fatty acid metabolism in breast cancer subtypes. Oncotarget. 2017;8:29487–500.
Nomura DK, Long JZ, Niessen S, Hoover HS, Ng SW, Cravatt BF. Monoacylglycerol lipase regulates a fatty acid network that promotes cancer pathogenesis. Cell. 2010;140:49–61.
Warburg O, Wind F, Negelein E. The metabolism of tumors in the body. J Gen Physiol. 1927;8:519–30.
Porporato PE, Filigheddu N, Pedro JNVS, Kroemer G, Galluzzi L. Mitochondrial metabolism and cancer. Cell Res. 2018;28:265–80.
Wang T, Fahrmann JF, Lee HY, Li J, Tripathi SC, Yue C, Zhang C, Lifshitz V, Song J, Yuan Y, Somlo G, Jandial R, Ann D, Hanash S, Jove R, Yu H. JAK/STAT3-regulated fatty acid b-oxidation is critical for breast cancer stem cell self-renewal and chemoresistance. Cell Metab. 2018;27:136-150e5.
Carracedo A, Cantley LC, Pandolfi PP. Cancer metabolism: fatty acid oxidation in the limelight. Nat Rev Cancer. 2013;13:227–32.
Ferraro GB, Ali A, Luengo A, Kodack DP, Deik A, et al. Fatty acid synthesis is required for breast cancer brain metastasis. Nat Cancer. 2021;2:414–28.
Camarda R, Zhou AY, Kohnz RA, Balakrishnan S, Mahieu C, Anderton B, Eyob H, Kajimura S, Tward A, Krings G, Nomura DK, Goga A. Inhibition of fatty acid oxidation as a therapy for MYC-overexpressing triple-negative breast cancer. Nat Med. 2016;22:427–32.
Qu Q, Zeng F, Liu X, Wang QJ, Deng F. Fatty acid oxidation and carnitine palmitoyltransferase I: emerging therapeutic targets in cancer. Cell Death Dis. 2016;7: e2226.
Hunt DA, Lane HM, Zygmont ME, Dervan PA, Hennigar RA. mRNA stability and over expression of fatty acid synthase in human breast cancer cell lines. Anticancer Res. 2007;27:27–34.
Chajes V, Cambot M, Moreau K, Lenoir GM, Joulin V. Acetyl-coA carboxylase α is essential to breast cancer cell survival. Cancer Res. 2006;66(10):5287–94.
Yao C-H, Liu G-Y, Wang R, Moon SH, Gross RW, Patti GJ. Identifying off-target effects of etomoxir reveals that carnitine palmitoyltransferase I is essential for cancer cell proliferation independent of beta-oxidation. PLoS Biol. 2018;16(3): e2003782.
Galluzzi L, Kepp O, Vander Heiden MG, Kroemer G. Metabolic targets for cancer therapy. Nat Rev Drug Discov. 2013;12(11):829–46.
Ashraf MA. Phytochemicals as potential anticancer drugs: time to ponder nature’s bounty. BioMed Res Int. 2020;2020:8602879.
Guerra AR, Maria F, Duarte MF, Duarte IF. Targeting tumor metabolism with plant-derived natural products: emerging trends in cancer therapy. J Agric Food Chem. 2018;66:10663–85.
Koh YC, Ho CT, Pan MH. Recent advances in cancer chemoprevention with phytochemicals. J Food Drug Anal. 2020;28:14–37.
Sheam MM, Haque Z, Nain Z. Towards the antimicrobial, therapeutic and invasive properties of Mikania micrantha Kunth: a brief overview. J Adv Biotechnol Exp Ther. 2020;3:92–101.
Tabaczar S, Pieniążek A, Czepas J, PiaseckaZelga J, Gwoździński K, Koceva-Chyła A. Quercetin attenuates oxidative stress in the blood plasma of rats bearing DMBA-induced mammary cancer and treated with a combination of doxorubicin and docetaxel. Gen Physiol Biophys. 2013;32:535–43.
Ali H, Dixit S. Quercetin attenuates the development of 7, 12-dimethyl benz (a) anthracene (DMBA) and croton oil-induced skin cancer in mice. J Biomed Res. 2015;29:139–44.
Ahn J, Lee H, Kim S, Park J, Ha T. The anti-obesity effect of quercetin is mediated by the AMPK and MAPK signaling pathways. Biochem Biophys Res Commun. 2008;373:545–9.
Brusselmans K, Vrolix R, Verhoeven G, Swinnen JV. Induction of cancer cell apoptosis by flavonoids is associated with their ability to inhibit fatty acid synthase activity. J Biol Chem. 2005;280:5636–45.
Zhang M, Xie Z, Gao W, Pu L, Wei J, Gao C. Quercetin regulates hepatic cholesterol metabolism by promoting cholesterol-to-bile acid conversion and cholesterol efflux in rats. Nutr Res. 2016;36:271–9.
Kim Y, Kim CS, Joe Y, Chung HT, Ha TY, Yu R. Quercetin reduces tumor necrosis factor alpha-induced muscle atrophy by upregulation of heme oxygenase-1. J Med Food. 2018;21(6):551–9.
Sultan AS, Khalil MIM, Sami BM, Alkhuriji AF, Sadek O. Quercetin induces apoptosis in triple-negative breast cancer cells via inhibiting fatty acid synthase and beta-catenin. Int J Clin Exp Pathol. 2017;10:156–72.
Ruidas B, Sur TK, Pal K, Som Chaudhury S, Prasad P, Sinha K, Sarkar PK, Das P, Das MC. Herbometallic nano-drug inducing metastatic growth inhibition in breast cancer through intracellular energy depletion. Mol Biol Rep. 2020;47:3745–63.
Yang J, Yan R, Roy A, Xu D, Poisson J, Zhang Y. The I-TASSER suite: protein structure and function prediction. Nat Methods. 2015;12:7–8.
Salentin S, Schreiber S, Haupt VJ, Adasme MF, Schroeder M. PLIP: fully automated protein-ligand interaction profiler. Nucleic Acids Res. 2015;43:W443–7.
Ruidas B, Som Chaudhury S, Pal K, Sarkar PK, Das MC. A novel herbometallic nanodrug has the potential for antibacterial and anticancer activity through oxidative damage. Nanomedicine. 2019;14:1173–89.
Srinivasan A, Thangavel C, Liu Y, Shoyele S, Den RB, Selvakumar P, Lakshmikuttyamma A. Quercetin regulates b-catenin signaling and reduces the migration of triple negative breast cancer. Mol Carcinog. 2016;55:743–56.
Llaverias G, Danilo C, Mercier I, Daumer K, Capozza F, Williams TM, Sotgia F, Lisanti MP, Frank PG. Role of cholesterol in the development and progression of breast cancer. Am J Pathol. 2011;178:402–12.
Montesdeoca N, Lopez M, Ariza X, Herrero L, Makowski K. Inhibitors of lipogenic enzymes as a potential therapy against cancer. FASEB J. 2020;34:11355–81.
Anand David AV, Arulmoli R, Parasuraman S. Overviews of biological importance of quercetin: a bioactive flavonoid. Pharmacogn Rev. 2016;10:84–9.
Srivastava S, Somasagara R, Hegde M, Nishana M, Tadi SK, Srivastava M, Choudhary B, Raghavan SC. Quercetin, a natural flavonoid interacts with dna, arrests cell cycle and causes tumor regression by activating mitochondrial pathway of apoptosis. Sci Rep. 2016;6:24049.
Reyes-Farias M, Carrasco-Pozo C. The anti-cancer effect of qt: molecular implications in cancer metabolism. Int J Mol Sci. 2019;20:3177.
Acknowledgements
We thank Dr. Sib Sankar Roy (Senior scientist, CSIR-IICB, West Bengal, India) for helping us in cell-based seahorse energy efflux experimentations.
Funding
This work was not supported by any grant from funding agencies.
Author information
Authors and Affiliations
Contributions
Conceptualization and design of study: BR. Experimentation, data acquisition and analysis: BR, TKS, KS, PS, SSC, SB, RM. Drafting manuscript: BR. Critical revision of the manuscript: CDM, AS. Study supervision: BR. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed involving animals were in accordance with the NIH guidelines and institutional animal ethical committee approval (RKC/IAEC/A/03 dated 14/12/17) for laboratory animals at R.G. Kar Medical College, Kolkata, India.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ruidas, B., Sur, T.K., Das Mukhopadhyay, C. et al. Quercetin: a silent retarder of fatty acid oxidation in breast cancer metastasis through steering of mitochondrial CPT1. Breast Cancer 29, 748–760 (2022). https://doi.org/10.1007/s12282-022-01356-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01356-y