Abstract
Purpose
Osteoporotic vertebral fracture (OVF) with nonunion or neurological deficit may be a candidate for surgical treatment. However, some patients do not show improvement as expected. Therefore, we conducted a nationwide multicenter study to determine the predictors for postoperative poor activity of daily living (ADL) in patients with OVF.
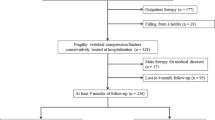
Methods
We retrospectively reviewed the case histories of 309 patients with OVF who underwent surgery. To determine the factors predicting postoperative poor ADL, uni- and multivariate statistical analyses were performed.
Results
The frequency of poor ADL at final follow-up period was 9.1%. In univariate analysis, preoperative neurological deficit (OR, 4.1; 95% CI, 1.8–10.3; P < 0.001), perioperative complication (OR, 3.4; P = 0.006), absence of preoperative bone-modifying agent (BMA) administration (OR, 2.7; P = 0.03), and absence of postoperative recombinant human parathyroid hormone (rPTH) administration (OR, 3.9; P = 0.006) were significantly associated. In multivariate analysis, preoperative neurological deficit (OR, 4.6; P < 0.001), perioperative complication (OR, 3.4; P = 0.01), and absence of postoperative rPTH administration (OR, 3.9; P = 0.02) showed statistical significance.
Conclusions
Preoperative neurological deficit, perioperative complication, and absence of postoperative rPTH administration were considered as predictors for postoperative poor ADL in patients with OVF. Neurological deficits and complications are often inevitable factors; therefore, rPTH is an important option for postoperative treatment for OVF.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
Steel H (1951) Kümmell’s disease. Am J Surg 81:161–167
Cauley JA, Hochberg MC, Lui L-Y et al (2007) Long-term risk of incident vertebral fractures. JAMA 298:2761–2767
Cummings SR, Black DM, Rubin SM (1989) Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med 149:2445–2448
Suzuki N, Ogikubo O, Hansson T (2008) The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months. Eur Spine J 17:1380–1390
Itoi E, Sakurai M, Mizunashi K et al (1990) Long-term observations of vertebral fractures in spinal osteoporotics. Calcif Tissue Int 47:202–208
Hasegawa K, Homma T, Uchiyama S et al (1998) Vertebral pseudarthrosis in the osteoporotic spine. Spine 23:2201–2206
Kanchiku T, Imajo Y, Suzuki H et al (2014) Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech 27:E61–E65
Omi H, Yokoyama T, Ono A et al (2014) Can MRI predict subsequent pseudarthrosis resulting from osteoporotic thoracolumbar vertebral fractures? Eur Spine J 23:2705–2710
Sugita M, Watanabe N, Mikami Y et al (2005) Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech 18:376–381
Ho SC, Lau EM, Woo J et al (1999) The prevalence of osteoporosis in the Hong Kong Chinese female population. Maturitas 32:171–178
Lee YL, Yip KM (1996) The osteoporotic spine. Clin Orthop Relat Res 323:91–97
Kaneda K, Taneichi H, Abumi K et al (1997) Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am 79:69–83
Ataka H, Tanno T, Yamazaki M (2009) Posterior instrumented fusion without neural decompression for incomplete neurological deficits following vertebral collapse in the osteoporotic thoracolumbar spine. Eur Spine J 18:69–76
Suk S-I, Kim J-H, Lee S-M et al (2003) Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine 28:2170–2175
Nguyen H-V, Ludwig S, Gelb D (2003) Osteoporotic vertebral burst fractures with neurologic compromise. J Spinal Disord Tech 16:10–19
Kashii M, Yamazaki R, Yamashita T et al (2013) Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures—anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J 22:1633–1642
Ito Y, Oda H, Taguchi T, Inoue H, Kawai S (2003) Results of surgical treatment for lumbar canal stenosis due to degenerative spondylolisthesis: enlargement of the lumbar spinal canal. J Orthop Sci 8:648–656
Hirabayashi K, Miyakawa J, Satomi K et al (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 6:354–364
Matsumoto T, Hoshino M, Tsujio T et al (2012) Prognostic factors for reduction of activities of daily living following osteoporotic vertebral fractures. Spine 37:1115–1121
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Ito Y, Hasegawa Y, Toda K et al (2002) Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J 2:101–106
Kanayama M, Ishida T, Hashimoto T et al (2010) Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse. J Spinal Disord Tech 23:53–56
Uchida K, Nakajima H, Yayama T et al (2010) Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine 13:612–621
Sudo H, Ito M, Kaneda K et al (2013) Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J 13:1726–1732
Ito M, Harada A, Nakano T et al (2010) Retrospective multicenter study of surgical treatments for osteoporotic vertebral fractures. J Orthop Sci 15:289–293
Kashii M, Yamazaki R, Yamashita T et al (2015) Factors affecting postoperative activities of daily living in patients with osteoporotic vertebral collapse with neurological deficits. J Bone Miner Metab 33:422–431
Nakashima H, Imagama S, Yukawa Y et al (2015) Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine 40:E120–E126
Yasuda T, Kawaguchi Y, Suzuki K et al (2017) Five-year follow up results of posterior decompression and fixation surgery for delayed neural disorder associated with osteoporotic vertebral fracture. Medicine (Baltimore) 96:e9395
Kashii M, Yamazaki R, Yamashita T et al (2013) Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures—anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J 22:1633–1642
Ciol MA, Deyo RA, Howell E et al (1996) An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc 44:285–290
Nakashima H, Imagama S, Yukawa Y et al (2015) Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine 40:E120–E126
Lyles KW, Colón-Emeric CS, Magaziner JS et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Santini D, Martini F, Fratto ME et al (2009) In vivo effects of zoledronic acid on peripheral gammadelta T lymphocytes in early breast cancer patients. Cancer Immunol Immunother 58:31–38
Carbone LD, Warrington KJ, Barrow KD et al (2006) Pamidronate infusion in patients with systemic sclerosis results in changes in blood mononuclear cell cytokine profiles. Clin Exp Immunol 146:371–380
Colón-Emeric CS, Mesenbrink P, Lyles KW et al (2010) Potential mediators of the mortality reduction with zoledronic acid after hip fracture. J Bone Miner Res 25:91–97
Neer RM, Arnaud CD, Zanchetta JR et al (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Compston JE (2007) Skeletal actions of intermittent parathyroid hormone: effects on bone remodelling and structure. Bone 40:1447–1452
Dempster DW, Cosman F, Kurland ES et al (2001) Effects of daily treatment with parathyroid hormone on bone microarchitecture and turnover in patients with osteoporosis: a paired biopsy study. J Bone Miner Res 16:1846–1853
Panico A, Lupoli GA, Marciello F, et al (2011) Teriparatide vs. alendronate as a treatment for osteoporosis: changes in biochemical markers of bone turnover, BMD and quality of life. Med Sci Monit 17:CR442-448
Ohtori S, Inoue G, Orita S et al (2012) Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine 37:E1464–E1468
Ohtori S, Inoue G, Orita S et al (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 38:E487–E492
Ebata S, Takahashi J, Hasegawa T et al (2017) Role of weekly teriparatide administration in osseous union enhancement within six months after posterior or transforaminal lumbar interbody fusion for osteoporosis-associated lumbar degenerative disorders: a multicenter, prospective randomized study. J Bone Joint Surg Am 99:365–372
Acknowledgements
The authors are indebted to the medical editors from the Department of International Medical Communications of Tokyo Medical University for editing and reviewing the initial English manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related directly or indirectly to this study.
Ethical approval
This study was approved by the Ethics Review Committee of all institute involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Murata, K., Matsuoka, Y., Nishimura, H. et al. The factors related to the poor ADL in the patients with osteoporotic vertebral fracture after instrumentation surgery. Eur Spine J 29, 1597–1605 (2020). https://doi.org/10.1007/s00586-019-06092-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06092-0