Abstract
Purpose
The COVID-19 pandemic resulted in increased penetrating trauma and decreased length of stay (LOS) amongst the adult trauma population, findings important for resource allocation. Studies regarding the pediatric trauma population are sparse and mostly single-center. This multicenter study examined pediatric trauma patients, hypothesizing increased penetrating trauma and decreased LOS after the 3/19/2020 stay-at-home (SAH) orders.
Methods
A multicenter retrospective analysis of trauma patients ≤ 17 years old presenting to 11 centers in California was performed. Demographic data, injury characteristics, and outcomes were collected. Patients were divided into three groups based on injury date: 3/19/2019–6/30/2019 (CONTROL), 1/1/2020–3/18/2020 (PRE), 3/19/2020–6/30/2020 (POST). POST was compared to PRE and CONTROL in separate analyses.
Results
1677 patients were identified across all time periods (CONTROL: 631, PRE: 479, POST: 567). POST penetrating trauma rates were not significantly different compared to both PRE (11.3 vs. 9.0%, p = 0.219) and CONTROL (11.3 vs. 8.2%, p = 0.075), respectively. POST had a shorter mean LOS compared to PRE (2.4 vs. 3.3 days, p = 0.002) and CONTROL (2.4 vs. 3.4 days, p = 0.002). POST was also not significantly different than either group regarding intensive care unit (ICU) LOS, ventilator days, and mortality (all p > 0.05).
Conclusions
This multicenter retrospective study demonstrated no difference in penetrating trauma rates among pediatric patients after SAH orders but did identify a shorter LOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic resulted in stay-at-home (SAH) orders and other mandates designed to slow the spread of disease [1,2,3]. These restrictions also triggered business closures, economic losses, and psychological stressors that have significantly impacted society [4,5,6,7,8,9,10,11]. These changes have been particularly detrimental to children who have also been impacted by school closures and social isolation [12,13,14,15,16]. Therefore, injury patterns and outcomes within the pediatric trauma population had the potential to change during the pandemic.
Significant shifts within the adult trauma population during COVID-19 are now well described and include an increase in penetrating trauma and drug use, variations in trauma volume based on insurance status, and a shorter length of stay (LOS) [17,18,19,20,21,22,23,24,25,26]. However, studies dedicated to the pediatric trauma population are sparse and have been mostly single-center in design [27,28,29,30,31,32,33,34]. One of these studies demonstrated a similar increase in pediatric penetrating trauma, as has been seen with adult trauma, during the COVID-19 pandemic [27]. Another study reporting that child-involved shooting incidents increased in 2020 during the COVID-19 pandemic also supports the possibility that penetrating trauma rates are increasing in the pediatric population [35].
Therefore, we sought to explore the changes in mechanisms and outcomes among the pediatric trauma population during the COVID-19 pandemic in a multicenter study, as these could affect resource allocation in the future. We hypothesized an increase in penetrating trauma rates and a shorter LOS in the Southern California pediatric trauma population after the March 19, 2020 SAH orders [36].
Methods
A post hoc analysis of pediatric trauma patients presenting to 11 American College of Surgeons (ACS) Level I and II trauma centers in Southern California between 1/1/2020–6/30/2020 and 3/19/2019–6/30/2019 was performed. These 11 centers span 7 counties in Southern California and comprise a mixture of academic and private hospitals that serve mostly urban areas. The study was approved by the Institutional Review Board (IRB) of University of California, Irvine and all participating centers and was deemed exempt from need for consent.
All patients ≤ 17 years old who were either a trauma activation or trauma consult were included in this study. The primary outcome was the rate of penetrating trauma, categorized as either gunshot wounds, stab wounds, or other. The secondary outcome was LOS. Other outcomes were intensive care unit (ICU) admission, ICU LOS, ventilator days, operations performed (tracheostomy, laparotomy, craniectomy/craniotomy, and vascular/endovascular surgery), and mortality. Demographic data were collected which included sex (self-reported), age, race, insurance status (i.e., Medicaid, private, and uninsured), and body mass index (BMI). Other mechanisms of injury recorded included motor vehicle collisions (MVC), pedestrian struck, motorcycle collision (MCC), sports injuries, ground level falls (GLF), falls from height, and assaults. Injury severity score (ISS), serum alcohol positivity, and urine toxicology were also recorded. Vital signs and exam findings on arrival were also collected and included heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), and Glasgow Coma Scale (GCS) score. Discharge disposition was collected and included home, long-term acute care hospital (LTAC), and acute rehabilitation.
Patients were then divided into three groups based on the date of injury: a historical control from 3/19/2019–6/30/2019 (CONTROL), immediately before the SAH order from 1/1/2020–3/18/2020 (PRE), and after the SAH order 3/19/2020–6/30/2020 (POST). Descriptive statistics were performed for all variables within each group, with categorical variables reported as percentages of their respective group and continuous variables as means with standard deviations. The POST group was compared to the PRE group and the CONTROL group in two separate analyses. This was done to account for both seasonal and annual variations that exist within the trauma population. Additionally, different subgroups including patients 12 years and older, younger than 12 years old, ISS greater than or equal to 10, and ISS less than 10 were created. LOS was compared between the three time periods for each subgroup. Chi-square tests were used to compare categorical variables and Mann–Whitney U tests for continuous variables. Next, multivariable logistic regression utilizing time period, age, race, insurance status, and ISS was performed to identify independent risk factors for a LOS longer than 2 days. The adjusted risk of LOS longer than 2 days was reported as an odds ratio (OR) with a 95% confidence interval (CI). p values < 0.05 were considered statistically significant. All analyses were performed using IBM SPSS Statistics for Windows (Version 24, IBM Corp., Armonk, NY).
Results
A total of 1677 trauma patients were identified across the 3 time periods: 631 patients in the CONTROL group, 479 in the PRE group, and 567 in the POST group.
PRE vs. POST demographics
Compared to the PRE group, the POST group had a higher percentage of white (42.0 vs. 35.9%, p = 0.045) and Black (9.3 vs. 5.8%, p = 0.035) patients, but a lower percentage of Latino patients (41.1 vs. 50.3%, p = 0.003). The POST group also had significantly higher rate of Medicaid (46.9 vs. 31.5%, p < 0.001), but lower rate of private insurance (43.0 vs. 56.6%, p < 0.001). Otherwise, the two groups were similar regarding sex, age, race, insurance status, and BMI (all p > 0.05) (Table 1).
CONTROL vs. POST demographics
Compared to the CONTROL group, the POST group had a higher rate of Medicaid (46.9 vs. 34.2%, p < 0.001), but lower rates of private insurance (43.0 vs. 57.4%, p < 0.001) and no insurance (3.9 vs. 6.5%, p = 0.043). The POST group also had a higher mean BMI (21.3 vs. 20.1 kg/m2, p = 0.006). Otherwise, the two groups were similar regarding sex, age, and race (all p > 0.05) (Table 1).
PRE vs. POST injury characteristics, toxicology, and vital signs
Compared to the PRE group, the POST group had a similar rate of penetrating trauma (11.3 vs. 9.0%, p = 0.219) including both gunshot and stab wounds individually (both p > 0.05), but a lower rate of MVC (21.2 vs. 27.3%, p = 0.020). Otherwise, the groups were similar in terms of mechanism of injury, alcohol/drug positivity, ISS, and vital signs on arrival (all p > 0.05) (Table 2).
CONTROL vs. POST injury characteristics, toxicology, and vital signs
Compared to the CONTROL group, the POST group had a similar penetrating trauma rate (11.3 vs. 8.2%, p = 0.075) including both gunshot and stab wounds individually (both p > 0.05). However, the POST group had lower rates of pedestrians struck (6.7 vs. 10.3%, p = 0.027) and MCC (3.9 vs. 7.6%, p = 0.006). The POST group had a higher mean SBP (122.2 vs. 120.4 mmHg, p = 0.045) and HR (108.1 vs. 105.1 beats per minute, p = 0.010) on arrival. Otherwise, the two groups were similar with regards to mechanism of injury, alcohol/drug positivity, and vital signs on arrival (all p > 0.05) (Table 2).
PRE vs. POST Outcomes
Compared to the PRE group, the POST group had a shorter mean LOS (2.4 vs. 3.3 days, p = 0.002). The POST group also had higher rates of discharge to home (80.6 vs. 75.6%, p = 0.049), but lower rates of discharge to acute rehabilitation (1.8 vs. 3.8%, p = 0.047). Otherwise, the two groups were similar in terms of ICU admission, ICU LOS, ventilator days, operations, discharge disposition, and mortality (all p > 0.05) (Table 3).
CONTROL vs. POST Outcomes
Compared to the CONTROL group, the POST group had a shorter mean LOS (2.4 vs. 3.4 days, p = 0.002) and a lower rate of laparotomy (2.0 vs. 2.8%, p = 0.002). Otherwise, the two groups were similar in terms of ICU admission, ICU LOS, ventilator days, discharge disposition, and mortality (all p > 0.05) (Table 3).
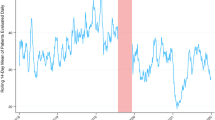
Mechanisms of injury of pediatric trauma patients by time period
In the POST group, there were 503 patients who sustained blunt and 64 who sustained penetrating injuries. In the PRE group, 436 sustained blunt and 43 sustained penetrating injuries. In the CONTROL group, 579 patients sustained blunt injuries and 52 sustained penetrating injuries (Fig. 1).
Length of stay for different pediatric trauma subgroups compared by time period
Among patients 12 years and older, mean LOS was significantly shorter in the POST group compared to both the PRE and CONTROL groups, respectively (2.5 vs 3.5 days, p = 0.026) (2.5 vs 3.5 days, p = 0.032). In patients younger than 12 years, LOS was similarly shorter in the POST group (2.2 vs 3.1 days, p = 0.022) (2.2 vs 3.2 days, p = 0.003). Among patients with an ISS greater than or equal to 10, mean LOS was significantly shorter in the POST group compared to both the PRE and CONTROL groups, respectively (4.5 vs 7.8 days, p = 0.004) (4.5 vs 8.9 days, p < 0.001). In patients with an ISS less than 10, LOS of the POST group was not significantly different than that of the other two time periods (p > 0.05) (Table 4).
Multivariable logistic regression analysis for risk of LOS longer than 2 days in pediatric trauma patients
On multivariable logistic regression analysis, an ISS greater than 15 was an independent associated risk factor for LOS longer than 2 days (OR = 4.99, CI 3.42–7.29, p < 0.001). Presenting during the POST period was associated with a decreased risk of having a LOS longer than 2 days (OR = 0.66, CI 0.54–0.82, p = < 0.001) (Table 5).
Discussion
There are few studies detailing the effects the COVID-19 pandemic has had on pediatric trauma mechanisms and outcomes. This retrospective multicenter study across Southern California found no difference in penetrating trauma rates after SAH orders including analyses on gunshot and stab wounds specifically. However, there was a shorter mean LOS in the POST cohort compared to both the PRE and CONTROL groups. There were no differences between cohorts in terms of other parameters such as drug and alcohol positivity and insurance status.
A rise in community violence during COVID-19 has resulted in a parallel increase in penetrating trauma rates among adults, but has not definitively affected the pediatric trauma population [37,38,39,40]. This current multicenter study found a slightly higher although statistically similar penetrating trauma rate among pediatric patients before and after SAH orders. Though some of our other findings, including a decrease in MVC, MCC, and pedestrians struck, are similar to that of prior studies, our findings regarding penetrating trauma oppose those reported by Sherman et al. who found an increase in penetrating trauma among pediatric patients during COVID-19 [27]. However, Sherman et al.’s study had a number of limitations including the inclusion of 18- and 19-year-old patients and the classification of animal bites (which comprised 42% of penetrating trauma in the study) as penetrating trauma which has different trauma and societal implications. Moreover, only a single comparison was made to the mean of the prior 4 years, which does not take into account there may have been a pre-existing annual trend for increased penetrating trauma prior to the pandemic. In contrast, our study compares the COVID-19 data to the year prior, as well as the time frame immediately preceding the pandemic to account for this potential confounder. Furthermore, findings of this multicenter study suggest that the pediatric trauma population was affected differently than the adult population by COVID-19 and SAH orders. This could be due to different pandemic-related stressors and children being less affected by the violence that has risen in the community. These findings could be useful to pediatric trauma centers when planning for future pandemics, as they could improve resource allocation.
Predicting LOS in pediatric trauma patients is important for resource management, especially during a pandemic [41]. This study identified a 1 day shorter mean LOS during the COVID-19 pandemic, compared to both the time period immediately prior and a historical control. Furthermore, we were also able to show that presenting during the COVID-19 pandemic was associated with a decreased risk of having a hospital stay longer than 2 days, even after controlling for other risk factors of prolonged length of stay. These findings are similar to that of two prior studies identifying a decreased LOS during COVID, though one included only adults and the other included both adult and pediatric trauma patients [7, 24]. To our knowledge, this study is the first to confirm these findings solely in a pediatric trauma population. The shorter LOS could be due to providers discharging patients earlier to conserve resources during a pandemic [42, 43]. These findings could also potentially indicate that LOS during non-pandemic times is unnecessarily long, though further prospective studies collecting readmission data are needed to confirm this.
There are a number of limitations to this study. First, this was a multicenter study that utilized multiple trauma registries and data collectors, which could have resulted in misclassification and missing variables. Second, this study does not include every trauma center in the region, making the subset of pediatric patients in this study not fully representative of the entire trauma population in Southern California. Additionally, the centers included in this study were not children’s hospitals. Third, as this was a post hoc analysis with no prior power analysis, our lack of statistical significance could be due to a lack of power, although the population size was larger than the previous study which found a significant difference in penetrating trauma, but notably included animal bites. Next, we did not collect variables that would allow us to track changes in non-accidental trauma, which significantly increased in other studies, limiting us from fully exploring all the effects of COVID-19 on the pediatric trauma population [29, 33]. Finally, COVID-19-related restrictions persisted for many months following our study period, suggesting this manuscript data may not fully represent all potential changes surrounding the COVID-19 pandemic.
Conclusion
This multicenter retrospective study in Southern California demonstrated similar penetrating trauma rates among pediatric trauma patients after SAH orders. However, the mean LOS was 1 day shorter compared to both the PRE and CONTROL cohorts. These findings may help trauma providers anticipate needs and allocate resources during future pandemics. In addition, future studies should be performed to evaluate if pediatric trauma LOS can be safely decreased during non-pandemic patient care.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J et al (2019) A novel coronavirus from patients with pneumonia in China. N Engl J Med 382(8):727–733. https://doi.org/10.1056/NEJMoa2001017
Castillo RC, Staguhn ED, Weston-Farber E (2020) The effect of state-level stay-at-home orders on COVID-19 infection rates. Am J Infect Control 48(8):958–960. https://doi.org/10.1016/j.ajic.2020.05.017
Borjas GJ (2020) Business closures, stay-at-home restrictions, and COVID-19 testing outcomes in New York City. Prev Chronic Dis 17:E109. https://doi.org/10.5888/pcd17.200264
Jacobsen GD, Jacobsen KH (2020) Statewide COVID-19 stay-at-home orders and population mobility in the United States. World Med Health Policy. https://doi.org/10.1002/wmh3.350 (Epub 2020 July 29)
Gostin LO, Wiley LF (2020) Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA 323(21):2137–2138. https://doi.org/10.1001/jama.2020.5460
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C et al (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg 78:185–193. https://doi.org/10.1016/j.ijsu.2020.04.018
Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L et al (2020) Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 277:55–64. https://doi.org/10.1016/j.jad.2020.08.001
Rajkumar RP (2020) COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 52:102066. https://doi.org/10.1016/j.ajp.2020.102066
Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, Wang X (2021) Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord 281:91–98. https://doi.org/10.1016/j.jad.2020.11.117
Gloster AT, Lamnisos D, Lubenko J, Presti G, Squatrito V, Constantinou M et al (2020) Impact of COVID-19 pandemic on mental health: an international study. PLoS ONE 15(12):e0244809. https://doi.org/10.1371/journal.pone.0244809
Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M (2020) The psychological impact of COVID-19 on the mental health in the general population. QJM 113(8):531–537. https://doi.org/10.1093/qjmed/hcaa201
Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E (2020) Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health 17(22):8479. https://doi.org/10.3390/ijerph17228479
Zhu S, Zhuang Y, Ip P (2021) Impacts on children and adolescents’ lifestyle, social support and their association with negative impacts of the COVID-19 pandemic. Int J Environ Res Public Health 18(9):4780. https://doi.org/10.3390/ijerph18094780
Tso WWY, Wong RS, Tung KTS, Rao N, Fu KW, Yam JCS et al (2020) Vulnerability and resilience in children during the COVID-19 pandemic. Eur Child Adolesc Psychiatry 17:1–16. https://doi.org/10.1007/s00787-020-01680-8
Marques de Miranda D, da Silva AB, Sena Oliveira AC, Simoes-E-Silva AC (2020) How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct 51:101845. https://doi.org/10.1016/j.ijdrr.2020.101845
Varma P, Junge M, Meaklim H, Jackson ML (2020) Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry 109:110236. https://doi.org/10.1016/j.pnpbp.2020.110236
Yeates EO, Grigorian A, Barrios C, Schellenberg M, Owattanapanich N, Barmparas G et al (2021) Changes in traumatic mechanisms of injury in Southern California related to COVID-19: penetrating trauma as a second pandemic. J Trauma Acute Care Surg 90(4):714–721. https://doi.org/10.1097/TA.0000000000003068
Ghafil C, Matsushima K, Ding L, Henry R, Inaba K (2021) Trends in trauma admissions during the COVID-19 pandemic in Los Angeles County, California. JAMA Netw Open 4(2):e211320. https://doi.org/10.1001/jamanetworkopen.2021.1320
Berg GM, Wyse RJ, Morse JL, Chipko J, Garland JM, Slivinski A et al (2021) Decreased adult trauma admission volumes and changing injury patterns during the COVID-19 pandemic at 85 trauma centers in a multistate healthcare system. Trauma Surg Acute Care Open 6(1):e000642. https://doi.org/10.1136/tsaco-2020-000642
Chodos M, Sarani B, Sparks A, Bruns B, Gupta S, Michetti CP et al (2021) Impact of COVID-19 pandemic on injury prevalence and pattern in the Washington, DC Metropolitan Region: a multicenter study by the American College of Surgeons Committee on Trauma, Washington, DC. Trauma Surg Acute Care Open 6:e000659. https://doi.org/10.1136/tsaco-2020-000659
Sherman WF, Khadra HS, Kale NN, Wu VJ, Gladden PB, Lee OC (2021) How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res 479(2):266–275. https://doi.org/10.1097/CORR.0000000000001484
Olding J, Zisman S, Olding C, Fan K (2021) Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon 19(1):e9–e13. https://doi.org/10.1016/j.surge.2020.07.004
Rhodes HX, Petersen K, Biswas S (2020) Trauma trends during the initial peak of the COVID-19 pandemic in the midst of lockdown: experiences from a rural trauma center. Cureus 12(8):e9811. https://doi.org/10.7759/cureus.9811
Leichtle SW, Rodas EB, Procter L, Bennett J, Schrader R, Aboutanos MB (2020) The influence of a statewide “Stay-at-Home” order on trauma volume and patterns at a level 1 trauma center in the United States. Injury 51(11):2437–2441. https://doi.org/10.1016/j.injury.2020.08.014
Young KN, Yeates EO, Grigorian A, Schellenberg M, Owattanapanich N, Barmparas G et al (2021) Drug and alcohol positivity of trauma patients related to COVID-19 stay-at-home orders. Am J Drug Alcohol Abuse 4:1–7. https://doi.org/10.1080/00952990.2021.1904967
Yeates EO, Juillard C, Grigorian A, Schellenberg M, Owattanapanich N, Barmparas G et al (2021) The coronavirus disease 2019 (COVID-19) stay-at-home order’s unequal effects on trauma volume by insurance status in Southern California. Surgery. https://doi.org/10.1016/j.surg.2021.02.060
Sanford EL, Zagory J, Blackwell JM, Szmuk P, Ryan M, Ambardekar A (2021) Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg 56(5):918–922. https://doi.org/10.1016/j.jpedsurg.2021.01.020
Sheridan GA, Nagle M, Russell S, Varghese S, O’Loughlin PF, Boran S et al (2020) Pediatric trauma and the COVID-19 pandemic: a 12-year comparison in a level-1 trauma center. HSS J 16(Suppl 1):1–5. https://doi.org/10.1007/s11420-020-09807-y
Kovler ML, Ziegfeld S, Ryan LM, Goldstein MA, Gardner R, Garcia AV et al (2020) Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl 116:104756. https://doi.org/10.1016/j.chiabu.2020.104756
Keays G, Friedman D, Gagnon I (2020) Injuries in the time of COVID-19. Health Promot Chronic Dis Prev Can 40(11–12):336–341. https://doi.org/10.24095/hpcdp.40.11/12.02
Bram JT, Johnson MA, Magee LC, Mehta NN, Fazal FZ, Baldwin KD et al (2020) Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop 40(8):373–379. https://doi.org/10.1097/BPO.0000000000001600
Hernigou J, Morel X, Callewier A, Bath O, Hernigou P (2020) Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int Orthop 44(8):1473–1480. https://doi.org/10.1007/s00264-020-04619-5
Sidpra J, Abomeli D, Hameed B, Baker J, Mankad K (2021) Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch Dis Child 106(3):e14. https://doi.org/10.1136/archdischild-2020-319872
Raitio A, Ahonen M, Jääskelä M, Jalkanen J, Luoto TT, Haara M et al (2021) Reduced number of pediatric orthopedic trauma requiring operative treatment during COVID-19 restrictions: a nationwide cohort study. Scand J Surg 110(2):254–257. https://doi.org/10.1177/1457496920968014
Donnelly M, Grigorian A, Swentek L, Arora J, Kuza CM, Inaba K et al (2021) Firearm violence against children in the United States. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000003347. Published online July 1, 2021
COVID19.CA.GOV. Latest news on COVID-19. https://covid19.ca.gov/latest-news. Updated May 25, 2021. Accessed May 25, 2021
Sutherland M, McKenney M, Elkbuli A (2021) Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med 39:225–226. https://doi.org/10.1016/j.ajem.2020.05.006
Abdallah HO, Zhao C, Kaufman E, Hatchimonji J, Swendiman RA, Kaplan LJ et al (2021) Increased firearm injury during the COVID-19 pandemic: a hidden urban burden. J Am Coll Surg 232(2):159–168. https://doi.org/10.1016/j.jamcollsurg.2020.09.028
Kim DY, Phillips SW (2021) When COVID-19 and guns meet: a rise in shootings. J Crim Justice 73:101783. https://doi.org/10.1016/j.jcrimjus.2021.101783
Qasim Z, Sjoholm LO, Volgraf J, Sailes S, Nance ML, Perks DH et al (2020) Trauma center activity and surge response during the early phase of the COVID-19 pandemic-the Philadelphia story. J Trauma Acute Care Surg 89(4):821–828. https://doi.org/10.1097/TA.0000000000002859
Gibbs D, Ehwerhemuepha L, Moreno T, Guner Y, Yu P, Schomberg J et al (2020) Prolonged hospital length of stay in pediatric trauma: a model for targeted interventions. Pediatr Res Epub. https://doi.org/10.1038/s41390-020-01237-0
Bornstein E, Gulersen M, Husk G, Grunebaum A, Blitz MJ, Rafael TJ et al (2020) Early postpartum discharge during the COVID-19 pandemic. J Perinat Med 48(9):1008–1012. https://doi.org/10.1515/jpm-2020-0337
Greene NH, Kilpatrick SJ, Wong MS, Ozimek JA, Naqvi M (2020) Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM 2(4):100234. https://doi.org/10.1016/j.ajogmf.2020.100234
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EOY, AG, NO, GB, KG, LP-V, AL, RAF, TC, KBS, GD, AJ, JC, AN, AL, and CG. The first draft of the manuscript was written by EOY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Compliance with ethical standards
This study was approved by the Institutional Review Board (IRB) of University of California, Irvine and all participating centers and was deemed exempt from need for consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yeates, E.O., Grigorian, A., Schellenberg, M. et al. Effects of the COVID-19 pandemic on pediatric trauma in Southern California. Pediatr Surg Int 38, 307–315 (2022). https://doi.org/10.1007/s00383-021-05050-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-05050-6