Abstract
Recently, progression-free survival at 24 months (PFS24) was defined as clinically relevant for patients with extranodal NK/T cell lymphoma. Herein, the clinical data from two independent random cohorts (696 patients each in the primary and validation datasets) were used to develop and validate a risk index for PFS24 (PFS24-RI), and evaluate its ability to predict early progression. Patients achieving PFS24 had a 5-year overall survival (OS) of 95.8%, whereas OS was only 21.2% in those failing PFS24 (P<0.001). PFS24 was an important predictor of subsequent OS, independent of risk stratification. The proportion of patients achieving PFS24 and 5-year OS rates correlated linearly among risk-stratified groups. Based on multivariate analysis of the primary dataset, the PFS24-RI included five risk factors: stage II or III/IV, elevated lactate dehydrogenase, Eastern Cooperative Oncology Group score ≥2, primary tumor invasion, and extra-upper aerodigestive tract. PFS24-RI stratified the patients into low-risk (0), intermediate-risk (1–2), high-risk (≥3) groups with different prognoses. Harrell’s C-index of PFS24-RI for PFS24 prediction was 0.667 in the validation dataset, indicating a good discriminative ability. PFS24-RI calibration indicated that the actual observed and predicted probability of failing PFS24 agreed well. PFS24-RI provided the probability of achieving PFS24 at an individual patient level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extranodal natural killer/T cell lymphoma (ENKTCL) is a rare, heterogeneous, and aggressive disease that shows a geographical and racial preference for East Asian and South American populations [1,2,3]. It predominantly originates in the upper aerodigestive tract (UADT), particularly the nasal cavity and Waldeyer’s ring [4, 5], and manifests as a localized disease with marked primary tumor invasion (PTI) [6,7,8].
Over the past decade, outcomes for patients with ENKTCL have improved because of the widespread application of upfront radiotherapy and modern chemotherapy regimens [9,10,11,12,13,14,15,16]. Five-year overall survival (OS) is 60–90% for localized disease and 20–40% for disseminated disease. However, about 10–30% of patients with early-stage disease and >50% of patients with advanced-stage disease will experience disease progression or relapse after treatment, with extremely poor survival outcomes [17,18,19]. Approximately 80% of disease progression or death occurs within 24 months after initial treatment [19]. The annual hazard rates of death and failure were highest in the first 24 months, but decreased to <5% from 36 months onward [19, 20]. Thus, we urgently require the tools for the early identification of progression in patients with ENKTCL. PFS at 24 months (PFS24) represents a logical cutoff time point to further evaluate treatment outcome and risk prediction for patients with ENKTCL.
Recently, we demonstrated that PFS24 is an early endpoint to evaluate disease-related outcomes in patients with ENKTCL [19]. Those who achieve PFS24 have a similar survival rate to the sex- and age-matched general population. By contrast, patients who have an early disease progression within the first 24 months have very poor outcomes [19]. Therefore, PFS24 is a promising endpoint to develop a risk model in patients with ENKTCL. In contrast to previously established prognostic models, such as the nomogram-revised risk index (NRI) and prognostic index of natural killer lymphoma (PINK), which use time-to-event endpoints [8, 21, 22], the dichotomous nature of the PFS24 endpoint permits the prediction of individual risk, and allows better modeling of the risk of disease related outcomes in a setting in which most patients are cured by first-line current treatment [23].
This present study aimed to determine the effect of PFS24 on OS. We developed a visual nomogram for individualized risk estimate of PFS24, constructed a personalized risk model for the endpoint PFS24, and carried out independent validation of its performance.
Subjects and methods
The study population and eligibility
From the China Lymphoma Collaborative Group (CLCG) database, we retrospectively reviewed patients with newly diagnosed ENKTCL from 2008 to 2016. Patients enrolled in this study received modern treatment strategies comprising non-anthracycline-based chemotherapy regimens and/or radiotherapy [14,15,16, 24]. Exclusion criteria for the study consisted of patients who received palliative treatment, anthracycline-based chemotherapy, or unknown chemotherapy regimens. A total of 1392 patients were included in this study. The study received ethical approval from the institutional review boards. The patient data were de-identified, precluding the requirement for informed patient consent.
Of 1315 patients with the primary site of UADT, most patients received radiotherapy with (n = 931; 70.8%) or without (n = 247; 18.8%) chemotherapy, whereas 137 (10.4%) patients received chemotherapy alone.
Dataset grouping
The Ann Arbor staging system was used to stage the patients, and NRI and PINK were used for stratification [21, 22]. We evaluated the effect of PFS24 status on subsequent OS in all patients. To develop a risk index for PFS24 (PFS24-RI) and validate it independently, patients were randomly assigned to the primary dataset (n = 696) or the validation dataset (n = 696) in a 1:1 ratio using a stratified random sampling method.
Statistical methods
PFS represented the time between treatment and initial disease progression, relapse, or any cause death. PFS24 meant that at 24 months after initial treatment, the patient was alive and had shown no disease progression or relapse. OS was defined as the time from treatment to any death from any cause. Subsequent OS after the risk-defining event was defined as the time from achieving PFS24 or time since progression in those patients who failed to achieve PFS24 to death from any cause. The Kaplan–Meier method was used to estimate the survival rates, which were compared using a log-rank test.
In the primary dataset, the independent clinical characteristics for PFS24 were determined using univariate and multivariate regression models. The validation dataset was used to assess the final model by measuring both discrimination and calibration. Model discrimination was evaluated using receiver operating characteristic curves and Harrell’s C-index. The integrated Brier score (IBS, a measure of the forecasting accuracy for probabilistic predictions) and a calibration curve were used determine the consistency between the nomogram-predicted survival probability and the actual observed outcome. Regression analysis was used to assess whether a linear relationship existed between PFS24 and OS. The Pearson correlation coefficient, r, was used to estimate the correlation in the weighted linear regression, which was weighted according to the number of patients. Analyses were conducted using IBM SPSS Statistics, version 27.0 (IBM Corp., Armonk, NY, USA, and the rms, hmisc, and survival packages in the R software version 4.0.5 (http://www.r-project.org). P < 0.05 (two-tailed) represented a statistically significant difference.
Results
Characteristics of the patients and their survival
Table 1 summarizes the patients’ baseline clinical characteristics. Their median age was 43 years old; and the ratio of males to females was 2.25:1. Most patients had a good performance status (PS) according to the Eastern Cooperative Oncology Group (ECOG) score 0–1 (95.2%), primary disease in the UADT (94.5%), and early-stage disease (90.2%). Lactate dehydrogenase (LDH) was elevated in 25.4% of the patients. Most of the patients were classified as low to intermediate-high risk based on NRI (85.0%) or low risk based on PINK (80.3%).
With a median follow-up of 53 months, 369 of 1392 patients (26.5%) developed early progression within 24 months (failing PFS24), whereas 1023 patients (73.5%) showed no progression (achieving PFS24); 295 patients (21.2%) died. In all patients, the 5-year PFS and OS rates were 66.9% and 77.7%; in early-stage patients, they were 70.2% and 80.3%; and in advanced-stage patients, they were 35.6% and 50.9%, respectively.
Effect of PFS24 status on subsequent OS
We first assessed the impact of PFS24 status on long-term survival in all patients. The subsequent 5-year OS rate was 95.8% (95% confidence interval (CI): 94.3–97.3) for patients achieving PFS24, which was significantly higher than the 21.2% (95% CI: 16.8–26.9; P < 0.001) for those failing PFS24 (Fig. 1). After disease progression within the first 24 months, the median OS was only 5.1 (95% CI: 4.1–6.2) months.
PFS24 as a predictor for subsequent OS independent of risk stratification
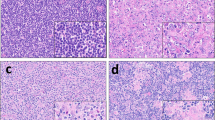
The impact of PFS24 status on subsequent OS in different risk groups was evaluated (Fig. 2). For patients achieving PFS24, the subsequent 5-year OS rate ranged from 92.8 to 94.7% across all risk groups stratified by NRI (Fig. 2A), and from 87.4 to 94.8% for all risk groups stratified by PINK (Fig. 2B). In contrast, for patients failing PFS24, the median OS was only 3 to 9.5 months for NRI-defined risk groups (Fig. 2C), and 4.7 to 5.5 months for PINK-defined risk groups (Fig. 2D). Patients achieving PFS24 had a very favorable prognosis, whereas patients failing PFS24 had a poor prognosis, regardless of the risk groups stratified using the NRI or PINK models.
PFS24 as a predictor for subsequent OS, independent of risk-stratified groups, using prognostic models. Subsequent OS for patients achieving PFS24 in risk groups stratified by NRI (A) and PINK (B) models, and for patients failing PFS24 in risk groups stratified by NRI (C) and PINK (D) models. PFS24, progression-free survival at 24 months; OS, overall survival; NRI, nomogram-revised risk index; PINK, prognostic index of natural killer lymphoma
Correlation between the proportion of patients achieving PFS24 and OS in the risk-stratified groups
The proportion of patients who achieved PFS24 were 85.7%, 76.0%, 72.4%, 59.9%, and 48.3% in low-, intermediate-low-, intermediate-high-, high-, and very-high-risk groups stratified using NRI, respectively, with the corresponding 5-year OS rates of 86.8%, 80.8%, 78.1%, 65.1%, and 51.4%. Similarly, the proportion of patients achieving PFS24 were 77.0%, 71.2%, and 42.3% for low-, intermediate-, and high-risk groups stratified using PINK, respectively, with corresponding 5-year OS rates of 80.7%, 74.3%, and 50.2%, respectively. A significant linear correlation between the proportion of patients achieving PFS24 and 5-year OS rates was observed among different NRI-defined or PINK-defined risk groups (both r = 1, Fig. 3). These findings indicated that achieving PFS24 after first-line therapy is an important goal to obtain favorable long-term survival for an individual patient.
Correlation between the proportion of patients achieving PFS24 and the 5-year OS rate in different risk groups stratified by the NRI (A) and PINK (B) models. PFS24, progression-free survival at 24 months; OS, overall survival; NRI, nomogram-revised risk index; PINK, prognostic index of natural killer lymphoma
Model development for PFS24-RI
We then developed a personalized risk model for PFS24. In the univariate analysis of the primary cohort, the risk factors associated with increased risk of disease progression before 24 months included extra-UADT (HR 3.34; 95% CI 1.78–6.32), regional lymph node involvement (HR 1.73; 95% CI 1.22–2.44), distant lymph node involvement (HR 3.55; 95% CI 1.82–7.02), presence of PTI (HR 1.67; 95% CI 1.18–2.37), elevated LDH (HR 1.99; 95% CI 1.37–2.89), ECOG score ≥2 (HR 2.95; 95% CI 1.44–6.07), and stage II (HR 1.70; 95% CI 1.15–2.49) or III–IV disease (HR 5.04; 95% CI 3.04–8.41; Supplemental Table 1). Multivariate analyses revealed that the stage, PTI, primary site, LDH, and ECOG score were independent risk factors for PFS24 (Table 2).
The multivariate analysis results were then used to develop an easy and visual prognostic nomogram to predict PFS24 (Fig. 4). Based on the corresponding regression coefficients, we then developed a PFS24-RI for the PFS24 endpoint in the primary dataset. The hazard ratio (HR) of the risk factors for PFS24 ranged between 1.4 and 2, with the exception of stage III/IV (HR = 3.31; Table 2). Consequently, we weighted the PFS24-RI components as follows: 1 point each for the risk factors extra-UADT; ECOG score ≥2; elevated LDH, PTI, or stage II; and 2 points for stage III/IV disease. Patients were stratified into the three groups based on the summed risk factor score: low risk (0), intermediate risk (1–2), and high risk (≥3).
Nomogram predicting the probability of failing to reach PFS24 for patients with ENKTCL. Each covariable value corresponds to a "Points" score shown in the top line of the nomogram. The sum of the points, which is identified in the line "Total Points" shows the sum of the points, which is translated to predict the probability of failing PFS24. PFS24, progression-free survival at 24 months; ENKTCL, extranodal NK/T-cell lymphoma; ECOG, Eastern Cooperative Oncology Group; PS, performance status; LDH, lactate dehydrogenase; PTI, primary tumor invasion; UADT, upper aerodigestive tract
Survival outcomes in risk groups stratified by PFS24-RI
In the whole population in the primary dataset, stratification using the PFS24-RI categories classified 195 (28.0%) patients as low risk, 371 (53.3%) as intermediate risk, and 130 (18.7%) as high risk. In the validation dataset, PFS24-RI classified 188 (27.0%) patients as low risk, 387 (55.6%) as intermediate risk, and 121 (17.4%) as high risk. PFS24-RI identified a small proportion of patients at low-risk, whereas it identified that a large proportion of them were at intermediate or high risk of disease progression and death.
Based on the PFS24-RI, the 5-year OS and PFS rates in three risk categories (low, intermediate, and high) were 87.7% (95% CI: 84.2–91.4) and 82.8% (95% CI: 87.0–89.0), 78.4% (95% CI: 75.4–81.6) and 66.4% (95% CI: 61.1–72.1), and 59.1% (95% CI: 52.8–66.1) and 45.3% (95% CI: 36.955.5) in the primary dataset (P < 0.001; Fig. 5A, B). The results were verified in the validation dataset, with 5-year OS and PFS rates of 87.0% (95% CI: 81.9–92.5) and 78.8% (95% CI: 72.3–85.9) in the low-risk group, 78.7% (95% CI: 74.5–83.1) and 67.3% (95% CI: 62.4–72.6) in the intermediate-risk group, and 62.9% (95% CI: 54.4–72.6) and 45.4% (95% CI: 36.3–56.7) in the high-risk group (P < 0.001; Fig. 6C, D). These results demonstrated that patients stratified by the PFS24-RI were associated with significantly different survival outcomes.
Survival curves of different risk groups based on PFS24-RI. OS (A) and PFS (B) of high, intermediate, and low-risk groups stratified according to PFS24-RI in the primary cohort. OS (C) and PFS (D) of high, intermediate, and low-risk groups stratified according to PFS24-RI in the validation dataset. PFS24, progression-free survival at 24 months; PFS24-RI, risk-index for progression-free survival at 24 months; OS, overall survival; PFS, progression-free survival
Validation and predictive accuracy of PFS24-RI for OS
Using the validation dataset, computing the bootstrap C statistic and a calibration plot were used to independently validate PFS24-RI. The C-index of PFS24-RI for the prediction of PFS24 was 0.664 in the primary dataset and 0.667 in the validation dataset, indicating that PFS24-RI had a good discriminative ability. According to the calibration curve, PFS24-RI was well calibrated, with an IBS of 0.178 in the primary dataset and 0.185 in the validation dataset. For the probability of failing PFS24, the actual observed and PFS24-RI predicted results agreed well (Fig. 6).
Discussion
Herein, we developed a PFS24-based risk model (PFS24-RI) to predict early disease progression in patients with ENKTCL under a current treatment strategy. A large multicenter cohort of patients was selected from the CLCG database to verify the PFS24 status as an indicator of prognosis of subsequent OS. Patients achieving PFS24 after initial therapy had favorable long-term outcomes, whereas patients failing PFS24 had poor prognosis, independent of risk groups stratified by the NRI or PINK models. Furthermore, extra-UADT, ECOG score ≥2, PTI, elevated LDH, and stage II or III–IV disease were identified as risk factors of failing PFS24, thus forming the PFS24-RI model. Based on PFS24-RI, patients could be categorized into low-, intermediate-, and high-risk groups with different prognoses. This model is useful to distinguish ENKTCL patients with different risks with disparate likelihoods of early progression or death. These results provide supplementary accuracy to the continual early estimation of prognosis after initial treatment, providing the rationale for surveillance strategies, and will help to guide prospective clinical trial designs for patients with ENKTCL.
In this study, using data from the CLCG database, we showed a similar frequency of early progression to that observed in previous studies [14, 17,18,19]. Among 1392 patients with ENKTCL, around a quarter (26.5%) experienced disease progression within 24 months after current treatment. PFS24 since initial therapy was associated with a significantly increased risk of death. There was a strong linear correlation between the proportion of patients achieving PFS24 and long-term OS among different risk groups stratified by NRI or PINK. Previously, we showed that prolonged OS is associated with improved PFS [25], and that survival time increased, the probability of survival increased, and the risks of failure and death decreased in early-stage ENKTCL [20]. Initially, the estimated risk of disease progression and mortality was high; however, they decreased markedly within the first 24 months after current treatment for ENKTCL [19, 20]. Patients who remained progression-free within 24 months after initial treatment had favorable long-term outcomes, with OS rates that were indistinguishable from those of age-, sex-, and country-matched populations [19]. In the present study, despite the heterogeneous prognoses for the NRI or PINK risk-stratified groups, all patients achieving PFS24 after initial treatment attained an equivalent favorable survival probability (~90%), independent of their initial risk category; however, patients failing PFS24 had extremely poor survival probability (median, ~6 months). Consistently, early progression within 24 months after initial therapy allowed stratification of subsequent OS and identified a high-risk population among patients with B cell lymphomas [26,27,28,29,30].
Optimization of risk stratification for early endpoints such as PFS24 and event-free survival at 24 months (EFS24) are crucial to facilitate prognosis and treatment decisions regarding lymphomas [27, 31, 32]. Here, we proposed that the novel PFS24-RI model, which integrated the established clinical risk factors to predict the PFS24 endpoint, will be useful in the upfront identification of high-risk patients with ENKTCL. The five variables, including stage, LDH, PS, primary site, and PTI, in the PFS24-RI are all well-established clinical predictors of survival outcome, and reflect the tumor load, invasive potential, and ability to tolerate treatment in patients with ENKTCL. LDH, stage, PS, and PTI remain from the NRI model [21], and primary site and stage are from the PINK model [22]. PFS24-RI provided a useful tool to advise patients for personalized risk prediction of early progression and has implications for enhancing patient stratification strategies in prospective clinical trial design. Patients at intermediate and high risk of disease progression within 24 months may benefit from escalated treatment or maintenance therapy.
Patient age is the most common indicator of continuous time-to-event outcomes, such as OS, in ENKTCL and other lymphomas [21, 33,34,35]. Consistently, elderly patients with ENKTCL had generally poor prognoses [36, 37]. However, older age (> 60 years old) was not identified as an independent risk factor in the PFS24-RI model. Our previous study demonstrated that elderly patients with low-risk early-stage disease or those with high-risk early-stage disease who achieve PFS24 after radiotherapy have similar survival to that of the sex- and age-matched general population [38]. These results suggested that, in contrast to the time-to-event endpoint of OS, PFS24 is less influenced by age and focuses more on disease events. Optimal treatment for ENKTCL should depend on disease-related risk factors rather than chronological age [37, 38]. Thus, PFS24-RI could generate predictions across a variety of ages as a disease-specific endpoint and could help to formulate more appropriate treatment strategies.
In this study, PFS24-RI clearly showed that patients with primary extra-UADT sites were at high risk of early progression. Previous studies demonstrated that a higher proportion of patients with extra-UADT ENKTCL had a risk of advanced-stage disease, elevated LDH, and poorer outcome compared with those with UADT ENKTCL [3, 4, 21, 22]. The reported 3-year OS and PFS rates were 43.6% and 27.9%, retrospectively [39]. This finding indicated that patients with extra-UADT ENKTCL were at increased risk of early progression and presented more aggressive clinical behavior.
This study included several strengths and limitations. Previous research highlighted more explicitly the importance of initial prognosis and treatment in patients with ENKTCL by using PINK and NRI at diagnosis [21, 22]. These previous models were constructed based on proportional hazards regression of time-to-event endpoints often, such as PFS or OS at 3 or 5 years, and assumed a constant risk of covariate implicitly. These models categorized patients into different risk groups according to outcomes provided by a survival curve; therefore, at specific time points, the predicted outcomes can vary markedly depending on clinical features of patients with ENKTCL in the original dataset. Thus, although a patient with ENKTCL can be classified as low risk or high risk, it is difficult to council patients on their individual risks for disease-specific outcomes. PFS24 has clinical relevance and could be adopted as a clinical study endpoint/early endpoint in a prognostic model of early progression prediction in ENKTCL. In this study, variables for potential inclusion in the PFS24-RI model were restricted to standard clinical variables that would be routinely available to physicians. This was a limitation of the model; however, the clinical variables included in the model have long history of clinical relevance in ENKTCL and are thus unlikely to be false associations. Although PFS24-RI is a personalized risk model to predict poor biological behavior, the precise mechanisms underlying early progression remain undefined. Assessment of tumor genetic features or including tumor biomarkers would be likely to add predictive information for patients with ENKTCL [40]. Further studies are needed to determine the effect of asparaginase-based regimens on PFS24 and OS, and assess the role of salvage treatments such as hematopoietic stem cell transplantation and immunotherapy for relapsed or refractory disease.
In conclusion, we demonstrated that PFS24 was an important predictor for OS, independent of NRI- or PINK-stratified risk groups. The PFS24-RI model provided the probability of achieving PFS24 at the level of the individual patient and could be applied for prospective study design and risk stratification.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBO, Berti E, Bhagat G, Borges AM, Boyer D, Calaminici M, Chadburn A, Chan JKC, Cheuk W, Chng WJ, Choi JK, Chuang SS, Coupland SE, Czader M, Dave SS et al (2022) The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia 36(7):1720–1748. https://doi.org/10.1038/s41375-022-01620-2
Sun J, Yang Q, Lu Z, He M, Gao L, Zhu M, Sun L, Wei L, Li M, Liu C, Zheng J, Liu W, Li G, Chen J (2012) Distribution of lymphoid neoplasms in China: analysis of 4,638 cases according to the World Health Organization classification. Am J Clin Pathol 138(3):429–434. https://doi.org/10.1309/ajcp7yltqpusdq5c
Au WY, Weisenburger DD, Intragumtornchai T, Nakamura S, Kim WS, Sng I, Vose J, Armitage JO, Liang R (2009) Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood 113(17):3931–3937. https://doi.org/10.1182/blood-2008-10-185256
Liu QF, Wang WH, Wang SL, Liu YP, Huang WT, Lu N, Zhou LQ, Ouyang H, Jin J, Li YX (2014) Immunophenotypic and clinical differences between the nasal and extranasal subtypes of upper aerodigestive tract natural killer/T-cell lymphoma. Int J Radiat Oncol Biol Phys 88(4):806–813. https://doi.org/10.1016/j.ijrobp.2013.12.005
Li YX, Liu QF, Fang H, Qi SN, Wang H, Wang WH, Song YW, Lu J, Jin J, Wang SL, Liu YP, Lu N, Liu XF, Yu ZH (2009) Variable clinical presentations of nasal and Waldeyer ring natural killer/T-cell lymphoma. Clin Cancer Res 15(8):2905–2912. https://doi.org/10.1158/1078-0432.CCR-08-2914
Wu RY, Liu K, Wang WH, Jin J, Song YW, Wang SL, Liu YP, Ren H, Fang H, Liu QF, Yang Y, Chen B, Qi SN, Lu NN, Tang Y, Tang Y, Li N, Ouyang H, Li YX (2017) Patterns of primary tumor invasion and regional lymph node spread based on magnetic resonance imaging in early-stage nasal NK/T-cell lymphoma: implications for clinical target volume definition and prognostic significance. Int J Radiat Oncol Biol Phys 97(1):50–59. https://doi.org/10.1016/j.ijrobp.2016.09.013
Qi SN, Xu LM, Yuan ZY, Wu T, Zhu SY, Shi M, Su H, Wang Y, He X, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Zhang YJ, Zhu Y, Cao JZ, Lan SM et al (2019) Effect of primary tumor invasion on treatment and survival in extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: a multicenter study from the China Lymphoma Collaborative Group (CLCG). Leuk Lymphoma 60(11):2669–2678. https://doi.org/10.1080/10428194.2019.1602265
Yang Y, Zhang YJ, Zhu Y, Cao JZ, Yuan ZY, Xu LM, Wu JX, Wang W, Wu T, Lu B, Zhu SY, Qian LT, Zhang FQ, Hou XR, Liu QF, Li YX (2015) Prognostic nomogram for overall survival in previously untreated patients with extranodal NK/T-cell lymphoma, nasal-type: a multicenter study. Leukemia 29(7):1571–1577. https://doi.org/10.1038/leu.2015.44
Yang Y, Zhu Y, Cao JZ, Zhang YJ, Xu LM, Yuan ZY, Wu JX, Wang W, Wu T, Lu B, Zhu SY, Qian LT, Zhang FQ, Hou XR, Li YX (2015) Risk-adapted therapy for early-stage extranodal nasal-type NK/T-cell lymphoma: analysis from a multicenter study. Blood 126(12):1424–1432; quiz 1517. https://doi.org/10.1182/blood-2015-04-639336
Yamaguchi M, Suzuki R, Oguchi M, Asano N, Amaki J, Akiba T, Maeda T, Itasaka S, Kubota N, Saito Y, Kobayashi Y, Itami J, Ueda K, Miyazaki K, Ii N, Tomita N, Sekiguchi N, Takizawa J, Saito B et al (2017) Treatments and outcomes of patients with extranodal natural killer/T-cell lymphoma diagnosed between 2000 and 2013: a cooperative study in Japan. J Clin Oncol 35(1):32–39. https://doi.org/10.1200/JCO.2016.68.1619
Kwong YL, Kim SJ, Tse E, Oh SY, Kwak JY, Eom HS, Do YR, Mun YC, Lee SR, Shin HJ, Suh C, Chuang SS, Lee YS, Lim ST, Izutsu K, Suzuki R, Relander T, d'Amore F, Schmitz N et al (2018) Sequential chemotherapy/radiotherapy was comparable with concurrent chemoradiotherapy for stage I/II NK/T-cell lymphoma. Ann Oncol 29(1):256–263. https://doi.org/10.1093/annonc/mdx684
Fox CP, Civallero M, Ko YH, Manni M, Skrypets T, Pileri S, Kim SJ, Cabrera ME, Shustov AR, Chiattone CS, Horwitz SM, Dlouhy I, Spina M, Hitz F, Montoto S, Nagler A, Martinez V, De Souza CA, Fernandez-Alvarez R et al (2020) Survival outcomes of patients with extranodal natural-killer T-cell lymphoma: a prospective cohort study from the international T-cell Project. Lancet Haematol 7(4):e284–e294. https://doi.org/10.1016/S2352-3026(19)30283-2
Vargo JA, Patel A, Glaser SM, Balasubramani GK, Farah RJ, Marks SM, Beriwal S (2017) The impact of the omission or inadequate dosing of radiotherapy in extranodal natural killer T-cell lymphoma, nasal type, in the United States. Cancer 123(16):3176–3185. https://doi.org/10.1002/cncr.30697
Qi SN, Yang Y, Zhang YJ, Huang HQ, Wang Y, He X, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Qiao XY, Wang H, Li GF, Zhu Y, Cao JZ, Wu JX, Wu T et al (2020) Risk-based, response-adapted therapy for early-stage extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: a China Lymphoma Collaborative Group study. Am J Hematol 95(9):1047–1056. https://doi.org/10.1002/ajh.25878
Qi SN, Yang Y, Song YQ, Wang Y, He X, Hu C, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Qiao XY, Wang H, Li GF, Huang HQ, Zhang YJ, Zhu Y, Cao JZ et al (2020) First-line non-anthracycline-based chemotherapy for extranodal nasal-type NK/T-cell lymphoma: a retrospective analysis from the CLCG. Blood Adv 4(13):3141–3153. https://doi.org/10.1182/bloodadvances.2020001852
Zheng X, He X, Yang Y, Liu X, Zhang LL, Qu BL, Zhong QZ, Qian LT, Hou XR, Qiao XY, Wang H, Zhu Y, Cao JZ, Wu JX, Wu T, Zhu SY, Shi M, Xu LM, Zhang HL et al (2021) Association of improved overall survival with decreased distant metastasis following asparaginase-based chemotherapy and radiotherapy for intermediate- and high-risk early-stage extranodal nasal-type NK/T-cell lymphoma: a CLCG study. ESMO Open 6(4):100206. https://doi.org/10.1016/j.esmoop.2021.100206
Yamaguchi M, Suzuki R, Kim SJ, Ko YH, Oguchi M, Asano N, Miyazaki K, Terui Y, Kubota N, Maeda T, Kobayashi Y, Amaki J, Soejima T, Saito B, Shimoda E, Fukuhara N, Tsukamoto N, Shimada K, Choi I et al (2018) Early disease progression in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Sci 109(6):2056–2062. https://doi.org/10.1111/cas.13597
Lim SH, Hong JY, Lim ST, Hong H, Arnoud J, Zhao W, Yoon DH, Tang T, Cho J, Park S, Ko YH, Kim SJ, Suh C, Lin T, Kim WS (2017) Beyond first-line non-anthracycline-based chemotherapy for extranodal NK/T-cell lymphoma: clinical outcome and current perspectives on salvage therapy for patients after first relapse and progression of disease. Ann Oncol 28(9):2199–2205. https://doi.org/10.1093/annonc/mdx316
Yang Y, Wang Y, Liu X, He X, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Qiao XY, Wang H, Li GF, Zhu Y, Cao JZ, Wu JX, Wu T, Zhu SY, Shi M et al (2021) Progression-free survival at 24 months and subsequent survival of patients with extranodal NK/T-cell lymphoma: a China Lymphoma Collaborative Group (CLCG) study. Leukemia 35(6):1671–1682. https://doi.org/10.1038/s41375-020-01042-y
Liu X, Wu T, Zhu SY, Shi M, Su H, Wang Y, He X, Xu LM, Yuan ZY, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Zhang YJ, Zhu Y, Cao JZ, Lan SM et al (2019) Risk-dependent conditional survival and failure hazard after radiotherapy for early-stage extranodal natural killer/T-cell lymphoma. JAMA Netw Open 2(3):e190194. https://doi.org/10.1001/jamanetworkopen.2019.0194
Chen SY, Yang Y, Qi SN, Wang Y, Hu C, He X, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Qiao XY, Wang H, Li GF, Zhang YJ, Zhu Y, Cao JZ, Lan SM et al (2021) Validation of nomogram-revised risk index and comparison with other models for extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: indication for prognostication and clinical decision-making. Leukemia 35(1):130–142. https://doi.org/10.1038/s41375-020-0791-3
Kim SJ, Yoon DH, Jaccard A, Chng WJ, Lim ST, Hong H, Park Y, Chang KM, Maeda Y, Ishida F, Shin DY, Kim JS, Jeong SH, Yang DH, Jo JC, Lee GW, Choi CW, Lee WS, Chen TY et al (2016) A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol 17(3):389–400. https://doi.org/10.1016/S1470-2045(15)00533-1
Liu X, Zhang LL, Qu BL, Zhong QZ, Qian LT, Yang Y, Hou XR, Qiao XY, Wang H, Zhu Y, Cao JZ, Wu JX, Wu T, Zhu SY, Shi M, Zhang HL, Zhang XM, Su H, Song YQ et al (2023) Evidence of cure for extranodal nasal-type natural killer/T-cell lymphoma with current treatment: an analysis of the CLCG database. Haematologica 23:2023. https://doi.org/10.3324/haematol.2022.281847
Qi SN, Li YX, Specht L, Oguchi M, Tsang R, Ng A, Suh CO, Ricardi U, Mac Manus M, Dabaja B, Yahalom J (2021) Modern radiation therapy for extranodal nasal-type NK/T-cell lymphoma: risk-adapted therapy, target volume, and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 110(4):1064–1081. https://doi.org/10.1016/j.ijrobp.2021.02.011
Yang Y, Cao JZ, Lan SM, Wu JX, Wu T, Zhu SY, Qian LT, Hou XR, Zhang FQ, Zhang YJ, Zhu Y, Xu LM, Yuan ZY, Qi SN, Li YX (2017) Association of improved locoregional control with prolonged survival in early-stage extranodal nasal-type natural killer/T-cell lymphoma. JAMA Oncol 3(1):83–91. https://doi.org/10.1001/jamaoncol.2016.5094
Zhu J, Yang Y, Tao J, Wang SL, Chen B, Dai JR, Hu C, Qi SN, Li YX (2020) Association of progression-free or event-free survival with overall survival in diffuse large B-cell lymphoma after immunochemotherapy: a systematic review. Leukemia 34(10):2576–2591. https://doi.org/10.1038/s41375-020-0963-1
Maurer MJ, Habermann TM, Shi Q, Schmitz N, Cunningham D, Pfreundschuh M, Seymour JF, Jaeger U, Haioun C, Tilly H, Ghesquieres H, Merli F, Ziepert M, Herbrecht R, Flament J, Fu T, Flowers CR, Coiffier B (2018) Progression-free survival at 24 months (PFS24) and subsequent outcome for patients with diffuse large B-cell lymphoma (DLBCL) enrolled on randomized clinical trials. Ann Oncol 29(8):1822–1827. https://doi.org/10.1093/annonc/mdy203
Casulo C, Byrtek M, Dawson KL, Zhou X, Farber CM, Flowers CR, Hainsworth JD, Maurer MJ, Cerhan JR, Link BK, Zelenetz AD, Friedberg JW (2015) Early relapse of follicular lymphoma after rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone defines patients at high risk for death: an analysis from the National LymphoCare Study. J Clin Oncol 33(23):2516–2522. https://doi.org/10.1200/JCO.2014.59.7534
Casulo C, Dixon JG, Le-Rademacher J, Hoster E, Hochster HS, Hiddemann W, Marcus R, Kimby E, Herold M, Sebban C, Gyan E, Foon K, Nielsen T, Vitolo U, Salles GA, Shi Q, Flowers CR (2022) Validation of POD24 as a robust early clinical end point of poor survival in FL from 5225 patients on 13 clinical trials. Blood 139(11):1684–1693. https://doi.org/10.1182/blood.2020010263
Luminari S, Merli M, Rattotti S, Tarantino V, Marcheselli L, Cavallo F, Varettoni M, Bianchi B, Merli F, Tedeschi A, Cabras G, Re F, Visco C, Torresan Delamain M, Cencini E, Spina M, Ferrero S, Ferrari A, Deodato M et al (2019) Early progression as a predictor of survival in marginal zone lymphomas: an analysis from the FIL-NF10 study. Blood 134(10):798–801. https://doi.org/10.1182/blood.2019001088
Jurinovic V, Kridel R, Staiger AM, Szczepanowski M, Horn H, Dreyling MH, Rosenwald A, Ott G, Klapper W, Zelenetz AD, Barr PM, Friedberg JW, Ansell S, Sehn LH, Connors JM, Gascoyne RD, Hiddemann W, Unterhalt M, Weinstock DM, Weigert O (2016) Clinicogenetic risk models predict early progression of follicular lymphoma after first-line immunochemotherapy. Blood 128(8):1112–1120. https://doi.org/10.1182/blood-2016-05-717355
Maurer MJ, Jais JP, Ghesquières H, Witzig TE, Hong F, Haioun C, Thompson CA, Thieblemont C, Micallef IN, Porrata LF, Ribrag V, Nowakowski GS, Casasnovas O, Bologna S, Morschhauser F, Morrison VA, Peterson BA, Macon WR, Copie-Bergman C et al (2016) Personalized risk prediction for event-free survival at 24 months in patients with diffuse large B-cell lymphoma. Am J Hematol 91(2):179–184. https://doi.org/10.1002/ajh.24223
International Non-Hodgkin’s Lymphoma Prognostic Factors Project (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329(14):987–994. https://doi.org/10.1056/NEJM199309303291402
Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, Morabito F, Martelli M, Brusamolino E, Iannitto E, Zaja F, Cortelazzo S, Rigacci L, Devizzi L, Todeschini G, Santini G, Brugiatelli M, Federico M (2004) Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood 103(7):2474–2479. https://doi.org/10.1182/blood-2003-09-3080
Federico M, Bellei M, Marcheselli L, Luminari S, Lopez-Guillermo A, Vitolo U, Pro B, Pileri S, Pulsoni A, Soubeyran P, Cortelazzo S, Martinelli G, Martelli M, Rigacci L, Arcaini L, Di Raimondo F, Merli F, Sabattini E, McLaughlin P, Solal-Céligny P (2009) Follicular lymphoma international prognostic index 2: a new prognostic index for follicular lymphoma developed by the international follicular lymphoma prognostic factor project. J Clin Oncol 27(27):4555–4562. https://doi.org/10.1200/JCO.2008.21.3991
Wang ZY, Li YX, Wang H, Wang WH, Jin J, Liu YP, Song YW, Wang SL, Liu XF, Yu ZH (2011) Unfavorable prognosis of elderly patients with early-stage extranodal nasal-type NK/T-cell lymphoma. Ann Oncol 22(2):390–396. https://doi.org/10.1093/annonc/mdq347
Liu WX, Shi M, Su H, Wang Y, He X, Xu LM, Yuan ZY, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Zhang YJ, Zhu Y, Cao JZ, Lan SM, Wu JX, Wu T et al (2019) Effect of age as a continuous variable on survival outcomes and treatment selection in patients with extranodal nasal-type NK/T-cell lymphoma from the China Lymphoma Collaborative Group (CLCG). Aging 11(19):8463–8473. https://doi.org/10.18632/aging.102331
Chen B, Zhu SY, Shi M, Su H, Wang Y, He X, Xu LM, Yuan ZY, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Zhang YJ, Zhu Y, Cao JZ, Lan SM, Wu JX et al (2018) Risk-dependent curability of radiotherapy for elderly patients with early-stage extranodal nasal-type NK/T-cell lymphoma: a multicenter study from the China Lymphoma Collaborative Group (CLCG). Cancer Med 7(12):5952–5961. https://doi.org/10.1002/cam4.1849
Zhao YT, Wang Y, Qi SN, Yang Y, He X, Zhang YJ, Huang HQ, Zhang LL, Wu G, Qu BL, Qian LT, Hou XR, Zhang FQ, Qiao XY, Wang H, Li GF, Zhu Y, Cao JZ, Wu JX et al (2021) Clinical features and treatment outcome of extranodal nasal-type NK/T-cell lymphoma of the extra-upper aerodigestive tract. Zhonghua Zhong Liu Za Zhi 43(7):787–794. https://doi.org/10.3760/cma.j.cn112152-20191207-00789
Xiong J, Cui BW, Wang N, Dai YT, Zhang H, Wang CF, Zhong HJ, Cheng S, Ou-Yang BS, Hu Y, Zhang X, Xu B, Qian WB, Tao R, Yan F, Hu JD, Hou M, Ma XJ, Wang X et al (2020) Genomic and transcriptomic characterization of natural killer T cell lymphoma. Cancer Cell 37(3):403–419.e406. https://doi.org/10.1016/j.ccell.2020.02.005
Funding
The present work was supported by grants from the National Key Research and Development of China (2020AAA0109504) and the National Natural Science Foundation of China (81970185).
Author information
Authors and Affiliations
Contributions
YXL and SNQ designed the research; JYL, SNQ, XRH, SYC, and XL collected and analyzed the data; JYL, SYC, XL, and HC performed the statistical analysis; YXL, JYL, and SNQ wrote the paper; all authors provided study materials or patient data and approved the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, JY., Hou, XR., Chen, SY. et al. Outcome and risk prediction of early progression in patients with extranodal natural killer/T cell lymphoma from the CLCG study. Ann Hematol 102, 2459–2469 (2023). https://doi.org/10.1007/s00277-023-05311-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05311-5