Summary
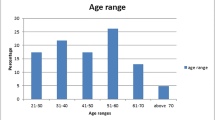
Fournier’s gangrene (FG) is an extremely aggressive and rapidly progressive polymicrobial soft tissue infection of the perineum, anal area or genitalial regions with a high mortality rate. The objectives of this study were to share our experience with the management of this serious infectious disease over the last 15 years. This retrospective study examined 24 patients diagnosed as having FG who were admitted to our hospital between March 1996 and December 2011. The gender, age, etiology, predisposing factors, laboratory findings, treatment modality, hospitalization time and spread of gangrene of the subjects were all recorded and analyzed. The results showed that the mean age of the patients was 48.33 years, the male-to-female ratio was 5:1 and the mortality rate was 20.8% (5/24). The most common predisposing factor was diabetes mellitus in 10 patients (41.6%), followed by alcohol abuse, obesity, neoplasms and immunosuppression. The most common etiology was peri-anal and peri-rectal abscesses (45.8%), followed by lesions of urogenital origin (33.3%) and cutaneous (8.3%) origin. No local pathologies could be identified in 3 (12.5%) patients. The most commonly isolated microorganisms were Escherichia coli (62.5%), followed by Enterococcus, Pseudomonas aeruginosa and Staphylococcus aureus. The median admission Fournier’s gangrene severity index (FGSI) score for survivors was 5.63±1.89 against 13.6±3.64 for non-survivors which was designed for predicting the disease severity in the series. Early diagnosis and immediate extensive surgical debridement were significant prognostic factors in the management of Fournier gangrene. Individualized reconstructive modalities for wound coverage were useful in that they repaired the tissue defect and improved the quality of life. We are led to conclude that Fournier’s gangrene is a severe condition with a high mortality. The Fournier’s gangrene severity index (FGSI) score at admission serves as a good predictor for the disease severity. Early diagnosis, surgical debridement and aggressive fluid therapy are significant prognostic factors in the management of Fournier gangrene. Individualized reconstructive surgery modalities for wound coverage are useful to correct the tissue defect and improve the quality of life.
Similar content being viewed by others
References
Czymek R, Hildebrand P, Kleemann M, et al. New insights into the epidemiology and etiology of Fournier’s gangrene: a review of 33 patients. Infection, 2009,37(4): 306–312
Laor E, Palmer LS, Tolia BM, et al. Outcome prediction in patients with Fournier’s gangrene. J Urol, 1995,154(1): 89–92
Erol B, Tuncel A, Hanci V, et al. Fournier’s gangrene: overview of prognostic factors and definition of new prognostic parameter. Urology, 2010,75(5):1193–1198
Grabe M, Bjerklund-Johansen TE, Botto H. Guidelines on Urological Infections. European Association of Urology, 2011, Update March 2011:76–78
Sorensen MD, Krieger JN, Rivara FP, et al. Fournier’s Gangrene: population based epidemiology and outcomes. J Urol, 2009,181(5):2120–2126
Eke N. Fournier’s gangrene: a review of 1726 cases. Br J Surg, 2000,87(6):718–728
Levenson RB, Singh AK, Novelline RA. Fournier gangrene: role of imaging. Radiographics, 2008,28(2): 519–528
Papaconstantinou I, Yiallourou AI, Dafnios N, et al. Successful treatment of a severe case of fournier’s gangrene complicating a perianal abscess. Case Report Med, 2011, 2011:702429
Villanueva-Saenz E, Martinez Hernandez-Magro P, Valdes Ovalle M, et al. Experience in management of Fournier’s gangrene. Tech Coloproctol, 2002,6(1):5–10
Korkut M, Icoz G, Dayangac M, et al. Outcome analysis in patients with Fournier’s gangrene: report of 45 cases. Dis Colon Rectum, 2003,46(5):649–652
Unalp HR, Kamer E, Derici H, et al. Fournier’s gangrene: evaluation of 68 patients and analysis of prognostic variables. J Postgrad Med, 2008,54(2):102–105
Ersay A, Yilmaz G, Akgun Y, et al. Factors affecting mortality of Fournier’s gangrene: review of 70 patients. ANZ J Surg, 2007,77(1–2):43–48
Tuncel A, Aydin O, Tekdogan U, et al. Fournier’s gangrene: Three years of experience with 20 patients and validity of the Fournier’s gangrene severity index score. Eur Urol, 2006,50(4):838–843
Koukouras D, Kallidonis P, Panagopoulos C, et al. Fournier’s gangrene, a urologic and surgical emergency: presentation of a multi-institutional experience with 45 cases. Urol Int, 2011,86(2):167–172
Bartolotta TV, Midiri M, Caruso G, et al. Necrotizing fasciitis of the scrotum (Fournier’s gangrene): ultrasound findings. Radiol Med, 2000,100(6):510–512
Kickuth R, Adams S, Kirchner J, et al. Magnetic resonance imaging in the diagnosis of Fournier’s gangrene. Eur Radiol, 2001,11(5):787–790
Gosi G, Munch Z. Fournier’s gangrene: early diagnosis is the best remedy. Magy Seb, 2002,55(1):27–30
Singh G, Sinha SK, Adhikary S, et al. Necrotising infections of soft tissues-a clinical profile. Eur J Surg, 2002, 168(6):366–371
Sugishita Y, Nagashima M, Ooshiro M, et al. Fournier’s gangrene progressing from the buttocks to the scrotum following a perianal abscess. J Infect Chemother, 2008, 14(1):56–58
Chen SY, Fu JP, Wang CH, et al. Fournier gangrene: a review of 41 patients and strategies for reconstruction. Ann Plast Surg, 2010,64(6):765–769
Moslemi MK, Sadighi Gilani MA, et al. Fournier gangrene presenting in a patient with undiagnosed rectal adenocarcinoma: a case report. Cases J, 2009,2:9136
Czymek R, Schmidt A, Eckmann C, et al. Fournier’s gangrene: vacuum-assisted closure versus conventional dressings. Am J Surg, 2009,197(2):168–176
Ekelius L, Bjorkman H, Kalin M, et al. Fournier’s gangrene after genital piercing. Scand J Infect Dis, 2004, 36(8):610–612
Purnell D, Hazlett T, Alexander SL. A new weapon against severe sepsis related to necrotizing fasciitis. Dimens Crit Care Nurs, 2004,23(1):18–23
Jallali N, Withey S, Butler PE. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. Am J Surg, 2005,189(4):462–466
Assenza M, Cozza V, Sacco E, et al. VAC (Vacuum Assisted Closure) treatment in Fournier’s gangrene: personal experience and literature review. Clin Ter, 2011,162(1): e1–e5
Jeong HJ, Park SC, Seo IY, et al. Prognostic factors in Fournier gangrene. Int J Urol, 2005,12(12):1041–1044
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Han, X., Liu, M. et al. Experience in management of Fournier’s gangrene: A report of 24 cases. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 32, 719–723 (2012). https://doi.org/10.1007/s11596-012-1024-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-012-1024-4