Abstract
Purpose
The benefits of parenteral nutrition and hydration (PNH) in patients with advanced cancer remain unknown. Therefore, we conducted a prospective multicenter cohort study to assess the effects of PNH on survival in patients with malignant bowel obstruction (MBO).
Methods
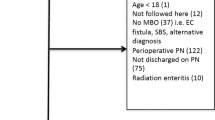
The present study was a secondary analysis. Data on primary nutritional administration routes during the first week of admission to palliative care units, i.e., parenteral nutrition and parenteral hydration, were obtained. Data on the averaged calorie sufficiency rate/total calorie intake (75% ≤ or 750 kcal/day ≤ , 50–75% or 500–750 kcal/day, 25–50% or 250–500 kcal/day, and < 25% or < 250 kcal/day) were also obtained. Participants with MBO were included and divided into two groups: PNH-high (25% ≤ or 250 kcal/day ≤) and PNH-low (< 25% or < 250 kcal/day). We performed time-to-event analyses using the Kaplan–Meier method, log-rank test, and univariate and multivariate Cox regression analyses.
Results
Patients were divided into the PNH-high (n = 68) and PNH-low (n = 76) groups. A significant difference was observed in survival rates between the two groups (log-rank P < 0.001). Median survival times were 35.5 (95% CI 27–44) and 17.5 (95% CI 13–21) days, respectively. In the multivariate-adjusted model, a significantly lower risk of mortality was observed in Cox’s proportional hazard model in the PNH-high group (HR 0.55 (95% CI 0.36–0.83), P = 0.005) than in the PNH-low group.
Conclusion
The present results indicated the beneficial effects of PNH for prolonging survival in advanced cancer patients with MBO in palliative care units.

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the present study were not publicly available as sharing is not explicitly covered by patient consent.
Code availability
Not applicable.
References
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36(1):11–48
Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP et al (2017) ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr 36(5):1187–1196
Roeland EJ, Bohlke K, Baracos VE, Bruera E, Del Fabbro E, Dixon S et al (2020) Management of cancer cachexia: ASCO guideline. J Clin Oncol 38(21):2438–2453
Raijmakers NJ, van Zuylen L, Costantini M, Caraceni A, Clark J, Lundquist G et al (2011) Artificial nutrition and hydration in the last week of life in cancer patients. A systematic literature review of practices and effects. Ann Oncol 22:1478–1486
Good P, Richard R, Syrmis W, Jenkins-Marsh S, Stephens J (2014) Medically assisted nutrition for adult palliative care patients (Review). Cochrane Database Syst Rev (4):CD006274
Hui D, Dev R, Bruera E (2015) The last days of life: symptom burden and impact on nutritional and hydration in cancer patients. Curr Opin Support Palliat Care 9(4):346–354
Orrevall Y (2015) Nutritional support at the end of life. Nutrition 31(4):615–616
Tobberup R, Thoresen L, Falkmer UG, Yilmaz MK, Solheim TS, Balstad TR (2019) Effects of current parenteral nutrition treatment on health-related quality of life, physical function, nutritional status, survival and adverse events exclusively in patients with advanced cancer: A systematic literature review. Crit Rev Oncol Hematol 139:96–107
Bouleuc C, Anota A, Cornet C, Grodard G, Thiery-Vuillemin A, Dubroeucq O et al (2020) Impact on health-related quality of life of parenteral nutrition for patients with advanced cancer cachexia: results from a randomized controlled trial. Oncologist 25(5):843–851
Amano K, Maeda I, Ishiki H, Miura T, Hatano Y, Tsukuura H, et al. Effects of enteral nutrition and parenteral nutrition on survival in patients with advanced cancer cachexia: analysis of a multicenter prospective cohort study. Clin Nutr. https://doi.org/10.1016/j.clnu.2020.07.027
Sowerbutts AM, Lal S, Sremanakova J, Clamp A, Todd C, Jayson GC et al (2018) Home parenteral nutrition for people with inoperable malignant bowel obstruction. Cochrane Database Syst Rev 8(8):CD012812. https://doi.org/10.1002/14651858.CD012812.pub2
Bozzetti F (2019) The role of parenteral nutrition in patients with malignant bowel obstruction. Support Care Cancer 27(12):4393–4399
Anthony T, Baron T, Mercadante S, Green S, Chi D, Cunningham J et al (2007) Report of the clinical protocol committee: development of randomized trials for malignant bowel obstruction. J Pain Symptom Manage 34:S49–S59
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Cotogni P, Ossola M, Passera R, Monge T, Fadda M, De Francesco A, Bozzetti F (2020) Home parenteral nutrition versus artificial hydration in malnourished patients with cancer in palliative care: a prospective, cohort survival study. BMJ Support Palliat Care 21:bmjspcare-2020–002343. https://doi.org/10.1136/bmjspcare-2020-002343
Naghibi M, Smith TR, Elia M (2015) A systematic review with meta-analysis of survival, quality of life and cost-effectiveness of home parenteral nutrition in patients with inoperable malignant bowel obstruction. Clin Nutr 34(5):825–837
Ganzini L, Goy ER, Miller LL, Harvath TA, Jackson A, Delorit MA (2003) Nurses’ experiences with hospice patients who hasten death. N Engl J Med 349(4):359–365
Bolt EE, Hagens M, Willems D, Onwuteaka-Philipsen BD (2015) Primary care patients hastening death by voluntarily stopping eating and drinking. Ann Fam Med 13(5):421–428
Bozzetti F (2020) Is there a place for nutrition in palliative care? Support Care Cancer 28(9):4069–4075
Oh SY, Jun HJ, Park SJ, Park IK, Lim GJ, Yu Y et al (2014) A randomized phase II study to assess the effectiveness of fluid therapy or intensive nutritional support on survival in patients with advanced cancer who cannot be nourished via enteral route. J Palliat Med 17(11):1266–1270
Sowerbutts AM, Lal S, Sremanakova J, Clamp AR, Jayson GC, Teubner A et al (2019) Palliative home parenteral nutrition in patients with ovarian cancer and malignant bowel obstruction: experiences of women and family caregivers. BMC Palliat Care 18:120
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
Amano K, Morita T, Miyamoto J, Uno T, Katayama H, Tatara R (2018) Perception of need for nutritional support in advanced cancer patients with cachexia: a survey in palliative care settings. Support Care Cancer 26(8):2793–2799
Amano K, Maeda I, Morita T, Masukawa K, Kizawa Y, Tsuneto S et al (2020) Beliefs and perceptions about parenteral nutrition and hydration by family members of patients with advanced cancer admitted to palliative care units: a nationwide survey of bereaved family members in Japan. J Pain Symptom Manage 60(2):355–361
Park EJ, Park K, Kim J, Oh S, Jung KS, Oh SY, et al (2020) Safety, efficacy, and patient satisfaction with initial peripherally inserted central catheters compared with usual intravenous access in terminally Ill cancer patients: a randomized phase II study. Cancer Res Treat 22. https://doi.org/10.4143/crt.2020.1008
Acknowledgements
This study was performed in the East-Asian Collaborative Cross-Cultural Study to Elucidate the Dying process (EASED). The participating study sites and site investigators in Japan were as follows: Satoshi Inoue, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Naosuke Yokomichi, M.D., Ph.D. (Department of Palliative and Supportive Care, Seirei Mikatahara General Hospital), Kengo Imai, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Hiroaki Tsukuura, M.D., Ph.D. (Department of Palliative Care, TUMS Urayasu Hospital), Toshihiro Yamauchi, M.D. (Seirei Hospice, Seirei Mikatahara General Hospital), Yu Uneno, M.D. (Department of Therapeutic Oncology, Graduate School of Medicine, Kyoto University), Akira Yoshioka, M.D., Ph.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Shuji Hiramoto, M.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Ayako Kikuchi, M.D. (Department of Oncology and Palliative Medicine, Mitsubishi Kyoto Hospital), Tetsuo Hori, M.D. (Department of Respiratory surgery, Mitsubishi Kyoto Hospital), Yosuke Matsuda, M.D. (Palliative Care Department, St.Luke’s International Hospital), Hiroyuki Kohara, M.D., Ph.D. (Hiroshima Prefectural Hospital), Hiromi Funaki, M.D. (Hiroshima Prefectural Hospital), Keiko Tanaka, M.D., Ph.D. (Department of Palliative Care Tokyo Metropolitan Cancer & Infectious Diseases Center Komagome Hospital), Kozue Suzuki, M.D. (Department of Palliative Care Tokyo Metropolitan Cancer & Infectious Diseases Center Komagome Hospital), Tina Kamei, M.D. (Department of Palliative Care, NTT Medical Center Tokyo), Yukari Azuma, M.D. (Home Care Clinic Aozora Shin-Matsudo), Teruaki Uno, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Jiro Miyamoto, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Hirofumi Katayama, M.D. (Department of Palliative Medicine, Osaka City General Hospital), Hideyuki Kashiwagi, M.D., MBA. (Aso Iizuka Hospital/Transitional and Palliative Care), Eri Matsumoto, M.D. (Aso Iizuka Hospital/Transitional and Palliative Care), Kiyofumi Oya, M.D. (Aso Iizuka Hospital/Transitional and Palliative Care), Takeya Yamaguchi, M.D. (Japan Community Health care Organization Kyushu Hospital / Palliative Care), Tomonao Okamura, M.D., MBA. (Aso Iizuka Hospital/Transitional and Palliative Care), Hoshu Hashimoto, M.D., MBA (Inoue Hospital/Internal Medicine), Shunsuke Kosugi, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Nao Ikuta, M.D. (Department of Emergency Medicine, Osaka Red Cross Hospital), Yaichiro Matsumoto, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Takashi Ohmori, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Takehiro Nakai, M.D. (Immuno-Rheumatology Center, St Luke's International Hospital), Takashi Ikee, M.D. (Department of Cardiorogy, Aso Iizuka Hospital), Yuto Unoki, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Kazuki Kitade, M.D. (Department of Orthopedic Surgery, Saga-Ken Medical Centre Koseikan), Shu Koito, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Nanao Ishibashi, M.D. (Environmental Health and Safety Division, Environmental Health Department, Ministry of the Environment), Masaya Ehara, M.D. (TOSHIBA), Kosuke Kuwahara, M.D. (Department of General Internal Medicine, Aso Iizuka Hospital), Shohei Ueno, M.D. (Department of Hematology/Oncology, Japan Community Healthcare Organization Kyushu Hospital), Shunsuke Nakashima, M.D. (Oshima Clinic), Yuta Ishiyama, M.D. (Department of Transitional and Palliative Care, Aso Iizuka Hospital), Akihiro Sakashita, M.D., Ph.D. (Department of Palliative Medicine, Kobe University School of Medicine), Ryo Matsunuma, M.D. (Department of Palliative Medicine, Kobe University Graduate School of Medicine), Hana Takatsu, M.D. (Division of Palliative Care, Konan Medical Center), Takashi Yamaguchi, M.D., Ph.D. (Division of Palliative Care, Konan Medical Center), Satoko Ito, M.D. (Hospice, The Japan Baptist Hospital), Toru Terabayashi, M.D. (Hospice, The Japan Baptist Hospital), Jun Nakagawa, M.D. (Hospice, The Japan Baptist Hospital), Tetsuya Yamagiwa, M.D., Ph.D. (Hospice, The Japan Baptist Hospital), Akira Inoue, M.D., Ph.D. (Department of Palliative Medicine Tohoku University School of Medicine), Takuhiro Yamaguchi, Ph.D. (Professor of Biostatistics, Tohoku University Graduate School of Medicine), Mitsunori Miyashita, R.N., Ph.D. (Department of Palliative Nursing, Health Sciences, Tohoku University Graduate School of Medicine), Saran Yoshida, Ph.D. (Graduate School of Education, Tohoku University), Yusuke Hiratsuka, M.D., Ph.D. (Department of Palliative Medicine Tohoku University School of Medicine), Keita Tagami, M.D., Ph.D. (Department of Palliative Medicine Tohoku University School of Medicine), Hiroaki Watanabe, M.D. (Department of Palliative Care, Komaki City Hospital), Takuya Odagiri, M.D. (Department of Palliative Care, Komaki City Hospital), Masayuki Ikenaga, M.D. (Hospice, Yodogawa Christian Hospital), Keiji Shimizu, M.D., Ph.D. (Department of Palliative Care Internal Medicine, Osaka General Hospital of West Japan Railway Company), Akira Hayakawa, M.D., Ph.D. (Hospice, Yodogawa Christian Hospital), Rena Kamura, M.D. (Hospice, Yodogawa Christian Hospital), Takeru Okoshi, M.D., Ph.D. (Okoshi Nagominomori Clinic), Tomohiro Nishi, M.D. (Kawasaki Municipal Ida Hospital, Kawasaki Comprehensive Care Center), Yasuhiro Shibata, M.D. (Kawasaki Municipal Ida Hospital, Kawasaki Comprehensive Care Center), Takayuki Hisanaga, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Takahiro Higashibata, M.D., Ph.D. (Department of General Medicine and Primary Care, Palliative Care Team, University of Tsukuba Hospital), Ritsuko Yabuki, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Shingo Hagiwara, M.D., Ph.D. (Department of Palliative Medicine, Yuai Memorial Hospital), Miho Shimokawa, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Junko Nozato, M.D. (Department of Clinical Oncology Graduate School of Medical and Dental Sciences Tokyo Medical and Dental University (TMDU)), Tetsuji Iriyama, M.D. (Specially Appointed Assistant Professor, Department of Internal Medicine, Palliative Care, Medical Hospital, Tokyo Medical and Dental University), Keisuke Kaneishi, M.D., Ph.D. (Department of Palliative Care Unit, JCHO Tokyo Shinjuku Medical Center), Mika Baba, M.D., Ph.D. (Department of Palliative medicine Suita Tokushukai Hospital), Yoshihisa Matsumoto, M.D., Ph.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Ayumi Okizaki, Ph.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yuki Sumazaki Watanabe, M.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Yuko uehara, M.D. (Department of Palliative Medicine, National Cancer Center Hospital East), Eriko Satomi, M.D. (Department of palliative medicine, National Cancer Center Hospital), Kaoru Nishijima, M.D. (Department of Palliative Medicine, Kobe University Graduate School of Medicine), Junichi Shimoinaba, M.D. (Department of Hospice Palliative Care, Eikoh Hospital), Ryoichi Nakahori, M.D. (Department of Palliative Care, Fukuoka Minato Home Medical Care Clinic), Takeshi Hirohashi, M.D. (Eiju General Hospital), Jun Hamano, M.D., Ph.D. (Assistant Professor, Faculty of Medicine, University of Tsukuba), Natsuki Kawashima, M.D. (Department of Palliative Medicine, Tsukuba Medical Center Hospital), Takashi Kawaguchi, Ph.D. (Tokyo University of Pharmacy and Life Sciences Department of Practical Pharmacy), Megumi Uchida, M.D., Ph.D. (Dept. of Psychiatry and Cognitive-Behavioral Medicine, Nagoya City University Graduate School of Medical Sciences), Ko Sato, M.D., Ph.D. (Hospice, Ise Municipal General Hospital), Yoichi Matsuda, M.D., Ph.D. (Department of Anesthesiology & Intensive Care Medicine/Osaka University Graduate School of Medicine), Satoru Tsuneto, M.D., Ph.D. (Professor, Department of Human Health Sciences, Graduate School of Medicine, Kyoto University Department of Palliative Medicine, Kyoto University Hospital), Sayaka Maeda, M.D. (Department of Palliative Medicine, Kyoto University Hospital), Yoshiyuki Kizawa M.D., Ph.D., FJSIM, DSBPMJ. (Designated Professor and Chair, Department of Palliative Medicine, Kobe University School of Medicine), Hiroyuki Otani, M.D. (Palliative Care Team, and Palliative and Supportive Care, National Kyushu Cancer Center).
Funding
The present study was supported in part by a Grant-in-Aid from the Japan Hospice Palliative Care Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: Koji Amano, Isseki Maeda, Yutaka Hatano, Masanori Mori, Tatsuya Morita.
Collection and/or assembly of data: All authors.
Statistical analysis: Sayaka Arakawa, Koji Amano, Shunsuke Oyamada.
Data analysis and interpretation: Sayaka Arakawa, Koji Amano, Shunsuke Oyamada, Isseki Maeda, Yutaka Hatano, Masanori Mori, Tatsuya Morita.
Drafting of the manuscript: Sayaka Arakawa, Koji Amano, Shunsuke Oyamada.
Final approval of the manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval
The present study was approved by the local Institutional Review Boards of all participating institutions.
Consent to participate
Since Japanese law does not require individual informed consent from participants in a non-invasive observational trial, we used an opt-out method rather than acquiring written or oral informed consent.
Consent for publication
All authors agree to submit.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arakawa, S., Amano, K., Oyamada, S. et al. Effects of parenteral nutrition and hydration on survival in advanced cancer patients with malignant bowel obstruction: secondary analysis of a multicenter prospective cohort study. Support Care Cancer 29, 7541–7549 (2021). https://doi.org/10.1007/s00520-021-06293-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06293-8