Abstract
Background
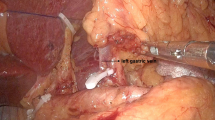
The aim of this retrospective matched‐paired cohort study was to clarify the effectiveness of preserving the vagus nerve in totally laparoscopic radical distal gastrectomy (TLDG).
Methods
One hundred eighty-three patients with gastric cancer who underwent TLDG between February 2020 and March 2022 were included and followed up. Sixty-one patients with preservation of the vagal nerve (VPG) in the same period were matched (1:2) to conventional sacrificed (CG) cases for demographics, tumor characteristics, and tumor node metastasis stage. The evaluated variables included intraoperative and postoperative indices, symptoms, nutritional status, and gallstone formation at 1 year after gastrectomy between the two groups.
Results
Although the operation time was significantly increased in the VPG compared with the CG (198.0 ± 35.2 vs. 176.2 ± 35.2 min, P < 0.001), the mean time of gas passage in the VPG was significantly lower than that in the CG (68.1 ± 21.7 h vs. 75.4 ± 22.6 h, P = 0.038). The overall postoperative complication rate was similar between the two groups (P = 0.794). There was no statistically significant difference between the two groups hospital stay, total number of harvested lymph nodes, and mean number of examined lymph nodes at each station. During follow-up, the morbidity of gallstones or cholecystitis (8.2% vs. 20.5%, P = 0.036), chronic diarrhea (3.3% vs. 14.8%, P = 0.022), and constipation (4.9% vs. 16.4%, P = 0.032) were significantly lower in the VPG than in the CG in this study. Moreover, injury to the vagus nerve was found to be an independent risk factor for gallstone formation or cholecystitis and chronic diarrhea in univariate analysis and multivariate analysis.
Conclusion
The vagus nerve plays an imperative role in gastrointestinal motility, and hepatic and celiac branch preservation mainly exerts efficacy and safety in patients who undergo TLDG.



Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Cancerincidence and mortality in China (2016) (2016) Journal of the National Cancer Center Cancerstatistics in China, 2015. CA Cancer J Clin 66(2):115–132
Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, Xue Y, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Chen P, Liu H, Zheng C, Liu F, Yu J, Li Z, Zhao G, Chen X, Wang K, Li P, Xing J, Li G (2016) Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol 34(12):1350–1357
Katai H, Mizusawa J, Katayama H, Morita S, Yamada T, Bando E, Ito S, Takagi M, Takagane A, Teshima S, Koeda K, Nunobe S, Yoshikawa T, Terashima M, Sasako M (2020) Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol 5(2):142–151
Japanese Gastric Cancer Association (2021) Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 24(1):1–21
Takachi K, Doki Y, Ishikawa O et al (2006) Postoperative ghrelin levels and delayed recovery from body weight loss after distal or total gastrectomy. J Surg Res 130:1
Ahn SH, Lee JH, Park DJ et al (2013) Comparative study of clinical outcomes between laparoscopy-assisted proximal gastrectomy (LAPG) and laparoscopy-assisted total gastrectomy (LATG) for proximal gastric cancer. Gastric Cancer 16:282–289
Liu YF, Cui XY, Zhang Y, Cao L, Hu X (2020) Efficacy of celiac branch preservation in Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. J Surg Res 245:330–337
Yunoki Y (1995) Effects of resection of celiac and pyloric branches of vagus nerve on the interdigestive motor activity of the upper digestive tract and biliary tree. J Smooth Muscle Res 31:33–41
Niijima A (1989) Nervous regulation of metabolism. Prog Neurobiol 33:135
Le MJ (1984) Metabolic and feeding patterns: role of sympathetic and parasympathetic efferent pathways. J Auton Nerv Syst 10:325
Kim SM, Cho J, Kang D, Oh SJ, Kim AR, Sohn TS, Noh JH, Kim S (2016) A randomized controlled trial of vagus nerve-preserving distal gastrectomy versus conventional distal gastrectomy for postoperative quality of life in early stage gastric cancer patients. Ann Surg 263(6):1079–1084
Furukawa H, Ohashi M, Honda M et al (2018) Preservation of the celiac branch of the vagal nerve for pylorus-preserving gastrectomy: is it meaningful? Gastric Cancer 21(3):516–523
Yoshida K, Honda M, Kumamaru H et al (2018) Surgical outcomes of laparoscopic distal gastrectomy compared to open distal gastrectomy: a retrospective cohort study based on a nationwide registry database in Japan. Ann Gastroenterol Surg 2(1):55–64
Amin MB, Edge SB, Greene FL et al (2016) AJCC cancer staging manual, 8th edn. Springer, New York, pp 203–220
Suh YS, Han DS, Kong SH et al (2014) Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg 259(3):485–493
Tokunaga M, Hiki N, Fukunaga T et al (2011) Is preservation of the celiac branch of the vagal nerve effective in preventing stasis following pylorus-preserving gastrectomy? Hepatogastroenterology 58(107–108):1046–1050
Wang FB, Powley TL (2008) Vagal innervation of intestines:afferent pathways mapped with newen bloc horseradish peroxidase adaptmion. Cell Tissue Res 329(2):221–230
Kim HH, Park MI, Lee SH et al (2012) Effects of vagus nerve preservation and vagotomy on peptide YY and body weight after subtotal gastrectomy. World J Gastroenterol 18(30):4044–4050
Kojima K, Yamada H, Inokuchi M et al (2008) Functional evaluation after vagus-nerve-sparing laparoscopically assisted distal gastrectomy. Surg Endosc 22(9):2003–2008
Aizawa M, Honda M, Hiki N et al (2017) Oncological outcomes of function-preserving gastrectomy for early gastric cancer: a multicenter propensity score matched cohort analysis comparing pylorus-preserving gastrectomy versus conventional distal gastrectomy. Gastric Cancer 20(4):709–717
Tomita R (2016) Surgical techniques to prevent reflux esophagitis in proximal gastrectomy reconstructed by esophagogastrostomy with preservation of the lower esophageal sphincter, pyloric and celiac branches of the vagal nerve, and reconstruction of the new His angle for early proximal gastric cancer. Surg Today 46(7):827–834
Hiramatsu Y, Kikuchi H, Takeuchi H (2021) Function-preserving gastrectomy for early gastric cancer. Cancers (Basel) 13(24):6223
Sun W, Deng J, He W et al (2020) Should the left gastric artery lymph node be considered as the predictive lymph node for extra-gastric lymph node metastases? Ann Transl Med 8(11):680
Ando S, Tsuji H (2008) Surgical technique of vagus nerve-preserving gastrectomy with D2, lymphadenectomy for gastric cancer. ANZ J Surg 78(3):172–176
Ladas SD, Isaacs PE, Quereshi Y et al (1983) Role of the small intestine in postvagotomy diarrhea. Gastroenterology 85:1088–1093
Rosa-e-Silva L, Troncon LE, Oliveira RB, Foss MC, Braga FJ, Gallo JL (1996) Rapid distal small bowel transit associated with sympathetic denervation in type I diabetes mellitus. Gut 39(5):748–756
Mao X, Xu X, Zhu H et al (2020) A comparison between pylorus-preserving and distal gastrectomy in surgical safety and functional benefit with gastric cancer: a systematic review and meta-analysis. World J Surg Oncol 18(1):160
Ikeguchi M, Watanabe J, Kuroda H et al (2011) Operative procedure for laparoscopy-assisted vagus nerve and pylorus-preserving gastrectomy (LAVNPPG) for early gastric cancer. Yonago Acta Med 54(4):59–63
Uyama I, Sakurai Y, Komori Y, Nakamura Y, Syoji M, Tonomura S, Yoshida I, Masui T, Ochiai M (2005) Laparoscopic gastrectomy with preservation of the vagus nerve accompanied by lymph node dissection for early gastric carcinoma. J Am Coll Surg 200(1):140–145
Author information
Authors and Affiliations
Contributions
ZKX and HX designed this study. LJW, YWQ, LY, and DCZ collected and analyzed the data. ZL, ZYH, and QYL were responsible for the follow-up of patients. YWQ and LJW participate in drafting the article. FYL and WZW revised the paper.
Corresponding author
Ethics declarations
Disclosures
Drs. Hao Xu, Linjun Wang, Yawei Qian, Zhongyuan He, Fengyuan Li, Weizhi Wang, Zheng Li, Qingya Li, Diancai Zhang, Li Yang, and Zekuan Xu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, H., Wang, L., Qian, Y. et al. Effectiveness of preserved vagal nerve in totally laparoscopy radical distal gastrectomy: a matched‐paired cohort analysis. Surg Endosc 37, 7538–7547 (2023). https://doi.org/10.1007/s00464-023-10254-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10254-z