Abstract
In 2020, the COVID-19 pandemic followed a two-wave pattern in most countries. Hospital admission for COVID-19 in one wave or another could have affected mortality, especially among the older persons. The objective of this study was to evaluate whether the admission of older patients during the different waves, before SARS-CoV-2 vaccination was available, was associated with a different mortality. We compared the mortality rates of patients hospitalized during 2020 before (first wave) and after (second wave) July 7, 2020, included in the SEMI-COVID-19 Registry, a large, multicenter, retrospective cohort of patients admitted to 126 Spanish hospitals for COVID-19. A multivariate logistic regression analysis was performed to control for changes in either the patient or disease profile. As of December 26, 2022, 22,494 patients had been included (17,784 from the first wave and 4710 from the second one). Overall mortality was 20.4% in the first wave and 17.2% in the second wave (risk difference (RD) − 3.2%; 95% confidence interval (95% CI) − 4.4 to − 2.0). Only patients aged 70 and older (10,973 patients: 8571 in the first wave and 2386 in the second wave) had a significant reduction in mortality (RD − 7.6%; 95% CI − 9.7 to − 5.5) (unadjusted relative risk reduction: 21.6%). After adjusting for age, comorbidities, variables related to the severity of the disease, and treatment received, admission during the second wave remained a protective factor. In Spain, patients aged 70 years and older admitted during the second wave of the COVID-19 pandemic had a significantly lower risk of mortality, except in severely dependent persons in need of corticosteroid treatment. This effect is independent of patient characteristics, disease severity, or treatment received. This suggests a protective effect of a better standard of care, greater clinical expertise, or a lesser degree of healthcare system overload.
Similar content being viewed by others
Introduction
The coronavirus disease 19 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a major, life-changing event that continues to overwhelm man’s collective mind. As of June 15, 2021, 175,333,154 infections and 3,793,230 deaths had been reported worldwide1. In 2020, most countries experienced at least two waves of the pandemic.
Patients with COVID-19 who require hospitalization have a high mortality rate. The in-hospital mortality rate was very high in the early phases of the pandemic, though there was a great degree of variability among countries and even areas, with mortality rates ranging from 12% up to 28%2,3,4,5,6. Mortality is higher in older patients (especially those over 79 years)5,7 as well as in patients with certain underlying conditions8.
Mortality is one of the main measures of severity of any epidemic. It is prone to change over time due to improved comprehension of the disease and the development of better treatments. COVID-19 mortality has fluctuated over time9,10,11 and varies according to geography12,13. In most countries, the pandemic followed a two-wave pattern in 2020, with a first wave in the spring and a second wave starting in late summer or early autumn. In North America10 and Europe14,15,16, mortality was higher in the first wave whereas in Africa17 and Brazil18, it was higher in the second wave.
In Spain, this evolution has yet to be thoroughly studied. The first wave was followed by three more waves (in early autumn, late autumn, and midwinter of 2020), each of which had lower death tolls and unadjusted mortality rates. A single-center study in Reus, Spain19 has shown that, after controlling for known mortality factors, there was still a lower mortality rate in the second wave.
According to our preliminary data, we hypothesized that hospital admission in the different waves could affect the mortality of patients with COVID-19, especially the older people. The primary aim of the study was to evaluate whether the admission of older patients during the different waves of 2020 was associated with a different mortality rate and whether this could be explained by differences in the characteristics of either the patients or the severity of the disease.
Results
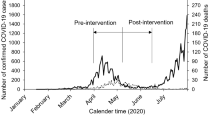
Mortality estimation and case fatality rates in first and second waves
As of December 26, 2020, a total of 22,494 patients had been included in the SEMI-COVID-19 Registry: 17,784 patients from the first wave and 4710 patients from the second wave. Overall mortality was 20.4% in the first wave and 17.2% in the second wave (RD − 3.2%; 95% CI − 4.4 to − 2.0). Figure 1 shows the case fatality rate stratified by age. As there were no differences in mortality according to wave in patients younger than 70 years, we focused the study on patients who were 70 years of age and older (10,973 patients: 8587 from the first wave and 2386 from the second wave). As has been observed in previous studies, mortality rose with age but was consistently lower in the second wave in patients older than 70 years: 35.2% and 27.6% in first and second waves, respectively, which represents a 7.8% absolute risk reduction and 21.6% relative risk reduction.
Case Fatality Rate (CFR) according to age in patients hospitalized during the first and second waves of COVID-19, expressed as percentage (deceased patients/total patients). The diamonds indicate the point estimate of the risk difference, and the horizontal bars represent its 95% confidence interval.
Base line characteristics, clinical presentation upon admission, and treatments received between waves
The differences in baseline characteristics (demographics and comorbidities), clinical presentation upon admission, and treatments received between waves were analyzed (Table 1). There were some differences in demographics in second-wave patients, including older age (second wave: 82.0 vs first wave: 80.8 years), a greater proportion of women (second wave: 48.2% vs first wave: 45.2%), a higher proportion of patients with hypertension (second wave: 73.7% vs first wave: 71.3%) and diabetes (second wave: 30.9% vs first wave: 26.3%), and a slightly higher degree of comorbidity (Charlson Comorbidity Index in the second wave: 5.7 vs first wave: 5.4). The clinical manifestations were also slightly different. Laboratory results showed some differences: blood glucose and creatinine values were higher in patients admitted in the second wave whereas hemoglobin was lower. A high-risk inflammatory pattern was more frequent in the first wave. In the second wave, there was greater use of corticosteroids (79.3% vs 39.5%) and remdesivir (12.6% vs 0.4%). Some of these aforementioned variations could be considered protective (e.g., more women, a lower-risk inflammatory pattern) whereas others (higher age, more diabetes, higher creatinine levels) would suggest higher risk of mortality.
Clinical differences in patients ≥ 70 years hospitalized for COVID-19 by survival status
A univariate analysis of mortality was performed. Almost all variables were statistically associated with mortality, denoting the large sample size. Table 2 shows data on demographics, clinical manifestations, laboratory findings, and treatments received. Although some of the associations were strong, the effects were often small.
The variables and interactions included in the maximal logistic regression model estimated are shown in Table 3.
The odds ratios and risk ratios of mortality of being admitted in the second wave versus the first one for the four different combinations of interaction covariates values are shown in Table 4. The protective effect of being admitted during the second wave of COVID-19 is highest for patients without severe dependence who are not treated with corticosteroids, and it diminishes when either of these circumstances is present, becoming neutral when both converge.
Discussion
This study confirms a difference in mortality in patients hospitalized for COVID-19 in Spain between the first and the second wave of the pandemic. The lower mortality rate observed in the second wave is due to the lower mortality in patients ≥ 70 years; no differences in mortality were observed among younger subjects. To our knowledge, this is a novel finding that has not been previously described.
This reduced mortality rate found in older patients hospitalized during the second wave of the COVID-19 pandemic compared to the first wave could be due to some unmeasured or unknown confounders which may be broadly grouped into three categories: differences in the patients, differences in the disease, or differences in treatment and overall management.
The second-wave patients in this study were slightly older, had a higher degree of dependence (as measured by Barthel index), and a greater comorbidity burden. Given that these factors are associated with a worse COVID-19 prognosis, the clinical and epidemiologic differences between patients hospitalized in the first and the second wave20 do not explain the lower mortality observed in the second wave.
Although patients admitted during the second wave were slightly less severe at admission, after adjustments in the multivariate analysis, admission during the second wave remained an independent protective factor. In the second wave, the use of treatments that have been shown to reduce COVID-19 mortality increased, namely corticosteroids21, tocilizumab22,23, and remdesivir24. However, the lower mortality in the second wave was unchanged after adjusting for the use of these therapies.
Our results suggest that there may be some factor (or, more probably, combination of factors), associated with hospitalization that influences mortality and changed between the waves. Some potential candidates are changes in the overall management of patients, improvements in clinical expertise, and a lesser degree of hospital overload (Fig. 2).
Several characteristics of patients, differences in COVID-19 severity and management could confound the estimation of mortality between waves. After adjusting for these factors, differences in the outcome could be explained by unmeasured patient characteristics and COVID-19 severity factors, or uncontrolled COVID-19 management.
Interestingly, the analysis of the interactions between severe dependency and systemic corticosteroid treatment with the hospital admission wave has allowed us to discover that the protective effect of the second wave on mortality is highest when both factors are absent, somewhat reduced when either of them is present, and neutral when both are present. It is likely, then, that the factors, largely unknown, that explain an average protective effect of the second wave, may not succeed in improving the prognosis of the most fragile and severe patients, such as those requiring corticosteroid treatment.
We have learned that there are a lot of “intangibles” that influence the prognosis of COVID-19 hospitalization. Quick identification of respiratory failure, thromboprophylaxis and early mobilization, an adequate state of hydration, proper management of stress hyperglycemia, nutritional support, physical rehabilitation, and more have become the new standard of care and are potential uncontrolled factors that could explain the better prognosis in the second wave. Most of these factors will have a greater impact on the older people, as they are frailer and thus prone to physical deconditioning, dehydration, or confusional states.
Another possibility is that greater clinical expertise led to improved prognosis. Indeed, in the USA, a progressive decline in COVID-19-related mortality was described after the passage of just a few months9.
Healthcare system overload could be an important driver of mortality in the COVID-19 pandemic25,26,27. The first wave in Spain was explosive and overwhelmed hospitals in some areas. For instance, in Madrid, COVID-19 occupancy reached nearly 300% of the nominal ICU capacity and nearly 105% of the general ward capacity28, paralyzing non-emergency surgical procedures. On the contrary, the second wave has been less dramatic, leading to a smaller impact on hospital occupancy and healthcare activity. It may well be that the lower mortality in the second wave is mainly a reflection of less healthcare system overload. As our study does not include data on the true workload borne by the hospitals, this notion remains a hypothesis.
In extreme cases, healthcare system overload leads to shortages, which can also have a greater effect on the older persons due to implementation of triage criteria. If it were confirmed that healthcare system overload causes greater mortality in the older persons, it would be a moral imperative for us as a society to quickly adopt robust preventative measures as soon as another wave is upon us and there is risk of healthcare system overload. Our registry cannot answer this crucial question, as we lack data on hospital or ICU patient loads at the time of the patients’ admissions.
We recognize several limitations in our study. The large number of researchers involved and/or variability in the availability of data from each hospital could have led to information bias. Selection bias could have been introduced given the voluntary participation of each center. A potential source of uncontrolled confounding factors is the severity of underlying conditions and overall frailty of patients. The lower mortality in the second wave could also be explained by a “harvesting effect” that may be present if the most severely ill patients had already died in the first wave, though patients admitted during the second wave were older and had more dementia and comorbidities. However, we did not analyze frailty, a prognostic factor that is more potent than dependence or age in older patients20.
In terms of limitations regarding treatment-related variables, the effect of remdesivir and tocilizumab on mortality are strongly time-dependent with a narrow window of opportunity and both tocilizumab and corticosteroids are indicated for a worsening respiratory or inflammatory condition. Our registry includes data on the timing of the drug initiation but does not include clinical and laboratory findings at that moment, so it is not possible to evaluate the exact effect of the drugs. The deleterious effect of corticosteroids or tocilizumab in our multivariate analysis should be interpreted as a marker of the patient’s worsening condition.
The strengths of this study include its multicenter, nationwide design as well as the large number of patients included, which provides strong statistical power. The consecutive inclusion of patients in each center limits selection bias.
In conclusion, mortality in the older patients hospitalized in Spain with COVID-19 has been significantly lower in the second wave even after adjusting for baseline clinical condition, disease severity upon admission, and pharmacological treatment with proven benefits in treating COVID-19, except in severely dependent persons in need of corticosteroid treatment. Our results suggest that this reduction of mortality could be related to a better standard of care, improvements in clinical expertise, less healthcare system overload, or a combination of these three factors, though other unknown confounding factors cannot be ruled out.
Methods
Study design
This is a retrospective cohort study comparing the first and second waves of the COVID-19 epidemic in Spain. The first wave was defined as the period between January 1 and July 7, 2020. The second wave was defined as the period between July 8, 2020 and December 26, 2020, before SARS-CoV-2 vaccination was available.
The final weeks of the first wave and the initial weeks of the second one thus defined periods with a low incidence of COVID-19 and few hospital admissions. However, this cut-off point reflects the transition from the greater healthcare system overload which occurred in the initial months to the lesser healthcare system overload of the later months.
Registry design
The SEMI-COVID-19 Registry is an ongoing, nationwide, retrospective cohort launched in March 2020 that comprises most consecutive patients hospitalized in Spain who are discharged with confirmed COVID-19 disease. It has become one of the largest repositories of COVID-19 patient data and includes more than 20,000 patients to date. Its characteristics have been thoroughly described elsewhere6.
Inclusion criteria for the registry were age ≥ 18 years and first hospital discharge with a confirmed diagnosis of COVID-19. Exclusion criteria were subsequent admissions of the same patient and denial or withdrawal of informed consent.
Consecutive patients who required hospital admission and who had SARS-CoV-2 infection confirmed by a positive result on real-time polymerase chain reaction (RT-PCR) testing of a nasopharyngeal, bronchoalveolar lavage, or sputum sample and who provided verbal consent were included in the registry. With the advent of the second wave, the inclusion criteria were expanded with two modifications: antigen testing was accepted as a method for confirming diagnosis and reinfections (> 3 months from the initial infection) of the same patient were accepted for inclusion. From March 23, 2020, to December 26, 2021, a total of 22,494 patients from 126 hospitals throughout the country were included in the registry.
Patients were treated at their attending physician’s discretion according to local protocols and clinical judgment. Patients included in open-label clinical trials could be included in the registry provided that all information about treatment was available. Due to its observational nature, the registry caused no inconvenience to the patients included.
Data collection
Clinical investigators all over the country collected data from medical records using a standardized online data capture system (DCS). The DCS includes both a database manager and the set of procedures for the verification of data. Patient identifiable data are dissociated and pseudonymized using an alphanumeric sequence and each researcher keeps a protected registry (patient log) for the purpose of data verification and quality control. The database platform is hosted in a secure server and both the database and each client–server transfer are encrypted. The pseudonymization system allows for safeguarding patient privacy while also complying with ethical considerations and data protection regulations.
Data on more than 300 variables are collected retrospectively after patient discharge and grouped under various headings: inclusion criteria, epidemiological data, RT-PCR and serology data, prior comorbidities and medication history, findings (symptoms and physical examination) at admission, laboratory (blood gases, metabolic panel, complete blood count, coagulation) and diagnostic imaging tests at admission, additional data at seven days after admission or at admission to the intensive care unit, pharmacological treatment (antiviral drugs, immunomodulators, antibiotics) and ventilatory support during the hospitalization, complications during the hospitalization, and progress after discharge and/or 30 days from diagnosis. The variables in the registry have previously been described6.
A number of secondary variables were calculated from the primary variables in the registry. Some qualitative variables were classified into binary categories whereas some quantitative variables were categorized as normal or abnormal; age was categorized into decades. Arterial stiffness was defined as a pulse pressure greater than or equal to 60 mmHg29. Blood glucose levels were categorized into three groups according to standard glycemic targets in hospitalized patients: < 140 mg/dl, 140–180 mg/dl, and > 180 mg/dl30. The risk categories based on the pattern of inflammation used in this study were a modified version of risk categories recently reported in another work from the SEMI-COVID-19 Registry31. The low-risk category was defined as lactate dehydrogenase (LDH), C-reactive protein (CRP), and D-dimer (DD) values in the first tercile and lymphocyte count in the third tercile. The high-risk category was defined as any LDH, CRP, or DD values in the third tercile or lymphocyte count in the first tercile. The moderate-risk category was defined as patients who did not meet the criteria of the low- or high-risk categories.
Statistical analysis
In a descriptive analysis, we compared epidemiological data, demographics, signs and symptoms on admission, comorbidities, laboratory results, chest x-ray findings, treatment received, and clinical outcomes. Continuous variables were expressed as mean and standard deviation or median and interquartile range (IQR), according to distribution assessed by the Shapiro–Wilk test and standardized normal probability plots. Categorical variables were expressed as frequencies and percentages. Differences between groups were compared using Student’s t-test or the Mann–Whitney U test for continuous variables and the likelihood-ratio chi-square test for categorical variables.
A univariate analysis was performed to explore possible risk factors for all-cause death during admission or the next 30 days from discharge and variables associated with the exposure (pandemic wave) using binomial logistic regressions. The variables were chosen from an array of clinical and laboratory findings, previous comorbidities, and treatments received according to local protocols. Due to the large sample size, almost all variables showed significant differences in the comparisons between exposure and outcome groups in the univariate analysis.
We created a logistic regression model to assess the effect of being admitted during the first or second wave on all-cause mortality risk. We selected a series of predictors associated with the exposure (pandemic wave) and the outcome (mortality) as potential confounding factors. The selection criteria also took theoretical arguments or findings from other studies into consideration in order to adjust for factors that could explain a potential difference in the risk of death between the two waves.
The admitting variables that were ultimately included as possible confounders of the wave effect were age (categorized into decades from 70 years), sex (reference: male), age-adjusted Charlson Comorbidity Index (reference: moderate comorbidity), degree of dependence (reference: none or mild dependence), hypertension, arterial stiffness (pulse pressure ≥ 60 mmHg), clouding of consciousness, tachypnea, oxygen saturation/FiO2 ratio (%), blood glucose level categories, risk category based on the pattern of inflammation, and bilateral pneumonia as well as tocilizumab, remdesivir, or corticosteroid therapy during hospitalization.
In addition, first-order interactions between the waves and all potential confounding factors were included in the initial model. Multicollinearity was detected for several terms of interaction, and they were removed from the model. A chunk test for the rest of interaction terms did show statistical significance (p < 0.001), so individual likelihood ratio tests were performed for every one of them. Three interactions with the variable "Wave" remained statistically significant: severe dependency, corticosteroid treatment, and ventilatory support, which has three different categories. In order to achieve an interpretable estimation and reduce the number of combinations for which to calculate the wave effect on mortality, we decided to omit the interaction of the wave with ventilatory support. So, the final logistic regression model included all the confusion terms and the interactions of Wave with Severe dependence and Systemic corticosteroid therapy. We did not conduct variable selection once the model was estimated, as this maximal model is the best fit for calculating the wave's effect on mortality. Adjusted odds ratios and risk ratios were estimated for each combination of the values of interaction terms. Adjusted risk ratios were calculated with delta-method standard errors for the wave covariate. All analyses were conducted using Stata version 18.0 (StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC).
Ethical considerations
The SEMI-COVID-19 Registry was approved by the Provincial Research Ethics Committee of Málaga (Spain) on March 27, 2020 (Ethics Committee code: SEMI-COVID-19 27/03/20). All experimental protocols were approved by Ethic Committee of Infanta Cristina University Hospital, Ethic Committee of Gregorio Marañón University Hospital, Ethic Committee of Costa del Sol Hospital. Marbella, Cabueñes University Hospital, Ethic Committee of Complejo Hospitalario Universitario de Albacete, Ethic Committee of Hospital Universitario La Paz, Ethic Committee of Hospital Royo Villanova, Ethic Committee of Complejo Hospitalario Universitario de Santiago, Ethic Committee of Hospital Universitario Puerta de Hierro, Ethic Committee of Hospital Universitario Doctor Peset, Ethic Committee of Hospital Clínico San Carlos, Ethic Committee of Complejo Asistencial de Segovia, Ethic Committee of Complejo Hospital Universitario de Badajoz, Ethic Committee of Hospital Universitario Miguel Servet, Ethic Committee of Hospital Universitario de la Princesa, Ethic Committee of Hospital Universitario Infanta Sofía, Ethic Committee of Complexo Hospitalario Universitario A Coruña, Ethic Committee of Hospital de Sant Joan Despí Moisès Broggi, Hospital Universitari Sant Joan d'Alacant, and Ethic Committee of 12 de Octubre University Hospital. The processing of personal data strictly complied with Spanish Law 14/2007, of July 3, on Biomedical Research; Regulation (EU) 2016/679 of the European Parliament, and of the Council of April 27, 2016, on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation); and Spanish Organic Law 3/2018, of December 5, on the Protection of Personal Data and the Guarantee of Digital Rights. Informed consent, written or verbal, was obtained from all participants. In the periods of maximum hospital care pressure with high number of cases admitted, a written informed consent was not possible to obtain if overwork left no time to explain informed consent, prepared the written documentation and keep safe it for overwork (March to April 2020, November to December 2020). In these cases, it was noted noted on the medical record that a written informed consent was not possible to obtain, but the patient gave verbal consent, as such procedure was approved by the ethics committees.
All methods were carried out in accordance with relevant guidelines and regulations. The STROBE Statement guidelines32 were followed in the conduct and reporting of the study.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Weekly epidemiological update on COVID-19-15 June 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---15-june-2021 (Accessed 20 June 2021).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395(10229), 1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3 (2020).
Docherty, A. B. et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 369, m1985. https://doi.org/10.1136/bmj.m1985 (2020).
Richardson, S. et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 323(20), 2052–2059. https://doi.org/10.1001/jama.2020.6775 (2020).
Borobia, A. M. et al. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J. Clin. Med. https://doi.org/10.3390/jcm9061733 (2020).
Casas-Rojo, J. M. et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: Results from the SEMI-COVID-19 Registry. Rev. Clin. Esp. 220(8), 480–494. https://doi.org/10.1016/j.rceng.2020.07.003 (2020).
Ramos-Rincon, J.-M. et al. Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain. J. Gerontol. A Biol. Sci. Med. Sci. 76(3), e28–e37. https://doi.org/10.1093/gerona/glaa243 (2020).
Finelli, L. et al. Mortality among US patients hospitalized with SARS-CoV-2 infection in 2020. JAMA Netw. Open. 4(4), e216556. https://doi.org/10.1001/jamanetworkopen.2021.6556 (2021).
Asch, D. A. et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern. Med. 181(4), 471–478. https://doi.org/10.1001/jamainternmed.2020.8193 (2021).
Vahidy, F. S. et al. Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area. JAMA 324(10), 998–1000. https://doi.org/10.1001/jama.2020.15301 (2020).
Docherty, A. B. et al. Changes in in-hospital mortality in the first wave of COVID-19: A multicentre prospective observational cohort study using the WHO Clinical Characterisation Protocol UK. Lancet Respir. Med. S2213–2600(21), 00175–00182. https://doi.org/10.1016/S2213-2600(21)00175-2 (2021).
Fan, G. et al. Decreased Case fatality rate of COVID-19 in the second wave: A study in 53 countries or regions. Transbound Emerg. Dis. https://doi.org/10.1111/tbed.13819 (2020).
James, N., Menzies, M. & Radchenko, P. COVID-19 second wave mortality in Europe and the United States. Chaos 31(3), 031105. https://doi.org/10.1063/5.0041569 (2021).
Nørgaard, S. K. et al. Real-time monitoring shows substantial excess all-cause mortality during second wave of COVID-19 in Europe, October to December 2020. Euro Surveill. https://doi.org/10.2807/1560-7917.ES.2021.26.1.2002023 (2021).
Radovanovic, D. et al. Characteristics and outcomes in hospitalized COVID-19 patients during the first 28 days of the spring and autumn pandemic waves in Milan: An observational prospective study. Respir Med. 178, 106323. https://doi.org/10.1016/j.rmed.2021.106323 (2021).
Borghesi, A. et al. Lombardy, Northern Italy: COVID-19 second wave less severe and deadly than the first? A preliminary investigation. Infect. Dis. 53(5), 370–375. https://doi.org/10.1080/23744235.2021.1884745 (2021).
Salyer, S. J. et al. The first and second waves of the COVID-19 pandemic in Africa: A cross-sectional study. Lancet 397(10281), 1265–1275. https://doi.org/10.1016/S0140-6736(21)00632-2 (2021).
de Souza, F. S. H., Hojo-Souza, N. S., da Silva, C. M. & Guidoni, D. L. Second wave of COVID-19 in Brazil: Younger at higher risk. Eur. J. Epidemiol. 36(4), 441–443. https://doi.org/10.1007/s10654-021-00750-8 (2021).
Iftimie, S. et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. PLoS ONE 16(3), e0248029. https://doi.org/10.1371/journal.pone.0248029 (2021).
Hewitt, J. et al. The effect of frailty on survival in patients with COVID-19 (COPE): A multicentre, European, observational cohort study. Lancet Public Health. 5(8), e444–e451. https://doi.org/10.1016/S2468-2667(20)30146-8 (2020).
RECOVERY Collaborative Group et al. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med. 384(8), 693–704. https://doi.org/10.1056/NEJMoa2021436 (2021).
REMAP-CAP Investigators et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N. Engl. J. Med. 384(16), 1491–1502. https://doi.org/10.1056/NEJMoa2100433 (2021).
RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 397(10285), 1637–1645. https://doi.org/10.1016/S0140-6736(21)00676-0 (2021).
Beigel, J. H. et al. Remdesivir for the treatment of Covid-19—final report. N. Engl. J. Med. 383(19), 1813–1826. https://doi.org/10.1056/NEJMoa2007764 (2020).
Soria, A. et al. The high volume of patients admitted during the SARS-CoV-2 pandemic has an independent harmful impact on in-hospital mortality from COVID-19. PLoS ONE 16(1), e0246170. https://doi.org/10.1371/journal.pone.0246170 (2021).
Ji, Y., Ma, Z., Peppelenbosch, M. P. & Pan, Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob. Health. 8(4), e480. https://doi.org/10.1016/S2214-109X(20)30068-1 (2020).
African COVID-19 Critical Care Outcomes Study (ACCCOS) Investigators. Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): A multicentre, prospective, observational cohort study. Lancet 397(10288), 1885–1894. https://doi.org/10.1016/S0140-6736(21)00441-4 (2021).
Condes, E. & Arribas, J. R. Impact of COVID-19 on Madrid hospital system. Enferm Infecc. Microbiol. Clin. 39(5), 256–257. https://doi.org/10.1016/j.eimc.2020.06.005 (2021).
Rodilla, E. et al. Impact of arterial stiffness on all-cause mortality in patients hospitalized with COVID-19 in Spain. Hypertension 77(3), 856–867. https://doi.org/10.1161/HYPERTENSIONAHA.120.16563 (2020).
Carrasco-Sánchez, F. J. et al. Admission hyperglycaemia as a predictor of mortality in patients hospitalized with COVID-19 regardless of diabetes status: Data from the Spanish SEMI-COVID-19 Registry. Ann. Med. 53(1), 103–116. https://doi.org/10.1080/07853890.2020.1836566 (2021).
Rubio-Rivas, M. et al. Risk categories in COVID-19 based on degrees of inflammation: Data on More than 17,000 patients from the Spanish SEMI-COVID-19 Registry. J. Clin. Med. 10(10), 2214. https://doi.org/10.3390/jcm10102214 (2021).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370(9596), 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X (2007).
Acknowledgements
We gratefully acknowledge all the investigators who participate in the SEMI-COVID-19 Registry (A complete list of the SEMI-COVID-19 Network members is provided at the end of the paper).
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: J.M.C.R., J.M.A.S., J.M.N.C., R.G.H., J.M.R.R., C.L.B. Acquisition of data: M.R.R., M.A.C.G., M.R.F.M., J.L.B.P., F.A.F., C.G.L., P.P.M., S.M.C., Y.T.C., M.M., M.M.B., D.M.M., G.M.G.G., R.G.F., N.G., R.F.M., M.C.S., N.R., J.P.G. and the members of the SEMI-COVID-19 Network. Analysis and interpretation of data: J.M.C.R., J.M.A.S. Drafting of the manuscript: J.M.C.R., J.M.A.S. Critical revision of the manuscript for important intellectual content: J.M.N.C., R.G.H., J.M.R.R., C.L.B., M.R.R., M.AC.G., M.R.F.M., J.L.B.P., F.A.F., C.G.L., P.P.M., S.M.C., Y.T.C., M.M., M.M.B., D.M.M., G.M.G.G., R.G.F., N.G., R.F.M., M.C.S., N.R., J.P.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Casas-Rojo, JM., Antón-Santos, JM., Millán-Núñez-Cortés, J. et al. Mortality reduction in older COVID-19-patients hospitalized in Spain during the second pandemic wave from the SEMI-COVID-19 Registry. Sci Rep 13, 17731 (2023). https://doi.org/10.1038/s41598-023-42735-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42735-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.