Abstract
The eligibility of reperfusion therapy has been expanded to increase the number of patients. However, it remains unclear the reperfusion therapy will be beneficial in stroke patients with various comorbidities. We developed a reperfusion comorbidity index for predicting 6-month mortality in patients with acute stroke receiving reperfusion therapy. The 19 comorbidities included in the Charlson comorbidity index were adopted and modified. We developed a statistical model and it was validated using data from a prospective cohort. Among 1026 patients in the retrospective nationwide reperfusion therapy registry, 845 (82.3%) had at least one comorbidity. As the number of comorbidities increased, the likelihood of mortality within 6 months also increased (p < 0.001). Six out of the 19 comorbidities were included for developing the reperfusion comorbidity index on the basis of the odds ratios in the multivariate logistic regression analysis. This index showed good prediction of 6-month mortality in the retrospective cohort (area under the curve [AUC], 0.747; 95% CI, 0.704–0.790) and in 333 patients in the prospective cohort (AUC, 0.784; 95% CI, 0.709–0.859). Consideration of comorbidities might be helpful for the prediction of the 6-month mortality in patients with acute ischemic stroke who receive reperfusion therapy.
Similar content being viewed by others
Introduction
The eligibility for reperfusion therapy has been expanded to increase the number of patients who would benefit from this treatment1,2. However, the benefit and risk should be considered in screening candidates for reperfusion therapy. Comorbidities are frequently found in patients with stroke and may be associated with patient outcomes, including mortality3,4. In the recent American Heart Association/American Stroke Association guidelines, some recommendations have been made on several individual comorbidities, such as diabetes mellitus, myocardial infarction, other cardiac diseases, systemic malignancy, end-stage renal disease, dementia, and sickle cell disease5. However, the levels of evidence are low. In addition, whether reperfusion therapy is beneficial in stroke patients with various comorbidities remains unclear.
The Charlson comorbidity index (CCI) is widely used in predicting 1-year mortality in various medical conditions and includes 19 comorbidities6. We developed a reperfusion comorbidity index primarily based on the comorbidities included in the CCI in patients with acute ischemic stroke receiving reperfusion therapy. We investigated its predictive ability for mortality within 6 months after reperfusion therapy.
Results
Study population
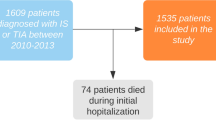
A total of 1026 patients were included in the retrospective cohort. Their median age was 71 (IQR, 62–76) years, and 589 patients (57.4%) were men. The median NIHSS score was 12.5 (IQR, 7–18) (Table 1). Of the 1026 enrolled patients, 845 (82.3%) had at least one comorbidity (median, 2 [IQR, 1–3]) (Fig. 1A). The most common comorbidity was atrial fibrillation (in 523 patients [51%]), followed by diabetes mellitus (in 432 patients [42.4%]), anemia (in 270 patients [26.3%]), and previous stroke (in 207 patients [20.2%]).
The prospective cohort included a total of 333 patients. Their median age was 71 (IQR, 59–78) years, and 208 patients (62.5%) were men. The median NIHSS score was 11 (IQR, 5–16). The demographic characteristics were similar between the retrospective and prospective cohorts, except for the presence/history of hypercholesterolemia, myocardial infarction, and metastatic cancer; current smoking status; initial NIHSS score; and treatment modalities (Supplemental Table 1).
Association of comorbidity with 3-month modified Rankin Scale (mRS)
Among 1026 patients who enrolled in the retrospective cohorts, 3-month mRS was unavailable in 22 patients. Of the 1004 patients, univariable and multivariate analyses showed that poor functional outcome at 3 months (mRS ≥ 3) was associated with age, pre stroke mRS, dementia, and diabetes. When we further included initial NIHSS score, multivariable analysis revealed that age, pre stroke mRS, initial NIHSS score, dementia, diabetes, and anemia were independent predictors of poor functional outcome at 3 months (Supplemental Tables 3 and 4).
Association of comorbidity with 6-month mortality
Among the 1026 patients, 141 (13.7%) died within 6 months. The median number of days until mortality was 12 (IQR, 3–76.5). The direct causes of mortality were cerebral infarction in 59 patients (41.8%), infection in 18 (12.8%), life-threatening hemorrhage, including intracranial hemorrhage in 17 (12.1%), cancer-related mortality in 10 (7.1%), myocardial infarction in 7 (0.5%), cardiac or pulmonary disease in 7 (0.5%), gastrointestinal hemorrhage in 1 (0.1%), and unknown in 22 (15.6%). Ten out of 14 patients (71.4%) with metastatic cancer died within 6 months (Table 1). As the number of comorbidities increased, the likelihood of mortality within 6 months also increased (2.8% in the patients without comorbidity, 7% in those with one comorbidity, 16% in those with two comorbidities, and 26% in those with three or more comorbidities; p < 0.001) (Fig. 1B).
Prognostic model for predicting 6-month mortality
We developed the prognostic model for predicting 6-month mortality using data from the retrospective cohort. For the graphical computation, we created the nomogram. We also developed the smartphone application for fast and easy decision-making in clinical practice (Fig. 2). The prognostic model was validated in the retrospective cohort using data from the prospective cohort.
The reperfusion comorbidity index without considering initial stroke severity
The multivariate logistic regression analysis showed that age, myocardial infarction, congestive heart failure, ulcer disease, diabetes mellitus, anemia, and metastatic cancer were independently associated with 6-month mortality (Table 2). These variables were used to construct the model of the reperfusion comorbidity index for predicting 6-month mortality. The predicted probability of mortality within 6 months without considering initial stroke severity was calculated using the following equation: predicted probability = 1/(1 + exp [− A]), where A = − 5.2999 + 0.0357 × age + 0.6666 × myocardial infarction + 0.6622 × congestive heart failure + 1.0187 × ulcer disease + 1.0201 × diabetes mellitus + 0.5568 × anemia + 2.8128 × metastatic cancer.
The predictive ability of the reperfusion comorbidity index for 6-month mortality showed an AUC of 0.747 (95% CI, 0.704–0.790) In the Hosmer and Lemeshow test, the p value was 0.786, indicating that the model was suitable (Fig. 3A). The calibration plots showed a close approximation to the logistic calibration of the nomogram. ROC comparison for death within 6 months showed that the AUC did not differ between reperfusion comorbidity index (age + 6 comorbidities [myocardial infarction, congestive heart failure, ulcer disease, diabetes mellitus, anemia, and metastatic cancer]) and the original CCI (age + 16 comorbidities) (0.747 [95% CI, 0.704–0.790] vs. 0.758 [95% CI, 0.716–0.800]; p = 0.112) (Fig. 4A). The AUC did not differ between the patients with and without successful recanalization (with recanalization, 0.772 [95% CI, 0.717–0.826] vs. without recanalization, 0.729 [95% CI, 0.634–0.824]; p = 0.439) (Fig. 4B).
Internal validation (A) and external validation (B). The predictive ability of the reperfusion comorbidity index for 6-month mortality showed an area under the curve (AUC) of 0.747 (95% CI, 0.704–0.790) in retrospective cohort (A). In the prospective cohort, the predictive ability of the reperfusion comorbidity index was AUC of 0.784 (95% CI, 0.709–0.859) (B).
Receiver-operating characteristic curve (ROC) comparison death within 6 months mortality according to two models (A) and achievement of recanalization (B). ROC comparison for death within 6 months showed that the area under the curve (AUC) did `not differ between reperfusion comorbidity index (age + 6 comorbidities [myocardial infarction, congestive heart failure, ulcer disease, diabetes mellitus, anemia, and metastatic cancer]) and the original Charlson comorbidity index model (age + 16 comorbidities) (p = 0.112) (A). ROC curve comparison showed that the AUC did not differ according to recanalization status (p = 0.439) (B).
In the prospective cohort, the predictive ability of the reperfusion comorbidity without considering initial stroke severity showed an AUC of 0.784 (95% CI, 0.709–0.859). In the Hosmer and Lemeshow test, the p value was 0.140, indicating that the model was suitable (Fig. 3B).
The reperfusion comorbidity index considering initial stroke severity
The multivariate logistic regression analysis showed that age, initial NIHSS score, ulcer disease, diabetes mellitus, anemia, and metastatic cancer were independently associated with 6-month mortality (Supplemental Table 5). The predicted probability of mortality within 6 months with considering initial stroke severity was calculated using the following equation: predicted probability = 1/(1 + exp [− A]), where A = − 6.2807 + 0.0307 × age + 0.1019 × NIHSS score + 0.8817 × ulcer disease + 0.571 × anemia + 0.9953 × diabetes mellitus + 2.4194 × metastatic cancer. ROC comparison for death within 6 months showed that the AUC did not differ between the reperfusion comorbidity index considering initial stroke severity (age, NIHSS score + 4 comorbidities [ulcer disease, diabetes mellitus, anemia, and metastatic cancer]) and the original CCI (age, NIHSS score + 16 comorbidities) (0.781 [95% CI, 0.738–0.824] vs. 0.792 [95% CI, 0.751–0.832]; p = 0.120) (Supplemental Fig. 1A).
In the prospective cohort, the predictive ability of the reperfusion comorbidity index considering initial stroke severity showed an area under the curve AUC of 0.821 (95% CI, 0.759–0.884). In the Hosmer and Lemeshow test, the p value was 0.098, indicating that the model was suitable (Supplemental Fig. 1B).
Discussion
In this study, we found that the patients who received reperfusion therapy frequently had comorbidities. Over 80% of them had one or more comorbidities. Mortality within 6 months was significantly associated with the number of comorbidities. In a previous study, the comorbidity burden was a strong prognostic factor for both short- and long-term mortalities in patients with stroke4. Comorbidities are closely related with each other and worsen the prognosis beyond that expected through the independent effects of each comorbid condition4. Comorbidities may also influence the clinical outcomes of stroke in terms of the diagnostic process, treatment effects, complication rates, and rehabilitation4,7.
We found that myocardial infarction, congestive heart failure, ulcer disease, diabetes mellitus, anemia, and metastatic cancer were independent predictors of mortality within 6 months. These comorbidities are known to be associated with an increased risk of mortality. Acute myocardial infarction complicating stroke accounts for 20% of in-hospital mortality cases. In-hospital mortality is three-fold higher in patients with stroke and acute myocardial infarction than in those without the latter8,9. Patients with stroke and congestive heart failure showed higher risks of mortality at 30 days (24.5%) and at 1 year (44.3%)10,11. Peptic ulcer disease was an independent risk factor for ischemic stroke and mortality12. Almost 12% of patients with peptic ulcer disease died within 1 year, and the main causes of mortality were cardiovascular disease and malignancy13. Admission blood glucose level and history of diabetes mellitus are strong predictors of poor outcomes14,15,16. Anemia on admission was also associated with an increased risk of mortality in ischemic stroke17. Cancer is unquestionably associated with the risk of mortality14,18. The presence of metastasis is particularly associated with the short-term risk of mortality. Approximately two-thirds of patients with stroke and metastatic cancer died within 6 months after stroke19.
There were slight differences of comorbidities between prediction of 6-month mortality and that of functional outcomes as 3 months. While metastatic cancer was a strong prognostic indicator for 6-month mortality, it was not associated with poor functional outcomes at 3 months. In contrast, dementia was associated with poor functional outcomes at 3 months, while it was not associated with 6-month mortality.
Herein, we included comorbidities based on the CCI. The CCI was developed as a prognostic indicator in patients with a variety of conditions admitted to a general medical service6. It has been also proven to be a valid parameter for predicting mortality within 1 year and functional outcomes in patients with stroke3,4. Patients with severe comorbidities were more likely to die during hospitalization20. We slightly modified the CCI by removing or replacing some comorbidities considering that our study population consisted of patients with acute stroke. We also examined mortality within 6 months because we wanted to investigate the role of the comorbidity index as a parameter for selecting patients for reperfusion therapy. The 6-month survival was suggested in the guidelines as a criterion for alteplase treatment in patients with stroke and systemic malignancy. This study showed that our comorbidity index model may be useful for predicting mortality within 6 months in patients with acute stroke who are potential candidates for reperfusion therapy.
We developed an additional model that includes NIHSS score to comorbidities because NIHSS is routinely determined and a strong prognostic factor in acute stroke. For the model, 6 or 4 (when including NIHSS score) out of the 19 comorbidities were included on the basis of the odds ratios in the multivariate logistic regression analysis. A simple prognostic tool should be used for screening candidates of reperfusion therapy in busy emergency rooms. Obtaining information on many individual comorbidities, such as those included in the CCI, is impractical in emergent conditions in relation to reperfusion therapy. The predictability of 6-month mortality of this models was similar to that of the original CCI model. Consideration of just 6 or 4 comorbidities instead of full comorbidities in the original CCI may be enough to predict mortality within 6 months in patients receiving reperfusion therapy. We also developed a nomogram and a smartphone application, which can be used easily and rapidly in busy emergency rooms21.
Many index scores for reperfusion therapy to predict stroke outcomes have already been proposed. For examples, those include the Pittsburgh Response to Endovascular Therapy (PRE) score22, the Stroke Prognostication Using Age and National Institutes of Health Stroke Scale (SPAN) index23, the Totaled Health Risks in Vascular Events (THRIVE) score24, the Houston Intra-Arterial Therapy (HIAT) score25, and the HIAT2 score26. We summarize a table of each scoring system and compared to our reperfusion comorbidity index (Supplemental table 6). The AUC value of our reperfusion comorbidity index was compatible with those of other scoring systems. Our comorbidity index is different from others in that it can be calculated before reperfusion therapy without further imaging analysis such as the Alberta stroke program early CT score (ASPECTS).
There are some limitations in this study. First, the study population was obtained from a nationwide registry, but in a single country with a single ethnicity. Comorbidities may be different among countries and ethnicities. Therefore, our model should be validated in other cohorts. Second, although a relatively large number of patients were included in this study, some comorbidities were not included in the final predictive model because of their very low prevalence. However, they may influence the outcomes. Although almost all necessary information on comorbidities were obtainable by thorough medical review, particularly in the prospective cohort. There still might be some comorbidities that were unobtainable due to various reasons. Third, we did not include some factors associated with the outcomes of the patients receiving reperfusion therapy for the predictive model (e.g. achievement of recanalization, infarction volume, and complication after reperfusion therapy, such as intracerebral hemorrhage). We wanted to develop a model predicting 6-month mortality, which can be available before reperfusion therapy. Finally, our comorbidity index provides probability of mortality within 6 months to guide and help for decision making of reperfusion therapy. However, quality of life is also very important. The decision regarding reperfusion therapy should be individualized and further research is required.
In conclusion, we developed and validated our simple reperfusion comorbidity index to determine the probability of mortality within 6 months using a large actual-clinical setting multicenter cohort in stroke patients receiving reperfusion therapy. This model may be helpful for prediction of 6-month mortality regarding reperfusion therapy in patients with acute ischemic stroke.
Methods
Patients
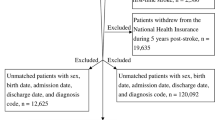
We analyzed data from the SElection CRiteria in Endovascular thrombectomy and Thrombolytic therapy (SECRET) registry. This nationwide registry included consecutive patients with hyperacute ischemic stroke who received intravenous thrombolysis or endovascular thrombectomy. The SECRET registry aimed at exploring the patient selection criteria for reperfusion therapy, especially in relation to clots, core, collaterals, and comorbidities. It included a retrospective cohort and a prospective cohort. The retrospective cohort included 1026 patients from 15 hospitals who received treatment between January 2012 and December 2015. The prospective cohort included 333 patients from 13 hospitals who received treatment between November 2016 and December 2017.
The SECRET registry collected the following data: (1) demographic and clinical data, (2) information on reperfusion therapy, (3) comorbidities, and (4) imaging data. We determined the modified Rankin scale score at 90 days, mortality within 6 months, and the cause of death. Recanalization was assessed using the modified treatment in cerebral infarction score (mTICI). Successful recanalization was defined as mTICI 2b or 3. Symptomatic intracerebral hemorrhage was defined in accordance with the European Cooperative Acute Stroke Study 3 criteria2.
Comorbidities
We determined the presence of comorbidities based on the CCI, which is widely used to predict 1-year mortality3,27. In this study, we modified the CCI, considering patients with stroke as the study population. We omitted paralysis from the original CCI because it is a common symptom or sign of stroke; conversely, we added anemia17, atrial fibrillation28, and depression29 as comorbidities, as they are common and are known to be associated with patient outcomes. Further, we merged diabetes mellitus with and without end-organ damage as diabetes mellitus. Finally, 19 comorbidities were included: myocardial infarction, congestive heart failure, peripheral vascular disease, previous stroke, atrial fibrillation, dementia, depression, chronic pulmonary disease, ulcer disease, mild liver disease, moderate or severe renal disease, connective tissue disease or rheumatic disease, diabetes mellitus, anemia, acquired immune deficiency syndrome, non-metastatic solid tumor, leukemia, lymphoma, and metastatic cancer.
We collected full information on the 19 comorbidities after completion of the reperfusion therapy via history taking and the thorough review of medical records at each study hospital. Neurologists or trained research assistants (nurses) determined the presence of comorbidities according to the definition of a comorbidity (Supplemental material). The number of comorbidities was categorized as 0, 1, 2, or ≥ 34.
Statistical analysis
Data were expressed as means ± SDs, medians and interquartile ranges (IQRs), or frequencies (percentages), as appropriate. Variables were tested for normality using the Kolmogorov–Smirnov test. Differences between the groups were compared using an independent sample t-test or the Mann–Whitney U-test for continuous variables and the chi-square test for categorical variables.
We developed a statistical model to predict 6-month mortality using univariate and multivariate logistic regression analyses with backward (Wald) selection of predictors in the retrospective cohort (the reperfusion comorbidity index). A multivariate analysis was performed using all variables with p values of < 0.05 in the univariate analysis. Comorbidities including leukemia, lymphoma, AIDS with a low prevalence (n < 5) were excluded in the multivariate analysis model. Therefore, 16 comorbidities were analyzed. We also developed another statistical model that added the National Institutes of Health Stroke Scale (NIHSS) score to comorbidities. The models were validated using data from a prospective cohort.
We determined the area under the receiver-operating characteristic curve (ROC) to predict 6-month mortality. The Hosmer and Lemeshow goodness-of-fit test was used to assess the acceptability of the predictive models. This test also determined how well the nomogram was calibrated. Close approximation between the observed and predicted probabilities demonstrated good calibration and confirmed the exportability of the model. We compared the predictability of the reperfusion comorbidity index with that of the original CCI. We also compared the AUC between the patients with recanalization and those without successful recanalization.
The nomogram for predicting 6-month mortality was constructed on the basis of the multivariate models with data from the retrospective cohort. Validation was performed using the prospective cohort. We also developed iPhone and android smartphone applications. The applications calculated the probability of 6-month mortality upon selection of comorbidities.
All p values were two-sided. p values of < 0.05 were considered significant. Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and R package version 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
Standard protocol approval, registration, and patient consent
The study is registered to Clinicaltrials.gov (NCT02964052). The study and registry were approved by the institutional review board (Yonsei University College of Medicine, 4-2015-1196). All methods were performed in accordance with the relevant guidelines and regulations. For the prospectively enrolled patients, written informed consent was obtained from the patients themselves or their next of kin.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Powers, W. J. et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46, 3020–3035 (2015).
Hacke, W. et al. Thrombolysis with alteplase 3 to 45 hours after acute ischemic stroke. N. Engl J. Med. 359, 1317–1329 (2008).
Goldstein, L. B., Samsa, G. P., Matchar, D. B. & Horner, R. D. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke 35, 1941–1945 (2004).
Schmidt, M., Jacobsen, J. B., Johnsen, S. P., Botker, H. E. & Sorensen, H. T. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology 82, 340–350 (2014).
Powers, W. J. et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49, e46–e110 (2018).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40, 373–383 (1987).
Tessier, A., Finch, L., Daskalopoulou, S. S. & Mayo, N. E. Validation of the Charlson comorbidity index for predicting functional outcome of stroke. Arch. Phys. Med. Rehabil. 89, 1276–1283 (2008).
Alqahtani, F. et al. Incidence and outcomes of myocardial infarction in patients admitted with acute ischemic stroke. Stroke 48, 2931–2938 (2017).
Seifi, A. et al. The incidence and risk factors of associated acute myocardial infarction (AMI) in acute cerebral ischemic (ACI) events in the United States. PLoS ONE 9, e105785 (2014).
Pongmoragot, J. et al. Stroke and heart failure: Clinical features, access to care, and outcomes. J. Stroke Cerebrovasc. Dis. 25, 1048–1056 (2016).
Kim, W. & Kim, E. J. Heart failure as a risk factor for stroke. J. Stroke 20, 33–45 (2018).
Cheng, T.-J. et al. The association between peptic ulcer disease and ischemic stroke. Medicine (Baltimore) 95, e3797 (2016).
Malmi, H., Kautiainen, H., Virta, L. J. & Farkkila, M. A. Increased short- and long-term mortality in 8146 hospitalised peptic ulcer patients. Aliment Pharmacol. Ther. 44, 234–245 (2016).
Saposnik, G. et al. The iScore predicts effectiveness of thrombolytic therapy for acute ischemic stroke. Stroke 43, 1315–1322 (2012).
Strbian, D. et al. Predicting outcome of IV thrombolysis-treated ischemic stroke patients: The DRAGON score. Neurology 78, 427–432 (2012).
Ntaios, G. et al. An integer-based score to predict functional outcome in acute ischemic stroke: The ASTRAL score. Neurology 78, 1916–1922 (2012).
Barlas, R. S. et al. Impact of hemoglobin levels and anemia on mortality in acute stroke: Analysis of UK regional registry data, systematic review, and meta-analysis. J. Am. Heart Assoc. 5, e003019 (2016).
Lee, M. J. et al. Hypercoagulability and mortality of patients with stroke and active cancer: The OASIS-CANCER Study. J. Stroke 19, 77–87 (2017).
Yoo, J., Nam, H. S., Kim, Y. D., Lee, H. S. & Heo, J. H. Short-term outcome of ischemic stroke patients with systemic malignancy. Stroke 50, 507–511 (2019).
Ovbiagele, B. Nationwide trends in in-hospital mortality among patients with stroke. Stroke 41, 1748–1754 (2010).
Cappellari, M. et al. IER-START nomogram for prediction of three-month unfavorable outcome after thrombectomy for stroke. Int. J. Stroke 15, 412–420 (2020).
Rangaraju, S. et al. Pittsburgh response to endovascular therapy (PRE) score: Optimizing patient selection for endovascular therapy for large vessel occlusion strokes. J. Neurointerv. Surg. 7, 783–788 (2015).
Saposnik, G., Guzik, A. K., Reeves, M., Ovbiagele, B. & Johnston, S. C. Stroke prognostication using age and NIH stroke scale: SPAN-100. Neurology 80, 21–28 (2013).
Flint, A. C., Cullen, S. P., Faigeles, B. S. & Rao, V. A. Predicting long-term outcome after endovascular stroke treatment: The totaled health risks in vascular events score. AJNR Am. J. Neuroradiol. 31, 1192–1196 (2010).
Hallevi, H. et al. Identifying patients at high risk for poor outcome after intra-arterial therapy for acute ischemic stroke. Stroke 40, 1780–1785 (2009).
Sarraj, A. et al. Optimizing prediction scores for poor outcome after intra-arterial therapy in anterior circulation acute ischemic stroke. Stroke 44, 3324–3330 (2013).
Bushnell, C. D., Lee, J., Duncan, P. W., Newby, L. K. & Goldstein, L. B. Impact of comorbidities on ischemic stroke outcomes in women. Stroke 39, 2138–2140 (2008).
Kernan, W. N. et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 2160–2236 (2014).
Towfighi, A. et al. Poststroke depression: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 48, e30–e43 (2017).
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (Grant number : HI19C0481, HC19C0028).
Author information
Authors and Affiliations
Contributions
H.S.N., Y.D.K., J.Y., and J.H.H. designed the study. H.S.N and H.S.L. performed the statistical analyses. H.S.N., Y.D.K., J.Y., H.P., B.M.K., O.Y.B., H.C.K., E.H., D.J.K., J.H., M.K., J.K.C., K.-Y.L., D.H.S., H.-Y.C., S.-I.S., J.-H.H., J.Y.L., J.-H.B., G.S.K., W.-K.S., J.-W.C., S.H.K., T.-J.S., S.W.H., J.H.P., J.K., Y.H.J., H.-J.C., S.H.A., S.I.L., K.-D.S., J.H.H. collected, assembled, and interpreted the data. H.S.N and J.H.H wrote the manuscript. All authors contributed to the preparation and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nam, H.S., Kim, Y.D., Yoo, J. et al. Comorbidity index for predicting mortality at 6 months after reperfusion therapy. Sci Rep 11, 5963 (2021). https://doi.org/10.1038/s41598-021-85390-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85390-4
This article is cited by
-
Effectiveness of endovascular treatment for in-hospital stroke vs. community-onset stroke: a propensity score-matched analysis
Journal of Neurology (2024)
-
One-Year Survival of Ischemic Stroke Patients Requiring Mechanical Ventilation
Neurocritical Care (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.