Abstract
Standard treatment of Parkinson’s disease involves the dopaminergic medications. Deep brain stimulation of the subthalamic nucleus (STN-DBS) is an important neurosurgical intervention often used as alternative treatment to drug therapy; however, it can be associated with increase of impulsive behaviors. This descriptive review focused on studies investigating the correlation between Deep brain stimulation of the subthalamic nucleus and impulsivity in Parkinson’s disease patients, arguing, the action’s mechanism and the specific role of the subthalamic nucleus. We searched on PubMed and Web of Science databases and screening references of included studies and review articles for additional citations. From initial 106 studies, only 15 met the search criteria. Parkinson’s Disease patients with and without Deep Brain Stimulation were compared with healthy controls, through 16 different tasks that assessed some aspects of impulsivity. Both Deep brain stimulation of the subthalamic nucleus and medication were associated with impulsive behavior and influenced decision-making processes. Moreover, findings demonstrated that: Impulse Control Disorders (ICDs) occurred soon after surgery, while, in pharmacological treatment, they appeared mainly after the initiation of treatment or the increase in dosage, especially with dopamine agonists. The subthalamic nucleus plays a part in the fronto-striato-thalamic-cortical loops mediating motor, cognitive, and emotional functions: this could explain the role of the Deep Brain Stimulation in behavior modulation in Parkinson’s Disease patients. Indeed, increase impulsivity has been reported also after deep brain stimulation of the subthalamic nucleus independently by dopaminergic medication status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact and implications
Deep brain stimulation of the sub-thalamic nucleus (STN-DBS) is an important neurosurgical intervention that could determine, as well as dopaminergic medication, relevant side effects such as increased impulsivity.
The studies analyzed in this review showed that after the surgical intervention, impulsivity improves independently by dopamination medication status. These findings could help to individuate contrasting data about the role of DBS on impulsivity in PD patients.
Future research should include the study of other factors, such as genetic predisposing, direct effect on limbic part of STN, cognitive outcome or depression scores, and should conduct larger, prospective, controlled trials to better clarify how different subcomponents of impulsivity can be modulated both by dopaminergic drugs and STN-DBS.
Introduction
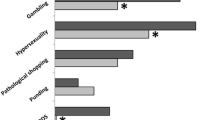
Parkinson’s disease (PD) is a neurodegenerative disorder due to loss of dopaminergic neurons in the substantia nigra pars compacta (SNc) and it is characterized by tremor, rigidity, and bradykinesia [1]. Although classically defined by motor symptoms, it is also associated with non-motor manifestations [2] that have a negative impact on the quality of life of patients [3]. Non-motor symptoms include autonomic and sensory dysfunctions, such as pain and a loss of smell or hyposmia, sleep disorders, cognitive and mood alterations [4,5,6,7]. Standard treatment for PD involves dopamine precursor of levodopa and dopamine agonists (DA) [8]. However, drug therapy is associated with side effects: on–off phenomena due to pharmacokinetics, levodopa-induced dyskinesia (LID), or non-motor symptoms including impulse control disorders (ICDs), such as gambling, hypersexuality, overeating [9]. Particularly, impulsive behaviors are increasingly reported as serious side effects of dopaminergic medication, used in the treatment of PD. Indeed, in the course of dopaminergic treatment patients can show impulsivity characterized by an inability to resist an inappropriate behavior. DA therapy is a major risk factor for the development of ICDs [10]. Impulsivity is characterized by a tendency towards rapid, ill considered, disinhibited choices. It can be broadly divided into:
-
decisional forms, including delay discounting (preference of a small immediate over a larger delayed reward);
-
reduced sensitivity to adverse outcomes (negative prediction errors) during learning;
-
reflection impulsivity (rapid decision-making);
-
risk-taking and response conflict (slowing and errors with competing responses);
-
motor forms, such as response inhibition (inhibition of a response whereby individuals are biased to make a specific response because it is repeated or more frequent) [11].
Deep brain stimulation (DBS) is an adjunctive therapy to reduce some of the symptoms of an advanced stage that responds to levodopa Deep brain stimulation (DBS) is an adjunctive therapy in reducing some of the symptoms of advanced, levodopa-responsive. It improves motor disability by 33%—67%, motor fluctuations by 73%—83%, and dyskinesias caused by levodopa [7, 13,14,15]. DBS uses electrodes connected to a device called ‘implantable pulse generator” that delivers electrical stimuli to a specific brain region. The subthalamic nucleus (STN) is a cerebral area commonly target for DBS in PD [16]. STN has been regarded as a significant structure in the modulation of the activity of output basal ganglia structures; it has an essential role in motor functions, but it has been linked both to reward and to inhibitory control. Bilateral continuous high-frequency stimulation of the STN with typically high frequency (130 to 185 Hz), with pulse widths’ amplitudes of 60 to 120 μsec at voltages ranging from 2.0 to 5.0 V, has been used to treat PD, although it is sometimes related to side effects that could worsen the quality of life, how as reported by Funkiewiez et al. [17]. This study found an increase of cognitive and neuropsychiatric symptoms after STN-DBS, such as impairment in verbal fluency and executive functions, to lack motivation, depression, mania, apathy and explosive-aggressive behavior. In addition, also STN-DBS, as well as drug therapy, has been associated with an increased risk of ICDs [18].
This descriptive review focuses on the studies that investigated the effect of STN-DBS on impulsivity in PD patients and argued its possible mechanisms of action.
Material and methods
Search strategy
Studies were identified in PubMed (2003, year of the first related published article — January 2020) and Web of Science databases (November 2007 — January 2020). The search combined the following terms: ("impulsive behavior" [MeSH Terms] OR ("impulsive" [All Fields] AND "behavior" [All Fields]) OR "impulsive behavior" [All Fields] OR "impulsive" [All Fields]) AND ("deep brain stimulation" [MeSH Terms] OR ("deep" [All Fields] AND "brain" [All Fields] AND "stimulation" [All Fields]) OR "deep brain stimulation" [All Fields]) AND ("parkinson disease" [MeSH Terms] OR ("parkinson" [All Fields] AND "disease" [All Fields]) OR "parkinson disease" [All Fields] OR "parkinsons" [All Fields]). The search terms were identified in the title and abstract. We selected only English texts. After duplicates had been removed, articles were evaluated based on the title, abstract, and text. Studies that examined impulsivity in PD patients were included, after they fulfilled the following criteria:
-
1.
The sample population included PD patients with STN DBS;
-
2.
Studies provided a neuropsychological assessment of impulsivity and neurocognitive performances;
-
3.
Data compared the performance of PD patients on/off stimulation and on/off medication and healthy controls (HC);
-
4.
We excluded studies on PD patient with dementia or affected by other neurological or major psychiatric disorders;
-
5.
Animal studies and published in non-peer reviewed research were excluded;
-
6.
We excluded case studies.
Of 108 studies identified, 15 met the inclusion criteria (Fig. 1). All studies conducted research on PD patients divided into two groups: PD with STN-DBS (a subgroup treated with both L-dopa and DA, ones treated only with L-dopa, and the last without medication treatment) and PD without DBS (three subgroups: PD NO-DBS treated with both L-dopa and DA, PD NO-DBS treated only with L-dopa, and PD NO-DBS without medication treatment). All PD patients fulfilled diagnostic criteria for PD according to the United Kingdom Parkinson Disease Society Brain Bank for Idiopathic PD [19]. Disease severity was rated on the Unified Parkinson Disease Rating Scale motor score and the Hoehn and Yahr score (stages I–III) [20].
The HC groups consisted of volunteers without a history of neurological or psychiatric disorders. All subjects, matched for age and education, had normal or corrected to normal vision.
In these studies, impulsivity was evaluated by 16 different tasks (Table 1). Demographic characteristics of each study’s sample were shown in Table 2.
Results
The role of DBS in ICD is not entirely clear and studies here identified have revealed conflicting results. Indeed, some authors affirmed that hyperdopaminergic manifestations, such as ICDs, could be reduced after DBS, in association with a reduction in the dose of levodopa [35]. These studies argued dopaminergic therapy, particularly DA, could cause the onset of ICDs, [36, 37]. Others authors, instead, reported that DBS is greater involved in increasing ICDs than L-dopa medication [21, 26].
STN-DBS and dopamine replacement in decision-making and impulsive behavior
Many studies have evaluated decision-making process in PD, comparing patients with STN DBS and patients treated pharmacologically. Findings revealed that both STN-DBS and medication were associated with impulsive behavior and both of them influenced decision-making processes in risky situations [21, 25]. According to these data, Djamshidian et al. [36] suggested that DA rather than DBS was responsible for the inability to slow down in high-conflict situations. Moreover, DA combined with L-dopa and STN-DBS would be causing sensitization of mesolimbic dopamine levels resulting in reduced decision threshold in a perceptual decision-making task. However, in a subsequent study, Djamashidian (2014), using the Beads task, had reported contrasting results showing that neither STN-DBS nor L-dopa monotherapy increased impulsive choices in PD patients,. However, this result could be due to a methodological problem related to the low sensitivity of the test chosen to evaluate impulsive behavior. Indeed, in both studies (Djashidian et al. 2013, 2014), the author concluded that all patients treated with L-dopa in combination with DA were more impulsive than all other groups treated with DBS, confirming the hypothesis that it is the pharmacological therapy rather than DBS that causes more impulsivity tendency.
Reference [26] highlighted the role of STN-DBS in the choice on the basis of probabilistic information from multiple stimuli regardless of the ON or OFF pharmacological status. In this study, patients performed the tasks ON or OFF DBS and/or ON or OFF dopaminergic therapy. When dopaminergic therapy was in OFF, memory for probabilistic information was compromised; while in OFF STN-DBS, the decision-making in combined multiple pieces of information was interrupted. Findings demonstrated that both dopamine medication and STN-DBS could influence decision-making processes but acting on different levels within the same task.
The STN-DBS effects on impulsive behavior
Studies about Decision-making studies in ambiguous or risky contexts in on PD patients with DBS, have shown that STN-DBS induces a lowering of the response threshold and a decrease in the level of caution by altering the speed-accuracy trade-off. In addition, stimulation increases rapid response errors and this effect is greater in BDS ON than in BDS OFF [24]. In addition, STN-DBS influences the pathways involved in risk assessment leading to a combination of overestimation of patient performance and increased risk-taking, and preference for competitive environments [23]. In a study assessing willingness to gamble on a fixed (unambiguous) prize, non-surgical PD patients tended to be more risk-averse than HC, whereas DBS patients were more willing to gamble for gains, as well as, losses both ON and OFF stimulation. On “risky” decision-making tasks, DBS patients were more risk-taking than normal, but stimulation might temper this tendency. Moreover, STN-DBS resulted in the performance of the patients to become differentially faster and more erroneous and induced a decrease in the level of caution [38].
Other studies on impulsivity in PD patients mainly focused on motor impulsivity using the stop-signal reaction time (RT) task [27, 28] and Go/NoGo RTs. Motor impulsivity results from insufficient motor or response inhibition. In PD patients, STN-DBS selectively improved inhibitory functions as its electrical stimulation significantly shortened the stop-signal reaction time [27]. Moreover, STN-DBS selectively decreased discriminability when the response was most prepotent [28]. Movement execution resulted faster with STN stimulation than with DBSOFF across different Go probability levels. Furthermore, these studies found that in comparison to HC, both STN-DBS and unoperated PD patients were more prone to making anticipatory errors.
Reference [29] examined more specifically the role of the subthalamic nucleus in reward and inhibitory control through go/no go tasks. The authors evaluated whether the weight gain experienced by PD patients after STN-DBS may be due to an alteration of reward and inhibitory functions. The results showed that body weight increased significantly after STN-DBS since to increased impulsivity and reward sensitivity. As impulsivity and reward sensitivity increased.
The effects of DBS on impulsivity were also investigated by other tasks involving inhibitory control or response selection under conflict. In Simon task, that produced conflict from response impulses in patients with PD and HC, responses were faster and more accurate when relevant (color) and irrelevant (spatial location) features of an imperative stimulus corresponded to the same response, but slower and less accurate when these features signaled conflicting responses [30]. STN-DBS patients were more susceptible to reacting impulsively in situations requiring a speedy decision among highly conflicting response alternatives. Moreover, STN-DBS patients overestimated their own performance assuming an extremely risky gambling behavior assessed by a simple two-choice gambling task due to the modulation of basal-ganglia-cortex circuits by STN-DBS leading to overly competitive behavior [23].
Since it is not yet clear what aspects of PD are actually caused by Basal Ganglia (BG) dysfunction, [34] investigated 13 patients with PD off-medication with bilateral subthalamic deep brain stimulation (DBS) with and without stimulation (DBS ON and DBS OFF, respectively) and 26 HC. All participants performed a task that verifies the relationship between the automatic response impulses and the selection of the direct action to the target. The results showed an improvement in automatic response activation under DBS ON, increasing susceptibility to impulsive responses, and a reduced impact of automatic response activation under DBS OFF. These data seem to support or argue that the BG determines the efficiency of the regulation and transmission of stimulus-driven bottom–up response activation necessary for efficient response selection.
Neuroanatomical correlates of impulsive behavior
Stimulation of the ventromedial STN through its close connection to the nucleus accumbens loop potentially induces ICD [32]. These cerebral areas are crucial in impulse control, motivational processes, and addictive behaviors. In addition, the orbitofrontal and anterior cingulate cortices and the ventral striatum are linked to impaired risk evaluation, which is mediated by DA in PD patients suffering from comorbid ICD. In recent years, magnetic resonance imaging examinations (MRI) focused on the dopaminergic system, have significantly contributed to the knowledge of neurobiological factors for ICDs. In PD patients with ICDs, structural MRI revealed orbitofrontal atrophy [33]. In addition, connectivity dysfunction between the striatal and limbic areas involving the neurocognitive networks has been proposed. In particular, a decreased of cerebral connectivity was found in the central executive network (mediofrontal areas, anterior cingulate and paracingulate cortices), while increased connectivity has been identified in the salience network (limbic-paralimbic network) and in the default mode network (precuneus and posterior cingulate, bilateral and ventromedial cortices) [31].
STN plays a key role in inhibition processes, which permit the suppression of premature actions and to block interference from irrelevant stimuli. Altered decision-making is associated with cognitive impulsivity, which is considered the inability to weigh the consequences of immediate and future events and, consequently, delay gratification [39]. Lesion studies have suggested the ventromedial prefrontal cortex, is the main area involved in this type of impulsivity [40]. A study conducted by van Wouwe et al. [41] reported that STN-DBS ON stimulation improved the reactive inhibition of impulsive actions that interfere with goal-directed behavior. These findings showed that DBS improves reactive inhibitory control, regardless of medication and regardless of whether it concerns chronic or acute Subthalamic Nucleus stimulation. The most important result of this study was that especially the dorsal STN circuitries were crucial for modulating the reactive inhibitory control of motor actions, how the selective stimulation of dorsal and ventral subregions of the Subthalamic Nucleus had indicated.
STN-DBS could improve ICD
Two studies hypothesized that STN DBS selectively improves inhibitory functions [27, 41]. This finding is consistent with the idea that DBS not only shuts off the pathological activity of STN but also imposes a new pattern of activity with beneficial effects. The improvement in the proficiency of inhibitory control would be greatest when stimulating a relatively dorsal STN subregion compared to a relatively ventral STN subregion. Confirmation of this pattern would provide new evidence that dorsal STN circuitries play, direct role in reactive inhibitory motor control processes.
Discussion
Studies on impulsivity in PD patients highlighted conflicting results. DA seems to represent the main risk factor that leads to “reflection impulsivity”. Indeed, ICDs predominantly occurred subsequent to treatment initiation or dosage increase particularly related to the effects of the DA [36, 25]. However, an increase of impulsivity has been reported also after STN-DBS independently by dopaminergic medication status. DBS, indeed, has been described as “releasing the brake” of the STN, that lead to faster responses, particularly in a high-conflict situation, suggesting a diminished ability to hold initial response tendencies in check [42]. STN-DBS patients tend to prefer high-risk options and are (deliberately or not) overconfident [43]. One important characteristic of a decision-making network is inhibition of the prepotent response to each individual stimulus, thus avoiding rapid impulsive behavior that does not weigh up all options. STN-DBS seems to be associate with the inability to slow and integrate evidence before deciding, probably due to interference of stimulation with adjustments of decision thresholds. STN-DBS can raise action impulsivity, increasing response speed and lowering response accuracy (Ballanger et al., 2009). The speed–accuracy trade-off is a property of decision-making that can be controlled by cognitive processing.
Contrasting data suggest that STN-DBS significantly improves the proficiency of reactive inhibitory control [27, 41] and the suppression of irrelevant motor impulses. Selectively stimulating the dorsal as opposed to the ventral STN substructure is responsible for this effect [30]. Probably, the site of stimulation could moderate the improvement of ICD improvement. These suppositions underscore the importance of accurate electrode targeting, contact selection and device programming to reduce postoperative neuropsychiatric impairment. The ability to predict neuropsychiatric symptoms based on subthalamic data may permit anticipation and prevention of these occurrences, improving safety and tolerability [22]. STN-DBS coupled with a large reduction in dopaminergic medication has been shown to reduce pre-existing impulsive behavior, but the onset of new or worsening of existing ICDs in the post-operative period despite the reduction in dopaminergic medications has also been documented.
Conclusion
The etiology and pathogenesis of treatment-induced impulsivity in PD remain unknown [44], though the altered activity of the mesolimbic dopamine system has been suggested to be responsible for the phenomenon, since dopaminergic neurons facilitate the adaptation of behavior according to reward or task demands. Similarly, it is well known that STN plays a part in the fronto-striato-thalamic-cortical loops mediating motor, cognitive, and emotional functions, thus suggesting that DBS may affect the behavior of PD patients, in addition to motor performance. However, literature data showed contrasting data about the role of DBS on impulsivity in PD patients. Several studies have stressed a direct correlation between STN-DBS and impulsive behavior, reporting the worsening or ex novo development of ICDs after surgery, other authors described a significant improvement of impulsivity after surgery. In addition, the studies reviewed involved only a limited number of participants, considering the high incidence of the disease and the sample heterogeneity, and the different tasks used did not permit a comparison between results. Future research should include the study of other factors, such as genetic predisposing, direct effect on the limbic part of STN, cognitive outcome or depression scores, and should conduct larger, prospective, controlled trials to better clarify how different subcomponents of impulsivity can be modulated both by dopaminergic drugs and STN-DBS.
References
Samii A, Nutt JG, Ransom BR (2004) Parkinson’s disease. Lancet 363(9423):1783–1793
Palmeri R, Lo Buono V, Corallo F, Foti M, Di Lorenzo G, Bramanti P, Marino S (2017) Nonmotor symptoms in parkinson disease: a descriptive review on social cognition ability. J Geriatr Psychiatry Neurol 30(2):109–121
Corallo F, De Cola MC, Lo Buono V, Di Lorenzo G, Bramanti P, Marino S (2017) Observational study of quality of life of Parkinson’s patients and their caregivers. Psychogeriatrics 17(2):97–102
Chaudhuri KR, Healy DG, Schapira AH (2006) Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol 5(3):235–245
Tolosa E, Compta Y, Gaig C (2007) The premotor phase of Parkinson’s disease. Parkinsonism relat disord 13:S2–S7
Poewe W (2008) Non-motor symptoms in Parkinson’s disease. Eur J Neurol 15(s1):14–20
Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois BMDS (2015) Research criteria for prodromal Parkinson’s disease. Mov Disord 30(12):1600–1611
Santiago AJ, Factor SA (2003) Levodopa. Neurol dis and therapy 59:381–406
Voon V, Fernagut PO, Wickens J, Baunez C, Rodriguez M, Pavon N (2009) Chronic dopaminergic stimulation in Parkinson’s disease: from dyskinesias to impulse control disorders. Lancet Neurol 8(12):1140–1149
Rossi PJ, De Jesus S, Hess CW, Martinez-Ramirez D, Foote KD, Gunduz A, Okun MS et al (2017) Measures of impulsivity in Parkinson’s disease decrease after DBS in the setting of stable dopamine therapy. Parkinsonism relat disord 44:13–17
Voon V, Napier TC, Frank MJ, Sgambato-Faure V, Grace AA, Rodriguez-Oroz M et al (2017) Impulse control disorders and levodopa-induced dyskinesias in Parkinson’s disease: an update. Lancet Neurol 16(3):238–250
Kumar R, Lozano AM, Kim YJ, Hutchison WD, Sime E, Halket E, Lang AE (1998) Double-blind evaluation of subthalamic nucleus deep brain stimulation in advanced Parkinson’s disease. Neurol 51(3):850–855
Limousin P, Krack P, Pollak P, Benazzouz A, Ardouin C, Hoffmann D, Benabid AL (1998) Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 339(16):1105–1111
Moro E, Scerrati M, Romito LMA, Roselli R, Tonali P, Albanese A (1999) Chronic subthalamic nucleus stimulation reduces medication requirements in Parkinson’s disease. Neurol 53(1):85–85
Houeto JL, Damier P, Bejjani PB, Staedler C, Bonnet AM, Arnulf I et al (2000) Subthalamic stimulation in Parkinson disease: a multidisciplinary approach. Arch Neurol 57(4):461–465
Okun MS (2012) Deep-brain stimulation for Parkinson’s disease. N Engl J Med 367(16):1529–1538
Funkiewiez A, Ardouin C, Caputo E, Krack P, Fraix V, Klinger H et al (2004) Long term effects of bilateral subthalamic nucleus stimulation on cognitive function, mood, and behaviour in Parkinson’s disease. J Neurol Neurosurg Psychiatry 75(6):834–839
Volkmann J, Daniels C, Witt K (2010) Neuropsychiatric effects of subthalamic neurostimulation in Parkinson disease. Nat Rev Neurol 6(9):487
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184
Rabey JM, Korczyn AD (1995) The Hoehn and Yahr rating scale for Parkinson’s disease. In: Instrumental methods and scoring in extrapyramidal disorders. Springer, Berlin, Heidelberg, pp 7–17
Frank MJ, Samanta J, Moustafa AA, Sherman SJ (2007) Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science 318(5854):1309–1312
Mosley PE, Smith D, Coyne T, Silburn P, Breakspear M, Perry A (2018) The site of stimulation moderates neuropsychiatric symptoms after subthalamic deep brain stimulation for Parkinson's disease. Neuroimage Clin 18:996–1006
Florin E, Müller D, Pfeifer J, Barbe MT, Fink GR, Timmermann L (2013) Subthalamic stimulation modulates self-estimation of patients with Parkinson’s disease and induces risk- seeking behaviour. Brain 136(11):3271–3281
Brandt J, Rogerson M, Al-Joudi H, Reckess G, Shpritz B, Umeh CC et al (2015) Betting on DBS: Effects of subthalamic nucleus deep brain stimulation on risk taking and decision making in patients with Parkinson’s disease. Neuropsychology 29(4):622
Boller JK, Barbe MT, Pauls KAM, Reck C, Brand M, Maier F et al (2014) Decision-making under risk is improved by both dopaminergic medication and subthalamic stimulation in Parkinson’s disease. Exp Neurol 254:70–77
Coulthard EJ, Bogacz R, Javed S, Mooney LK, Murphy G, Keeley S, Whone AL (2012) Distinct roles of dopamine and subthalamic nucleus in learning and probabilistic decision making. Brain 135(12):3721–3734
Mirabella G, Iaconelli S, Romanelli P, Modugno N, Lena F, Manfredi M, Cantore G (2012) Deep brain stimulation of subthalamic nuclei affects arm response inhibition in Parkinson’s patients. Cereb Cortex 22(5):1124–1132
Georgiev D, Dirnberger G, Wilkinson L, Limousin P, Jahanshahi M (2016) In Parkinson’s disease on a probabilistic Go/NoGo task deep brain stimulation of the subthalamic nucleus only interferes with withholding of the most prepotent responses. Exp Brain Res 234(4):1133–1143
Aiello M, Eleopra R, Foroni F, Rinaldo S, Rumiati RI (2017) Weight gain after STN-DBS: The role of reward sensitivity and impulsivity. Cortex 92:150–161
Wylie SA, Ridderinkhof KR, Elias WJ, Frysinger RC, Bashore TR, Downs KE et al (2010) Subthalamic nucleus stimulation influences expression and suppression of impulsive behaviour in Parkinson’s disease. Brain 133(12):3611–3624
Tessitore A, Santangelo G, De Micco R, Giordano A, Raimo S, Amboni M et al (2017) Resting-state brain networks in patients with Parkinson’s disease and impulse control disorders. Cortex 94:63–72
Callesen MB, Scheel-Krüger J, Kringelbach ML, Møller A (2013) A systematic review of impulse control disorders in Parkinson’s disease. J Parkinsons Dis 3(2):105–138
Gatto EM, Aldinio V (2019) Impulse Control Disorders in Parkinson’s Disease. A Brief and Comprehensive Review, Front Neurol., p 10
Plessow F, Fischer R, Volkmann J, Schubert T (2014) Subthalamic deep brain stimulation restores automatic response activation and increases susceptibility to impulsive behavior in patients with Parkinson’s disease. Brain Cogn 87:16–21
Bhattacharjee S (2018) Impulse control disorders in Parkinson’s disease: Review of pathophysiology, epidemiology, clinical features, management, and future challenges. Neurol India 2018(66):967–975
Djamshidian A, O’Sullivan SS, Foltynie T, Aviles-Olmos I, Limousin P, Noyce A et al (2013) Dopamine agonists rather than deep brain stimulation cause reflection impulsivity in Parkinson’s disease. J Parkinsons Dis 3(2):139–144
Djamshidian A, O’Sullivan SS, Tomassini A, Foltynie T, Limousin P, Aviles-Olmos I et al (2014) In a rush to decide: deep brain stimulation and dopamine agonist therapy in Parkinson’s disease. J Parkinsons Dis 4(4):579–583
Pote I, Torkamani M, Kefalopoulou ZM, Zrinzo L, Limousin-Dowsey P, Foltynie T et al (2016) Subthalamic nucleus deep brain stimulation induces impulsive action when patients with Parkinson’s disease act under speed pressure. Exp Brain Res 234(7):1837–1848
Harnishfeger KK (1995) The development of cognitive inhibition: theories, definitions, and research evidence. In: Interference and inhibition in cognition, Academic Press, pp 175–204
Bechara A, Damasio H (2002) Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia 40(10):1675–1689
van Wouwe NC, Pallavaram S, Phibbs FT, Martinez-Ramirez D, Neimat JS, Dawant BM et al (2017) Focused stimulation of dorsal subthalamic nucleus improves reactive inhibitory control of action impulses. Neuropsychologia 99:37–47
Frank MJ (2006) Hold your horses: a dynamic computational role for the subthalamic nucleus in decision making. Neural Netw 19(8):1120–1136
Cavanagh JF, Sanguinetti JL, Allen JJ, Sherman SJ, Frank MJ (2014) The subthalamic nucleus contributes to post-error slowing. J Cogn Neurosci 26(11):2637–2644
Kasemsuk C, Oyama G, Hattori N (2017) Management of impulse control disorders with deep brain stimulation: a double-edged sword. J Neurol Sci 374:63–68
Acknowledgements
This work did not receive any financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report no declarations of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lo Buono, V., Lucà Trombetta, M., Palmeri, R. et al. Subthalamic nucleus deep brain stimulation and impulsivity in Parkinson’s disease: a descriptive review. Acta Neurol Belg 121, 837–847 (2021). https://doi.org/10.1007/s13760-021-01684-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-021-01684-4